Vestibular Disorders and
the Cavalier King Charles Spaniel
The vestibular system is a sensory system that coordinates the position of the dog's eyes, neck, trunk, and limbs relative to the position or movement of its head. It enables the dog to maintain its balance and stablize its eyes during movement of its head. The system is located in the vestibulum in the inner ear. It sends signals to the neural structures that control eye movements and to the muscles that keep the dog stable and upright. The system compensates the position of the dog's body for gravity and movement.
The components of the vestibular system are divided into peripheral (relating to the inner ear) and central components (relating to the brain stem). Therefore, vestibular disorders are distinguished between peripheral vestibular disease (PVD) and central vestibular disease.
In a February 2021 article examining the medical records of 239 dogs identified with vestibular symptoms, the cavalier King Charles spaniel was the most common dog diagnosed with this disorder (26 dogs -- 11%).
What It Is
- peripheral vestibular disease (PVD)
- central vestibular disease (CVD)
- idiopathic vestibular syndrome (IVS)
- benign paroxysmal positional vertigo
- inner ear infections/inflammation
- primary secretory otitis media
- cerebellar infarcts (strokes)
- vestibular epilepsy (VE)
- inflammatory brain disease
- nasopharyngeal polyps
- intracranial neoplasia
- ototoxicity
Vestibular syndrome (or dysfunction) is one of a few disorders which may be "idiopathic" (meaning that its cause is not known), or it may be the result of some other disease. Therefore, it is important to try to determine if there is an underlying disease causing the symptoms which constitute vestibular syndrome. Apart from idiopathic vestibular disease, the most common disorders causing vestibular symptoms in cavalier King Charles spaniels are: otitis media and/or otitis interna (or labyrinthitis), primary secretory otitis media (PSOM), cerebrovascular disease (cerebellar infarcts), and inflammatory brain disease (granulomatous meningoencephalomyelitis). Other causes include: nasopharyngeal polyps, intracranial neoplasia, and ototoxicity.
For those causes of vestibular syndrome other than the idiopathic variety, the diagnosis and treatment involve identifying and treating the particular disease causing the symptoms.
RETURN TO TOP
• peripheral vestibular disease (PVD)
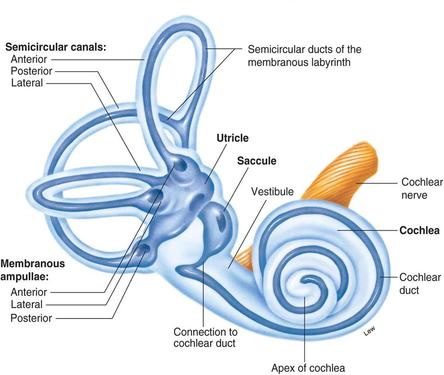
The main peripheral component of the vestibular system is a set of interconnected canals called “the labyrinth” (see drawing below). They contain sensory hair cells which convert physical motion, such as head movements, into neural impulses.
PVD maybe either unilateral (one-sided, affecting one ear) or bilateral.
RETURN TO TOP
• central vestibular disease (CVD)
The central vestibulary system is located within the cerebellum.
RETURN TO TOP
• idiopathic vestibular syndrome (IVS)
Idiopathic vestibular disease is the most common version of
peripheral vestibular disease in older dogs. It therefore also is
referred to as “old dog” or “geriatric” vestibular or even “Idiopathic
Geriatric Vestibulitis”. The onset usually is
sudden, and symptoms typically include:
• A
staggering or rolling gait (ataxia)
• Nystagmus
(uncontrolled movements of the eyes, usually from side to side, or in a
circular pattern)
• Strabismus (inability of the
eyes to aim at the same point in space)
• Head
tilt
•
Falling down
• Vomiting
Usually there is no facial nerve twitching or Horner's syndrome involved.
There is no effective medication to cure this idiopathic version. Nevertheless, improvement of symptoms usually occurs within days or a few weeks, with the nystagmus usually resolving earliest. Most dogs will make a full recovery although some may continue to have a slight head tilt.
In a February 2021 article examining the medical records of 239 dogs identified with vestibular symptoms, 78 dogs (34.2%) were diagnosed with idiopathic vestibular syndrome.
RETURN TO TOP
• benign paroxysmal positional vertigo
 While
many veterinarians insist that idiopathic vestibular disease is, indeed,
"idiopathic" -- meaning that it is a condition that appears to arise
spontaneously or for which the cause is unknown -- it is very likely
that many cases of idiopathic vestibular disease are, in fact, cases of
benign paroxysmal positional vertigo (BPPV). BPPV occurs when microsized
stones or granules -- actually calcium carbonate crystals called
otoconia (right) -- become dislodged from the utricle, which is
one of the inner ear sensory organs. (See the location of the
utricle in the diagram above.)
While
many veterinarians insist that idiopathic vestibular disease is, indeed,
"idiopathic" -- meaning that it is a condition that appears to arise
spontaneously or for which the cause is unknown -- it is very likely
that many cases of idiopathic vestibular disease are, in fact, cases of
benign paroxysmal positional vertigo (BPPV). BPPV occurs when microsized
stones or granules -- actually calcium carbonate crystals called
otoconia (right) -- become dislodged from the utricle, which is
one of the inner ear sensory organs. (See the location of the
utricle in the diagram above.)
These stones are embedded in a viscous fluid membrane which flows back and forth to stimulate a patch of sensory hair cells -- called the macula utricle -- to detect motion and orientation. The hair cells are weighted by the granules and membrane to provide a degree of inertia to enable the utricle to detect linear accelerations and head-tilts. When the head is tilted, gravity pulls on the gelatinous membrane, causing the hair cells to bend.
However, occasionally, one or more of these calcium granules become dislodged from the utricle and flow into one of the semicircular canals which sense the rotation of the head. Once in a canal, they may still move when the head changes position, but their movement can cause a false sense that the head and body are spinning around.
The diagnosis of BPPV is made by the characteristic symptoms and also by observing the nystagmus – the uncontrolled movements of the eyes, usually from side to side, or in a circular pattern. Then the veterinarian will conduct maneuvering tests such as the Dix - Hallpike maneuver and the side-lying maneuver, which involve protocols of postioning and then re-positioning the patient until the signs of nystagmus disappear.
As with idiopathic vestibular disease, BPPV also may resolve itself within a few days without any treatment. It is for this reason that idiopathic vestibular disease actually may be BPPV.
RETURN TO TOP
• inner ear infections and inflammation (otitis media and otitis interna)
Otitis media and otitis interna are the medical terms used by veterinarians to describe an inner – or middle – ear infection (media) or inflammation (interna). They are the most common causes of peripheral vestibular disease in dogs.
Single-sided facial paralysis is the most common sign of a middle ear disorder. A myringotomy (incision of the ear drum) to obtain a sample of the infection material in the ear usually is necessary to determine the appropriate antibiotic to prescribe. Treatment with antibiotics for up to six weeks. If antibiotics are discontinued too soon, the symptoms and infection will recur and can be more difficult to treat. Corticosteroids are usually not required.
In a February 2021 article examining the medical records of 239 dogs identified with vestibular symptoms, 54 dogs (23.7%) were diagnosed with otitis media interna.
RETURN TO TOP
• primary secretory otitis media (PSOM)
Primary secretory otitis media (PSOM) -- also known as "glue ear" or "middle ear effusion" or "otitis media with effusion" (OME) -- has been reported almost exclusively in cavaliers. It consists of a highly viscous mucus plug which fills the dog's middle ear and may cause the tympanic membrane to bulge. The mucus has also been referred to as "hyperintense material". It may result in symptoms of peripheral vestibular syndrome. PSOM is covered extensively as a separate topic here.
In a February 2021 article examining the medical records of 239 dogs identified with vestibular symptoms, 2 dogs (0.8%) were diagnosed with PSOM.
RETURN TO TOP
• cerebellar infarcts (strokes)
Cavaliers appear predisposed to develop cerebellar infarcts, or strokes. The affected dog may be behaving normally one minute, and then in an instant, become unsteady, un-coordinated, nauseous, walk uncontrollably in small circles, or even faint and fall over. The dog may tilt its head, have facial paralysis, lose its vision or control of its bowels, or change its temperament. Some symptoms may progress over the first twelve hours, presumably due to brain swelling, while others may disappear quickly. Most symptoms should begin to lessen within a day or two. All of these symptoms are consistent with central vestibular disorder.
In an August 2015 abstract, UK neurologists report finding cerebellar infarctions in 24 dogs, including 9 cavaliers, displaying ataxia (staggering or rolling gait), hypermetria (voluntary muscular movements tend to overreach their intended goals), head tilt, nystagmus (uncontrolled movements of the eyes), reduced postural reactions (e.g., replacing a foot after being lifted), and decreased menace response (eye blinking in response to an on-coming object). They concluded that cerebellar ischemic strokes should be considered an important differential diagnosis in dogs with acute vestibular signs.
In a February 2021 article examining the medical records of 239 dogs identified with vestibular symptoms, 25 dogs (11%) were diagnosed with ischamic infarcts.
Cerebellar infarcts are covered extensively as a separate topic here.
RETURN TO TOP
• vestibular epilepsy (VE)
Vestibular epilepsy (VE) is described as focal seizures with vestibular disease as the only or main symptom. The signs range from mild disequilibrium to dizziness and vertigo. These seizures tend to have a short duration of even just a few seconds to minutes and an abrutp ending. Diagnosis of VE may be confused with vestibular paroxysmia (VP), a much rarer disorder among dogs. consisting of brief episodes of spinning or non-spinning vertigo.
In this March 2024 article, VE was diagnosed in 10 dogs, including a cavalier King Charles spaniel. The episodes of VE in this study were recurrent, as may be epileptic seizures. See the linked article for details. Its authors suspect an epileptic origin for the VE episodes.
RETURN TO TOP
• inflammatory brain disease
Granulomatous meningoencephalitis (GME) is an inflammatory disease of the central nervous system (CNS) caused by the infiltration of normal, unaffected tissues by immune system cells, called mononuclear cells. It has been successfully treated with cyclophosphamide, an anti-cancer chemotherapy drug, and prednisone.
In a February 2021 article examining the medical records of 239 dogs identified with vestibular symptoms, 35 dogs (15.4%) were diagnosed with meningoencephalitis.
RETURN TO TOP
• nasopharyngeal polyps
Nasopharyngeal polyps are non-neoplastic masses, originating from the mucous lining of the nasopharynx, the tympanic bulla, or the Eustachian tube. Dogs with these polyps often display peripheral vestibular syndrome.
RETURN TO TOP
• intracranial neoplasia
Intracranial neoplasia is a brain tumor which can cause vestibular signs of either the peripheral or central variety. In a February 2021 article examining the medical records of 239 dogs identified with vestibular symptoms, 26 dogs (11.4%) were diagnosed with brain neoplasia.
RETURN TO TOP
• ototoxicity
Ototoxicity is poisoning which affects the ears, resulting from the reaction to drugs or chemicals which damage the inner ear or the vestibular nerve. Drugs known to cause ototoxicity include metronidazole*, neomycin and streptomycin.
*Metronidazole (Flagyl) may cause adverse events in dogs hypersensitive to it. See Metronidazole Risks. In a February 2021 article examining the medical records of 239 dogs identified with vestibular symptoms, 3 dogs (1.3%) were diagnosed with metronidazole toxicity.
RETURN TO TOP
Symptoms
 The typical symptoms of
peripheral vestibular disease (PVD)
include:
The typical symptoms of
peripheral vestibular disease (PVD)
include:
• Ataxia (a
staggering or rolling gait)
• Nystagmus
(uncontrolled movements of the eyes, usually from side to side, or in a
circular pattern)
• Strabismus (inability of the
eyes to aim at the same point in space)
• Head
tilt (see photo at top right)
• Circling*
•
Falling down
• Nausea signs (salivation, lip
licking, restlessness)
• Vomiting (usually at the
outset but not continuous)
These are standard signs of peripheral vestibular disorders. If the PVD is bilateral, no one-sided staggering occurs, and the dog's balance is lost on both sides.
* See Dr. Clare Rusbridge's YouTube video on the specific causes of circling.
Central vestibular disorders may also include nystagmus with the eyes moving vertically without any rotary component, and facial nerve twitching. CVD dogs are significantly more likely to not be able to walk at all -- to appear to be paralyzed.
Horner's syndrome is not a usual symptom of the idiopathic variety, but it is a typical sign of other peripheral versions of vestibular syndrome. Classic signs of Horner's syndrome are limited to one side of the face and include: small pupil size (miosis), protrusion of the third eyelid, drooping of the upper eyelid (ptosis), a sunken appearance to the eye (enophthalmos), and dilation of blood vessels on affected side of the face, which may make the area feel warmer.
Facial nerve paralysis is a common additional condition associated with vestibular symptoms.
In a November 2016 abstract, French researchers studied 69 dogs with facial nerve paralysis. The report does not provide a count of cavalier King Charles spaniels included in the study, but the researchers concluded that the CKCS and the French bulldog should be added to the list of predisposed breeds to the disorder. Additionally, they found that vestibular signs were the most common additional clinical signs and were observed in 36% of dogs with idiopathic facial paralysis. See our discussion of facial nerve paralysis for more information.
RETURN TO TOP
Diagnosis
Diagnosis of idiopathic vestibular disorder usually involves a process of, first, elimination of other possible causes of the symptoms, and second, determining whether the dysfunction is peripheral vestibular diease (PVD) or central vestibular disease (CVD). Diagnosing CVD involves identifying clinical signs which could not be attributed to PVD.
For those causes of vestibular syndrome other than the idiopathic variety, the diagnosis involves identifying the particular disease causing the symptoms. If benign paroxysmal positional vertigo (BPPV) is suspected, maneuvering tests such as the Dix - Hallpike maneuver and the side-lying maneuver, which involve protocols of postioning and then re-positioning the patient, may be performed.
A complete neurological examination would be appropriate, along with an otoscopic examination, x-rays of the tympanic bullae, computed tomography (CT) or magnetic resonance imaging (MRI), thyroid function testing, and a brainstem auditory evoked response (BAER) test. To diagnose central vestibular disease, either CT or MRI would be necessary.
RETURN TO TOP
Treatment
Idiopathic vestibular syndrome is known often to begin resolving itself within days or weeks without any treatment. However, the dog needs to be closely monitored during this period. Therefore, patience is required of the dog's owner, because the symptoms of this disorder can be very disturbing. Veterinarians may prescribe cerenia (maropitant citrate) tablets, or meclizine (Bonine, AntiVert), both motion-sickness medications, and/or a benzodiazepine drug called diazepam (Valium). Either maropitant or metoclopramide may be administered to limit vomiting.
In a July 2022 article, German and UK researchers studied the effects of ondansetron, a selective 5-HT3 receptor antagonist, administered intravenously in 14 dogs diagnosed with vestibular syndrome and nausea. They report finding that "Clinical resolution of nausea was observed 1 hour after administration of ondansetron, whereas serum AVP concentration decreased 4 hours after ondansetron administration." They concluded: "Administration of ondansetron IV is beneficial for dogs with nausea secondary to acute vestibular syndrome. Ondansetron substantially and rapidly decreased clinical signs of nausea behavior and stopped emesis. See, also, this March 2021 article.
In some cases, the corticosteroid drug prednisone may be prescribed.
A proven homeopathic version of motion-sickness medication is Cocculus Indicus.
Most dogs will make a full recovery although some may continue to have a slight head tilt. The recovery time could be from within less than an hour to weeks. Most recoveries occur within a couple of weeks.
If benign paroxysmal positional vertigo (BPPV) is suspected, physical maneuvering methods, such as canine versions of the positioning protocols such as the Semont Liberatory Maneuver and the Horizontal Canal Repositioning Maneuver, may be attempted. An example of such treatment is, first, to lie the dog on its side which seems to have the most nystagmus symptoms and watch the dog's eyes until the involuntary movements stop. Then wait about 30 seconds, holding the dog in that same position. Then turn the dog over so that it is lying on its other side. If and when any nystagmus symptoms end, hold the dog in that position for another 30 seconds. If the dog no longer has any symptoms, it would indicate that the maneuver successfully dislodged the loose granules from the canal and enabled them to flow back into the utricle.
In some cases, neuromuscular electrical stimulation (NMES) has reportedly helped to resolve the symptoms.
For those causes of vestibular syndrome other than the idiopathic variety, the treatment involves treating the particular disease causing the symptoms.
RETURN TO TOP
Research News
 August 2022:
Ondansetron quickly decreased nausea signs due to vestibular
syndrome, in 14 dog study. In a
July 2022 article, German and UK researchers (Lea Henze, Sarah Foth,
Sebastian Meller, Friederike Twele, Marios Charalambous, Hannah Kenward,
Jonathan Elliott, Ludovic Pelligand, Holger A. Volk) studied the effects of
ondansetron, a selective 5-HT3 receptor antagonist, administered
intravenously in 14 dogs diagnosed with vestibular syndrome and nausea.
They report finding that "Clinical resolution of nausea was observed 1
hour after administration of ondansetron, whereas serum AVP
concentration decreased 4 hours after ondansetron administration." They
concluded: "Administration of ondansetron IV is beneficial for dogs with
nausea secondary to acute vestibular syndrome. Ondansetron substantially
and rapidly decreased clinical signs of nausea behavior and stopped
emesis.
August 2022:
Ondansetron quickly decreased nausea signs due to vestibular
syndrome, in 14 dog study. In a
July 2022 article, German and UK researchers (Lea Henze, Sarah Foth,
Sebastian Meller, Friederike Twele, Marios Charalambous, Hannah Kenward,
Jonathan Elliott, Ludovic Pelligand, Holger A. Volk) studied the effects of
ondansetron, a selective 5-HT3 receptor antagonist, administered
intravenously in 14 dogs diagnosed with vestibular syndrome and nausea.
They report finding that "Clinical resolution of nausea was observed 1
hour after administration of ondansetron, whereas serum AVP
concentration decreased 4 hours after ondansetron administration." They
concluded: "Administration of ondansetron IV is beneficial for dogs with
nausea secondary to acute vestibular syndrome. Ondansetron substantially
and rapidly decreased clinical signs of nausea behavior and stopped
emesis.
 March 2021:
Ondansetron successfully treated nausea in dogs with vestibular
syndrome in a preliminary study.
In
a
March 2021 article, a team of UK and German veterinary researchers
(S. Foth, Sebastian Meller, Hannah Kenward, J. Elliot, L. Pelligand,
Holger Andreas Volk [right]) tested the selective 5-HT3
receptor antagonist ondansetron to treat 16 dogs diagnosed with
vestibular syndrome and signs of experiencing nausea. They evaluated the
dogs' reactions by nausea-like behaviors on a 5-point numerical rating
scale -- salivation, lip licking, restlessness, vocalisation, and
lethargy. They report finding evidence of the efficacy of ondansetron as
a successful treatment for nausea in dogs with vestibular disease.
March 2021:
Ondansetron successfully treated nausea in dogs with vestibular
syndrome in a preliminary study.
In
a
March 2021 article, a team of UK and German veterinary researchers
(S. Foth, Sebastian Meller, Hannah Kenward, J. Elliot, L. Pelligand,
Holger Andreas Volk [right]) tested the selective 5-HT3
receptor antagonist ondansetron to treat 16 dogs diagnosed with
vestibular syndrome and signs of experiencing nausea. They evaluated the
dogs' reactions by nausea-like behaviors on a 5-point numerical rating
scale -- salivation, lip licking, restlessness, vocalisation, and
lethargy. They report finding evidence of the efficacy of ondansetron as
a successful treatment for nausea in dogs with vestibular disease.
February 2021:
Cavaliers were the most common breed in UK study of 239 dogs
with vestibular syndrome.
 In a
February 2021 article by a team of Royal Veterinary College (RVC)
researchers (Eleanor Harrison, Nick J. Grapes, Holger A. Volk, Steven De
Decker [right]), they examined the RVC medical records of 239 dogs
diagnosed with vestibular syndrome, in an effort to identify observable
symptoms with the most common causes of the disorder. The most common
breed among the 239 dogs was the cavalier King Charles spaniel (26 dogs
-- 11%). They report finding fifteen underlying disorders:
In a
February 2021 article by a team of Royal Veterinary College (RVC)
researchers (Eleanor Harrison, Nick J. Grapes, Holger A. Volk, Steven De
Decker [right]), they examined the RVC medical records of 239 dogs
diagnosed with vestibular syndrome, in an effort to identify observable
symptoms with the most common causes of the disorder. The most common
breed among the 239 dogs was the cavalier King Charles spaniel (26 dogs
-- 11%). They report finding fifteen underlying disorders:
• Idiopathic vestibular disease: 78 dogs -- 34.2%
• Otitis media interna: 54 dogs -- 23.7%
• Meningoencephalitis (inflammation of brain and meninges): 35 dogs -- 15.4%
• Brain neoplasia (tumor): 26 dogs -- 11.4%
• Ischaemic infarct (stroke): 25 dogs -- 11%
• Intracranial empyema (pus): 4 dogs -- 1.8%
• Metronidazole (Flagyl) toxicity: 3 dogs -- 1.3%
• Neoplasia (tumor) affecting the middle ear: 3 dogs -- 1.3%
• Primary secretory otitis media (PSOM): 2 dogs -- 0.8%
• Congenital cerebellar malformation: 2 dogs -- 0.8%
• Corticosteroid responsive tremor syndrome: 2 dogs -- 0.8%
• Hypothyroidism: 2 dogs -- 0.8%
• Congenital vestibular syndrome: 1 dog -- 0.4%
• Fucosidosis (rare genetic enzyme disorder): 1 dog -- 0.4%
• External trauma: 1 dog -- 0.4%
They found that idiopathic vestibular disease was associated with higher age, higher bodyweight, improving clinical signs, pathological nystagmus, facial nerve paresis, absence of Horner's syndrome, and a peripheral localization. Otitis media interna was associated with younger age, male gender, Horner's syndrome, a peripheral localization, and a history of otitis externa. Ischaemic infarct was associated with older age, peracute onset of signs, absence of strabismus, and a central localisation. They concluded that discrete clinical features can be used to identify the most likely diagnosis in dogs with vestibular syndrome.
August 2020:
Cavaliers have fourth highest odds of vestibular disaease in
one-year UK study of primary-care clinics.
 In an
August 2020 article, UK investigators (Sinziana Maria Radulescu
[right],
Karen Humm, Louis Mark Eramanis, Holger A. Volk, David B. Church, David
Brodbelt, Dan Gerard O'Neill) reviewed the UK primary care clinical
records for the year 2016 of over 900,000 dogs, finding 759 cases of
diagnosis of vestibular disease (VD). The breeds with the highest odds
of VD diagnosis that year were French bulldogs, English bulldogs, King
Charles spaniels (English toy spaniels), and cavalier King Charles spaniels, followed by the
Springer spaniel, boxer, and golden retriever breeds. The authors had
special comments about cavaliers and their suseceptibility for VD, as
follows:
In an
August 2020 article, UK investigators (Sinziana Maria Radulescu
[right],
Karen Humm, Louis Mark Eramanis, Holger A. Volk, David B. Church, David
Brodbelt, Dan Gerard O'Neill) reviewed the UK primary care clinical
records for the year 2016 of over 900,000 dogs, finding 759 cases of
diagnosis of vestibular disease (VD). The breeds with the highest odds
of VD diagnosis that year were French bulldogs, English bulldogs, King
Charles spaniels (English toy spaniels), and cavalier King Charles spaniels, followed by the
Springer spaniel, boxer, and golden retriever breeds. The authors had
special comments about cavaliers and their suseceptibility for VD, as
follows:
"CKCS are known to be predisposed to several neurological syndromes that can cause vestibular signs, including occipital hypoplasia/syringomyelia, granulomatous meningoencephalomyelitis (GME), and VD. Moreover, CKCS have a tendency toward cerebrovascular disease, particularly rostral cerebellar artery infarction. In immature dogs, the first presenting sign of syringomyelia could be scoliosis, which can appear similar to a head tilt of vestibular origin. VD in CKCS can be also idiopathic -- CKCS is one of the most commonly seen breeds with idiopathic facial nerve paralysis and facial and vestibular neuropathy of unknown origin. Aside from central and IPVD [idiopathic peripheral VD], CKCS are also predisposed to primary secretory otitis media, known to commonly be associated with peripheral VD."
The most common symptoms of VD were: head tilt (69.8%), nystagmus (uncontrolled movements of the eyes, usually from side to side, or in a circular pattern) (68.1%), and ataxia (a staggering or rolling gait) (64.5%). The most frequently used treatments were antiemetics (43.2%), systemic glucocorticoids (33.1%), antimicrobials (25%), and propentofylline (23.25%).
May 2020:
Cavaliers rank #1 in most commonly affected breeds for
peripheral vestibular disease in a UK study.
 In
a
May 2020 article, UK researchers Rocio Orlandi (right),
Rodrigo Gutierrez-Quintana, Beatrice Carletti, Camilla Cooper, Josep
Brocal, Sara Silva, Rita Gonçalves studied 188 dogs in two UK veterinary
clincs between 2013 and 2019. Of all 188 affected dogs, 38 (20%) of them
were cavalier King Charles spaniels, which they reported as the most
commonly affected breed in the study. Clinical signs included head tilt
(185 dogs), ataxia (123), facial paralysis (103), nystagmus (97),
positional strabismus (93) and Horner syndrome (7). The most prevalent
diagnosis was idiopathic vestibular disease (128 dogs), followed by
otitis media and/or interna (49), hypothyroidism (7), suspected
congenital vestibular disease (2), neoplasia (1) and cholesteatoma (1).
Magnetic resonance imaging (MRI) was performed on all patients. The
researchers concluded that:
In
a
May 2020 article, UK researchers Rocio Orlandi (right),
Rodrigo Gutierrez-Quintana, Beatrice Carletti, Camilla Cooper, Josep
Brocal, Sara Silva, Rita Gonçalves studied 188 dogs in two UK veterinary
clincs between 2013 and 2019. Of all 188 affected dogs, 38 (20%) of them
were cavalier King Charles spaniels, which they reported as the most
commonly affected breed in the study. Clinical signs included head tilt
(185 dogs), ataxia (123), facial paralysis (103), nystagmus (97),
positional strabismus (93) and Horner syndrome (7). The most prevalent
diagnosis was idiopathic vestibular disease (128 dogs), followed by
otitis media and/or interna (49), hypothyroidism (7), suspected
congenital vestibular disease (2), neoplasia (1) and cholesteatoma (1).
Magnetic resonance imaging (MRI) was performed on all patients. The
researchers concluded that:
"Idiopathic vestibular disease is the most common cause of peripheral vestibular dysfunction in dogs and it is associated with advanced age. Incomplete recovery from peripheral vestibular disease is common, especially in dogs presenting with cranial nerve enhancement on MRI but less so if there is previous history of vestibular episodes."
April 2019:
Cavaliers are found among the top four breeds predisposed for
vestibular disease in the UK.
 In an
April 2019 abstract at the BVASA Congress, researchers (Sinziana
Maria Radulescu, Karen Humm, Louis Mark Eramanis, Holger Volk
[right], Dave C. Brodbelt, David B. Church, Dan G. O’Neill) reviewing the
2016 data in the UK VetCompass database report that among 905,544 dogs,
759 vestibular cases were confirmed, with an overall prevalence of
0.08%. The cavalier King Charles spaniel was the fourth most predisposed
breed (the top three were the Springer spaniel, golden retriever, and
border collie) with 2.70 times the odds for developing vestibular
compared to cross-breeds. The most common signs were: head tilt (69.8%),
nystagmus (68.1%), and ataxia (64.5%). The most frequently used
treatments were: antiemetics, cortisteroids, antimicrobials, and
propentofylline.
In an
April 2019 abstract at the BVASA Congress, researchers (Sinziana
Maria Radulescu, Karen Humm, Louis Mark Eramanis, Holger Volk
[right], Dave C. Brodbelt, David B. Church, Dan G. O’Neill) reviewing the
2016 data in the UK VetCompass database report that among 905,544 dogs,
759 vestibular cases were confirmed, with an overall prevalence of
0.08%. The cavalier King Charles spaniel was the fourth most predisposed
breed (the top three were the Springer spaniel, golden retriever, and
border collie) with 2.70 times the odds for developing vestibular
compared to cross-breeds. The most common signs were: head tilt (69.8%),
nystagmus (68.1%), and ataxia (64.5%). The most frequently used
treatments were: antiemetics, cortisteroids, antimicrobials, and
propentofylline.
January 2016: French researchers include two cavaliers in study of facial and vestibular neuropathy of unknown origin. In a January 2016 article, the same team of French researchers who reported in July 2015 that cavalier King Charles spaniels were "highly represented in study of idiopathic labial and facial canine vestibular neuropathy", reported on 16 dogs, including 2 cavaliers, with facial and vestibular neuropathy of unknown origin (FVNUO). They stated that all of the dogs had onset of the FVNUO in less than 24 hours, and that their thyroid function was within normal limits. None of the 16 dogs received any treatment except artificial tears. Vestibular signs resolved and a return to normal facial movement occurred in one of the CKCSs. The other cavalier developed hemifacial contracture. They concluded that "FVNUO shares similarities with idiopathic facial paralysis. The prognosis for return of normal facial and vestibular function is guarded and there may be relapse after recovery."
January 2016:
US Neurologist Rossmeisl finds PSOM, CM/SM, brachycephalic airway
obstruction syndrome and laryngeal paralysis in a cavalier.
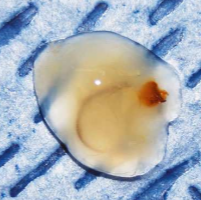 In a
January 2016 article, Virginia Tech veterinary neurologist John
Rossmeisl reports on a 13-year-old, male castrated cavalier King Charles
spaniel which had symptoms of vestibular disease -- a left head tilt and
circling to the left, which progressed to left lateral recumbency,
positional strabismus (OS), and rotary nystagmus (OU) -- and also the
absence of postural reactions in all limbs, exaggerated spinal reflexes
in all limbs, and respiratory distress. He performed an MRI and
otoscopic examination and performed a myringotomy. (See specimen of
mucus at right.) He found no evidence
of inflammation or infection. He diagnosed: (a) primary secretory otitis
media (PSOM), causing the peripheral vestibular signs; (b)
CM/SM,
causing the central nervous system symptoms; (c)
brachycephalic airway
obstruction syndrome (BAOS) and laryngeal paralysis, causing the dog’s
inability to walk and required tracheal intubation and supplemental
oxygen. The owner chose euthanasia rather than surgery to relieve the
BAOS.
In a
January 2016 article, Virginia Tech veterinary neurologist John
Rossmeisl reports on a 13-year-old, male castrated cavalier King Charles
spaniel which had symptoms of vestibular disease -- a left head tilt and
circling to the left, which progressed to left lateral recumbency,
positional strabismus (OS), and rotary nystagmus (OU) -- and also the
absence of postural reactions in all limbs, exaggerated spinal reflexes
in all limbs, and respiratory distress. He performed an MRI and
otoscopic examination and performed a myringotomy. (See specimen of
mucus at right.) He found no evidence
of inflammation or infection. He diagnosed: (a) primary secretory otitis
media (PSOM), causing the peripheral vestibular signs; (b)
CM/SM,
causing the central nervous system symptoms; (c)
brachycephalic airway
obstruction syndrome (BAOS) and laryngeal paralysis, causing the dog’s
inability to walk and required tracheal intubation and supplemental
oxygen. The owner chose euthanasia rather than surgery to relieve the
BAOS.
August 2015: Cerebellar infarction symptoms in cavaliers resemble acute vestibular signs. In an August 2015 abstract, UK neurologists (B. Thomsen, L. Garosi, G. Skerritt, C. Rusbridge, T. Sparrow, M. Berendt, H. Gredal) report finding cerebellar infarctions in 24 dogs, including 9 cavalier King Charles spaniels, displaying ataxia (staggering or rolling gait), hypermetria (voluntary muscular movements tend to overreach their intended goals), head tilt, nystagmus (uncontrolled movements of the eyes), reduced postural reactions (e.g., replacing a foot after being lifted), and decreased menace response (eye blinking in response to an on-coming object). They concluded that cerebellar ischemic strokes should be considered an important differential diagnosis in dogs with acute vestibular signs.
July 2015:
French researchers find cavaliers highly represented in study of
idiopathic labial and facial canine vestibular neuropathy.
 In an
April 2015 article, a team of French researchers (Aurélien
Jeandel (right), J.
Thibaud, F. Delisle, Stephane Blot) found 21 dogs with cases of idiopathic
labial and facial canine vestibular neuropathy over the past ten years.
The inclusion criteria were: (1) Dog with clinical signs consistent with
vestibular syndrome and facial paralysis; (2) No argument suggesting a
central nervous system; (3) Normal MRI of the brain parenchyma and
absence of middle or inner ear infection. Of the 21 dogs found, there
were 4 American Staffordshire Terriers, 3 cavalier King Charles
spaniels, and 3 Boxers. Sixteen were male and 5 were female. The median
age of presentation was 6.6 years. In all cases, the onset of the
symptoms were acute. The vestibular syndrome symptoms most frequently
encountered were torticollis (21/21) and nystagmus (16/21).
In an
April 2015 article, a team of French researchers (Aurélien
Jeandel (right), J.
Thibaud, F. Delisle, Stephane Blot) found 21 dogs with cases of idiopathic
labial and facial canine vestibular neuropathy over the past ten years.
The inclusion criteria were: (1) Dog with clinical signs consistent with
vestibular syndrome and facial paralysis; (2) No argument suggesting a
central nervous system; (3) Normal MRI of the brain parenchyma and
absence of middle or inner ear infection. Of the 21 dogs found, there
were 4 American Staffordshire Terriers, 3 cavalier King Charles
spaniels, and 3 Boxers. Sixteen were male and 5 were female. The median
age of presentation was 6.6 years. In all cases, the onset of the
symptoms were acute. The vestibular syndrome symptoms most frequently
encountered were torticollis (21/21) and nystagmus (16/21).
RETURN TO TOP
Related Links
Veterinary Resources
Results of magnetic resonance imaging in dogs with vestibular disorders: 85 cases (1996-1999). Laurent S. Garosi, Ruth Dennis, Jacques Penderis, Christopher R. Lamb, Mike P. Targett, Rodolfo Cappello, Agnes J. Delauche. J Am Vet Med Assoc February 2001;218:385–391. Quote: Objective: To determine results of magnetic resonance (MR) imaging in dogs with vestibular disorders (VD) and correlate results of MR imaging with clinical findings. Design: Retrospective study. Animals: 85 dogs. Procedure: Information on signalment, clinical signs, and presumptive lesion location was obtained from the medical records, and MR images were reviewed. Results: 27 dogs had peripheral VD, 37 had central VD, and 21 had paradoxical VD. Of the 27 dogs with peripheral VD, 11 (41%) had MR imaging abnormalities involving the ipsilateral tympanic bulla compatible with otitis media (6 also had abnormalities involving the petrous portion of the ipsilateral temporal bone compatible with otitis interna), 7 (26%) had MR imaging abnormalities compatible with middle ear neoplasia, 2 (7%) had an ipsilateral cerebellopontine angle lesion, and 7 (26%) did not have MR imaging abnormalities. All dogs with central and paradoxical VD had abnormalities evident on MR images. Of the 37 dogs with central VD, 13 (35%) had an extra-axial lesion, 6 (16%) had an intra-axial lesion, and 18 (49%) had multiple intra-axial lesions. In 23 (62%) dogs with central VD, lesions on MR images corresponded with location suspected on the basis of clinical signs. Of the 21 dogs with paradoxical VD, 12 (57%) had an extra-axial lesion, 5 (24%) had an intra-axial lesion, and 4 (19%) had multiple intra-axial lesions. Location of lesions on MR images agreed with location suspected on the basis of clinical signs in 19 (90%) dogs. Conclusions and Clinical Relevance: Results suggest that MR imaging may be helpful in the diagnosis and treatment of VD in dogs.
Vestibular Diseases of Cats and Dogs. Richard A. LeCouteur. 2002 WSAVA Congress. August 2002.
Neurological diseases of the Cavalier King Charles spaniel. Rusbridge, C. J. Small Animal Practice. June 2005;46(6): 265-272. "Vestibular syndrome is one of the most common neurological presentations. Clinical signs may include some or all of the following: head tilt, ataxia, circling, rolling, tendency to lean to side of head tilt, and deviation of eye ventrally (ipsilateral to head tilt) when the head is elevated above the horizontal plane. For prognostic purposes, it is vital to distinguish between peripheral and central disease."
Signs of neurologic dysfunction in dogs with central versus peripheral vestibular disease. Mark T. Troxel, Kenneth J. Drobatz, Charles H. Vite. J Am Vet Med Assoc. August 2005; doi: 10.2460/javma.2005.227.570 Quote: Objective: To determine the frequency of specific signs of neurologic dysfunction in dogs with central vestibular disease (CVD) or peripheral vestibular disease (PVD) and whether the degree of head tilt, rate of nystagmus, and number of beats of postrotatory nystagmus can be used to help distinguish CVD from PVD. Design: Prospective clinical study. Animals: 40 client-owned dogs with vestibular system dysfunction. Procedure: A standard neurologic examination was performed, along with an expanded vestibular system examination that assessed the degree of head tilt, rate of nystagmus, and number of beats of postrotatory nystagmus. Results: Dogs with CVD were significantly more likely to be nonambulatory than were dogs with PVD. Dogs with PVD were significantly more likely to veer or lean in 1 direction and to have resting nystagmus than were dogs with CVD. Median rate of resting nystagmus was significantly higher for dogs with PVD, but no significant differences between groups were detected in regard to presence or degree of head tilt, presence of positional ventral strabismus, and number of beats of postrotatory nystagmus. Conclusions and Clinical Relevance: Results suggest that nonambulatory tetraparesis is significantly more common in dogs with CVD and veering and leaning are significantly more common in dogs with PVD. Although neither the degree of head tilt nor the number of beats of postrotatory nystagmus could be used to distinguish CVD from PVD, rate of resting nystagmus may be useful in distinguishing the 2 conditions.
Proposed Treatment for Vestibular Dysfunction in Dogs. Margaret Kraeling. CHAP Newsletter. December 2007; 6–9.
Vestibular Disease in Dogs and Cats. Simon Platt. 2008 WSAVA Congress. August 2008.
Optic neuritis in a Cavalier King Charles Spaniel. M. K. Zarfoss. Cornell Univ. September 2008. Senior seminar paper. Quote: "Betsy, a 4.5 year-old female spayed Cavalier King Charles Spaniel, was presented to the Cornell University Hospital for Animals for evaluation of acute blindness, inappetance, and lethargy. Ophthalmic examination revealed keratoconjunctivitis sicca in both eyes (OU), absent menace OU, decreased pupillary light responses OU, posterior vitreal haze OU, and optic disk enlargement OU. A diagnosis of optic neuropathy was pursued because of bilaterally enlarged optic disks in the absence of other localizing clinical signs or ophthalmic abnormalities sufficient to cause blindness. The presumptive diagnosis of optic neuritis due to granulomatous meningoencephalomyelitis (GME) was based upon: peripapillary retinal vasculitis on fluorescein angiography, severe lymphocytic inflammation within the cerebrospinal fluid (CSF), negative infectious disease serum and CSF titers, and favorable response to immuno-suppression. Granulomatous meningoencephalomyelitis is an inflammatory disease of the central nervous system (CNS) of undetermined etiology and poor prognosis. Successful treated of this dog's GME consisted of conventional treatment using oral prednisone and non-conventional treatment using an additional immunosuppressive agent, cytosine arabinoside."
The neurology of balance: Function and dysfunction of the vestibular system in dogs and cats. Marc Kent, Simon R. Platt, Scott J. Schatzberg. Vet. J. September 2010; doi: 10.1016/j.tvjl.2009.10.029 Quote: Disorders affecting the vestibular system are a common neurological problem encountered in small animal practice. As a result, veterinarians are often faced with determining the underlying etiology of affected animals. In order to establish an accurate etiological diagnosis, proper interpretation of neurological deficits and precise neuroanatomical localization are essential. Neurological examination can confirm whether the vestibular dysfunction is of peripheral or central nervous system origin. Peripheral vestibular diseases include idiopathic vestibular syndrome, which has some similarities with vestibular neuritis in humans. Central vestibular diseases in general have a poor prognosis in comparison to those affecting the peripheral vestibular system.
Vestibular Disease: Anatomy, Physiology, and Clinical Signs. Mark Lowrie. VetLearn Compendium. July 2012;34(7). Quote: "The vestibular system is responsible for keeping an animal oriented with respect to gravity. It is a sensory system that maintains the position of the eyes, body, and limbs in reference to the position of the head. Proper interpretation of neurologic deficits and precise neuroanatomic localization are essential to diagnose and prognosticate the underlying disorder. Neurologic examination can confirm whether the vestibular dysfunction is of peripheral or central nervous system origin. Idiopathic vestibular syndrome is the most common cause of peripheral vestibular disease in dogs and, despite its dramatic clinical presentation, can improve without intervention. Central vestibular diseases generally have a poorer prognosis. ... Granulomatous meningoencephalomyelitis (GME) is a severe inflammatory disease of the central nervous system (CNS), characterised by large perivascular accumulations of mononuclear cells in the parenchyma and meninges of the brain and spinal cord (Braund and others 1978). The aetiology is unknown. It is most common in middle-aged dogs, although it can occur from age six months to 10 years (Braund 1985). Female dogs are slightly more commonly affected than male dogs (Braund 1985). Clinical signs reflect the area of brain or spinal cord affected. The most common signs are spinal pain, depression, seizures, vestibular signs, paresis and postural deficits. Disseminated and focal forms are recognised and focal forms may present with just involvement of the optic nerves manifesting as sudden onset blindness (Braund 1985). Diagnosis is suggested by appropriate MRI and CSF changes and by ruling out infectious causes of encephalitis (Fig 4), but can only be confirmed by postmortem examination."
Vestibular Disease. Simon R. Platt. Clinicians Brief. December 2012.
Neck Stiffness & Head Tilt in a Young Spaniel. Louis N. Gotthelf. Clinician's Brief. March 2013: 23-25. Quote: "A 9-month-old female Cavalier King Charles spaniel presented for apparent neck pain when walked on a leash. History: The owner reported neck stiffness and head tilt. After the leash had been removed, the signs continued to persist for more than 24 hours. The puppy appeared bright, alert, and responded when called. Examination: Physical examination did not elicit a painful response when the head and neck were manipulated in any direction. A slight head tilt was observed when the puppy walked freely in the clinic; however, laboratory diagnostics were not performed. Evaluation may reveal a bulging eardrum, indicative of primary secretory otitis media (PSOM). PSOM of Cavalier King Charles spaniels (CKCSs) commonly occurs as head and neck pain that may be difficult to localize. With pressure in the bulla, Horner syndrome or facial nerve palsy may be evident. Vestibular disease may be present with increased bulla pressure and can manifest as nystagmus or head tilt. Breed-Specific Considerations: Careful examination can reveal an abnormal or bulging eardrum. Clinicians adept at visualizing a normal eardrum with a handheld otoscope can detect a bulging eardrum; the tip of the cone has to be small yet long enough to make the bend in the ear canal. The tip of the otoscope cone should be placed in the horizontal ear canal close enough to the eardrum to focus on the tympanic membrane. A highly magnified, well illuminated examination should be done with a video otoscope to determine eardrum status. Bottom Line: CKCS eardrums should always be evaluated. If PSOM is suspected, a high-magnification eardrum examination may require referral. PSOM can be asymptomatic in CKCSs, in which case myringotomy is not required; however, the owner should be educated to take appropriate steps if signs are displayed. The Take-Home: CKCSs often have a genetic defect of their eustachian tube that results in PSOM, which may be asymptomatic. Bulging eardrum and ear pain are typical of PSOM in CKCSs. PSOM should be differentiated from SM via eardrum evaluation and MRi (if necessary). Myringotomy can relieve PSOM signs. Antibiotics will not be helpful. Periodic treatment is required."
Proposed Treatment for Geriatric Vestibular Disease in Dogs. Margaret Kraeling. Topics in Companion Animal Medicine. March 2014;29(1):6-9. Quote: "Sudden-onset vestibular dysfunction in the canine is a commonly seen condition in veterinary practice, with some veterinarians reporting several cases each month. However, traditional veterinary medicine has little to offer these patients other than symptomatic relief for the severe nausea that accompanies the vertigo and supportive advice for the owners. Owners of affected dogs are informed that these symptoms usually resolve within a few days. As physical therapists, we often see cases of benign paroxysmal positional vertigo in our human practice clinics, and effective protocols for diagnosis and treatment of the condition have been developed for this condition. A modified testing and repositioning postural maneuver used successfully on 12 canine patients in our canine rehabilitation clinic (The Canine Fitness Centre, Calgary, Alberta, Canada) is hereby described."
Otitis externa and media -- pathogenisis and signs. Filippo de Bellis. Vet. Times. December 2014. Quote: "Otitis media: In dogs and cats, otitis media can be primary or secondary. In cats, primary otitis media occurs as a result of an infection ascending through the Eustachian tube to the middle ear. An exact mechanism for the development of otitis media has not been reported, although the bacterial isolates from the bullae of cats with middle ear disease are consistent with respiratory pathogens. It has been hypothesised that chronic viral upper respiratory infection early in life may play a role in initiating otitis media in cats. In dogs, primary otitis media can also originate from ascending nasal or respiratory infections through the auditory tube, although otitis media most often occurs as an extension of otitis externa. Additionally, it can occur as primary disease due to middle ear or auditory tube abnormalities such as with primary secretory otitis media, most often seen in cavalier King Charles spaniels. It has been speculated the primary otitis in these cases could occur secondarily to structural changes in the soft palate or nasopharyngeal apertures. Secondary otitis media in cats is reported as a consequence of ear mite infestation with subsequent rupture of the tympanic membrane or as extension of a nasopharyngeal polyp (Figure 3) originating from the middle ear mucosa and growing through the tympanic membrane. Secondary otitis media in dogs can be caused by draining through a damaged ear drum, of exudates, infectious organisms, debris and residuals of medications. Once an inflammatory process is established, a series of pathological changes take place including oedema, ulcerations, granulation tissue formation, and osteomyelitis. Clinical signs of otitis media are variable. Most commonly, dogs and cats with a perforated ear drum show large amount of liquid discharge within the ear canal, often with mucous material produced by the lining of the tympanic bulla. Additionally, due to the close proximity of the inner ear structures, patients with otitis media can also develop vestibular signs. Summarising, clinical presentation of otitis media can include: facial nerve paralysis; Horner’s syndrome; hearing abnormalities; ataxia; head tilt; ventro-lateral strabismus; nystagmus; respiratory signs; pain on palpation of the base of the ear; and reluctance to open the mouth."
The vestibular and facial idiopathic neuropathy in dogs: 21 cases study (Les neuropathies vestibulaires et faciales idiopathiques chez le chien : étude de 21 cas). A. Jeandel, J. Thibaud, F. Delisle, S. Blot. Revue Vétérinaire Clinique. April 2015;50(2):76-77. Quote: [Google translation] "The peripheral vestibular syndrome (PVS), secondary to impairment of the vestibular nerve or its receptors, often idiopathic or inflammatory origin (otitis interna) in dogs. In otitis media / internal, one can observe a SVP associated with facial paralysis. Yet described vestibular damage associated with facial paralysis without abnormality of the middle / inner ear during the MRI. Similarly, considered idiopathic facial paralysis are sometimes associated with vestibular symptoms. No item specifically addresses these labial and facial idiopathic neuropathy (NVFI) 0030, 0035, 0040, 0045 and 0050. The aim of our study was to retrospectively identify cases of NVFI, to describe the epidemiology, clinical presentation, paraclinical changes and the evolution of these animals in the long term. The cases of NVFI within the last ten years were reviewed. The inclusion criteria were as follows: (1) Dog with clinical signs consistent with vestibular syndrome and facial paralysis; (2) No argument suggesting a central nervous system; (3) Normal MRI of the brain parenchyma and absence of middle or inner ear infection. Twenty-one dogs have fulfilled these inclusion criteria. The most represented breeds are American Staffordshire Terriers (4), the Boxers (3), the cavalier King Charles (3). Sixteen males are identified against five females. The presence of male was significantly higher (p = 0.027). The median age of presentation was 6.6 years [0.5 to 12.5]. In all cases, the reported method of onset is acute (less than 72 h). The symptoms most frequently encountered vestibular syndrome are torticollis (21/21), nystagmus (16/21). A dog was being treated for diabetes mellitus. A Schirmer test was performed in seven dogs: one case of quantitative tear deficiency was observed. The cytological examination of CSF is normal in all dogs removed. By cons, compared to a contemporary witness population with idiopathic epilepsy, protein level was significantly increased (p <0.001): median 0.40 g / L [0.20 to 0.90]. A search of infectious agents was performed in three animals (PCR LCS) the examination was normal. Cholesterol assays, triglycerides, total T4 and TSH, performed in 10 animals are within the usual values. The clinical evolution of the vestibular and facial involvement was documented in these seventeen of these animals (followed six months). Clinical remission is random and its duration is very variable. About residual vestibular disorders, permanent torticollis is reported in three cases, intermittent in four cases. The median disease duration was 60 days [1-730]. Regarding the signs of facial involvement, the return to proper function (eyelid closure, no food waste) is reported in fourteen cases, including six cases with hemifacial spasm sequelae. The median disease duration was 53 days [7-730]. Self-resolvent recurrences are reported by owners in three animals during the telephone follow-up. A recurrence was observed during monitoring by a clinician to establish the contralateral part in two animals after remission of the first episode. An MRI control and LCS puncture confirmed contralateral recurrence in one of them. When SVP associated with facial paralysis of acute onset with a dog, so it should be integrated in the diagnostic hypotheses NVFI. The origin of this concomitant damage is probably related to nearby course of these nerves when they entered in their respective channel in the temporal bone through the internal acoustic meatus. Recovery is variable. An inflammatory origin is suspected given the protein level changes observed."
Neurological signs in 24 dogs with rostral cerebellar infarction. B. Thomsen, L. Garosi, G. Skerritt, C. Rusbridge, T. Sparrow, M. Berendt, H. Gredal. 27th ESVN-ECVN Symposium. J.Vet.Int.Med. August 2015; ESVN-ECVN Abstracts p.27. Quote: "Studies on canine ischemic stroke suggest an overrepresentation of cerebellar cases. Although not the leading localization in humans, a cerebellar stroke syndrome characterized by vertigo, ataxia, nystagmus, and headache is described. Purpose of the present study was to characterize neurological signs in dogs with cerebellar infarction. A retrospective multicenter study of dogs examined 2010–2014 was performed. Dogs with acute non-progressive neurological deficits and magnetic resonance imaging suggestive of cerebellar infarction were eligible for inclusion. Twenty-four dogs (16 females, 8 males) with a median age of 8 years (range 3–11 years) were included. Breeds comprised the Cavalier King Charles Spaniel (n = 9), Greyhound (n = 3), Labrador Retriever (n = 2), and ten other breeds. In all dogs, infarcts were located to the rostral cerebellum and the territory of the rostral cerebellar artery (left n = 13, right n = 10, midline n = 1). Common neurological deficits were ataxia (n = 24), hypermetria (n = 12), contralateral head tilt (n = 13), nystagmus (n = 8), reduced postural reactions (n = 8), and decreased menace response (ipsilateral n = 4, bilateral n = 2). Four dogs had additional non-cerebellar brain infarcts. Six dogs had a history suggestive of a possible transient ischemic attack. Cerebellar ischemic stroke should be considered an important differential diagnosis in dogs with acute vestibular signs. A syndrome of canine cerebellar ischemic stroke caused by infarction in the territory supplied by the rostral cerebellar artery with neurological deficits resembling its human counterpart does seem to exist."
What is your diagnosis? Middle ear material from a dog. Nicole M. Weinstein, Katie M. Boes, Elizabeth Mauldin, John Rossmeisl. Vet. Clinical Pathology. January 2016. Quote: “Case Presentation: A 13-year-old, male castrated Cavalier King Charles Spaniel (CKCS) was referred ... for suspected vestibular disease of 2 days duration. The clinical history included a left head tilt and circling to the left, which progressed to left lateral recumbency within approximately 12 hours. Upon admission, respiratory distress was also noted. Relevant physical and neurologic examination findings included moderate bilateral otic discharge, positional strabismus (OS), rotary nystagmus (OU) with a fast phase to the right, absence of postural reactions in all limbs, and exaggerated spinal reflexes in all limbs. The clinical examination findings supported a multifocal neurologic condition that included dysfunction of both peripheral and central vestibular systems. Magnetic resonance imaging (MRI) and an otoscopic examination were performed. MRI revealed material in both the left and right ear bullae as well as caudal occipital malformation syndrome–syringohydromyelia (COMS-SM). During the otoscopic exam, the left tympanic membrane was bulging, but intact, while the right was ruptured. Slides of material obtained during myringotomy on the left ear were submitted for cytologic evaluation. Interpretation: Primary secretory otitis media. ... No evidence of inflammation or infection was identified. The combination of patient breed, gross appearance, and cytologic findings was compatible with primary secretory otitis media (PSOM). While the peripheral vestibular signs were explained by PSOM, the central nervous system signs were attributed to COMS and syrinx formation. Both brachycephalic airway syndrome and laryngeal paralysis were also diagnosed and may have contributed to the patient’s inability to ambulate given persistent hypoxemia that required intubation and oxygen supplementation. Surgery to alleviate the upper airway disease was discussed, but the owner elected euthanasia. Discussion: ... Common clinical signs in dogs with PSOM include head and cervical pain, and vocalization. Some dogs also exhibit aural pruritus with or without obvious otitis externa. Neurologic signs are present less often and may include ataxia, nystagmus, head tilt, facial paralysis, or seizures. The tympanic membrane is often intact but may be bulging and appear opaque. A white to yellow mucus plug can be visualized during myringotomy or if the tympanic membrane is not intact. Recurrence following ear flushing is common, but the prognosis is considered good, including in dogs with progressive disease. In approximately 50% of CKCS dogs undergoing imaging, PSOM is an incidental finding. The resolution of vestibular signs following removal of the mucus plug, even in dogs with COMS with or without syringomyelia, supports PSOM as a distinct disease entity rather than as an entirely incidental finding. The exact cause of PSOM in dogs is unknown.”
Facial and vestibular neuropathy of unknown origin in 16 dogs. A. Jeandel, J. L. Thibaud, S. Blot. J. Sm. Anim. Pract. January 2016. Quote: "Objectives: The aim of this study was to describe the signalment, clinical presentation, diagnostic findings and long-term follow-up in dogs with concomitant facial and vestibular neuropathy of unknown origin [FVNUO]. Methods: Appropriate cases were located through medical record searches. Inclusion criteria comprised dogs that had: clinical signs of facial paralysis with concomitant peripheral vestibular syndrome, thyroid function tests, no abnormalities on magnetic resonance imaging of the brain and tympanic bullae, and cerebrospinal fluid analysis. Results: Sixteen dogs met the inclusion criteria [including 2 cavalier King Charles spaniels]. Facial paralysis had acute onset (<24 hours) in all dogs, thyroid function was within normal limits. ... None of the 16 dogs received any treatment except artificial tears. Follow-up was incomplete for three dogs. In eight dogs (62%), vestibular signs resolved [including one of the cavalier King Charles spaniels]. The median time to complete PVS [peripheral vestibular syndrome] resolution was 55 days (range, 3 to 365). A return to normal facial movement was reported in five dogs (39%) [including one of the cavalier King Charles spaniels]. The median time to FP [facial paralysis] resolution was 45 days (range, 7 to 730). Complete resolution of both PVS and FP was observed in four dogs (31%) [including one of the cavalier King Charles spaniels]. The nine other dogs exhibited long-term sequelae: five dogs (38%) displayed a persistent or intermittent head tilt; two dogs (15%) did not recover facial motor function after 18 and 24 months; ipsilateral hemifacial contracture developed in six other dogs (46%) [including one of the cavalier King Charles spaniels]. The median time between the initial and last follow-up examination was 18 months (range, 6 to 42). ... Clinical Significance: Facial and vestibular neuropathy of unknown origin shares similarities with idiopathic facial paralysis. The prognosis for return of normal facial and vestibular function is guarded and there may be relapse after recovery."
Síndrome Vestibular em Animais de Companhia: estudo retrospetivo de 29 casos clínicos (Vestibular Syndrome in Small Animals: retrospective study about 29 clinical cases). Carolina Das Neves Campos Barata Gonçalves. Univ. of Lisbon. March 2016. Quote: "The vestibular system is the sensory system responsible for maintaining the animal’s balance relative to the gravitational field of the earth, and to adjust de position of the eyes, neck, trunk and limbs during the movement of the head. This system is divided in two functional components: the peripheral component, composed by the vestibulocochlear nerve (VIII) and its sensory receptors in the inner ear, and the central component, composed by the vestibular nuclei and pathways in the brainsteam and cerebellum. When one of these components is affected, the animal develops signs characterizing the vestibular syndrome. These clinical signs include loss of coordination and balance, falls, head tilt and positional strabismus, all to the side of the lesion, and pathologic nystagmus. The neurological examination allows to predict the location of the lesion and to clinically differentiate peripheral from central and paradoxical vestibular syndrome. This differentiation is important in determining the differential diagnoses, the diagnostic plan and also the prognosis and therapeutic plan. Several diseases could cause the onset of vestibular signs. The most common causes of peripheral vestibular syndrome are otitis media/interna and idiopathic vestibular syndrome, while the most common causes of central vestibular syndrome are inflammatory/ infectious diseases of the central nervous system and neoplasia. The practical component consists in a retrospective study of 29 clinical cases who presented at the clinic Referência Veterinária with signs of vestibular syndrome and were evaluated through magnetic resonance imaging. At the end of the study it was concluded that vestibular syndrome is a neurologic dysfunction who affects animals at any age, and it was confirmed that the most common etiologies described correspond to the observed at clinical practice. This study was important to understand that the use of magnetic resonance imaging is important at the evaluation of animals with central vestibular syndrome, and even with peripheral vestibular dysfunctions. There are some cases where the clinical signs used to differentiate the types of vestibular syndrome are subtle and can be attenuated by the administered drugs. Finally, it was also concluded that the neurological examination is a very reliable method to predict the location of the lesions and to differentiate between peripheral, central and paradoxical vestibular syndrome."
Vestibular Syndrome – Tilting, Rolling and Falling, Oh My! BVNS Neurotransmitter 2.0 Technically Speaking November 2016. Quote: “Vestibular Disease” is actually a misnomer. There are many diseases that can cause vestibular dysfunction, but since there are many causes (or in some cases a cause cannot be found), and there is not a consistent change in anatomy, it is incorrect to refer to it as a disease. It is referred to it as a syndrome - a collection of clinical signs often observed together; or simply “vestibular dysfunction”.
Facial Nerve Paralysis in Dogs: A Retrospective Study of 69 Cases. C. Ricco, L. Giraud, L. Cauzinille. 29th ESVN-ECVN Symposium. J. Vet. Int. Med. November 2016;30(6):1953. Quote: Facial paralysis is readily recognised in small-animal veterinary practice because of its manifestation of facial asymmetry; the idiopathic form has been previously reported to be present in 75% of dogs. The purpose of this study in dogs was to classify and determine the origin of facial nerve dysfunction using enhanced diagnostic procedures, including magnetic resonance imaging (MRI). The medical records of 69 dogs admitted for facial paralysis were reviewed. Neurological examination confirmed facial nerve abnormalities, which were all investigated with MRI. Idiopathic facial paralysis was diagnosed in 48% of dogs. Vestibular signs were the most common additional clinical signs and were observed in 36% of dogs with idiopathic facial paralysis. Peripheral nervous system disease was diagnosed in 19% of dogs, and central nervous system disease occurred in 30% of dogs. Two new predisposed breeds are added, the French bulldog and the Cavalier King Charles spaniel. Improved diagnostic methods enabled the diagnosis of a higher percentage of inflammatory/infectious diseases, which were absent in the central nervous system aetiologies of a previous similar study, and revealed metabolic (hypothyroidism), inflammatory and neoplastic aetiologies for peripheral nervous system disease.
Vestibular disease in dogs under UK primary veterinary care: epidemiology and clinical management. Sinziana Maria Radulescu, Karen Humm, Louis Mark Eramanis, Holger Volk, Dave C. Brodbelt, David B. Church, Dan G. O’Neill. BSAVA Congress 2019 proceedings; p. 502. Quote: Objectives: Vestibular disease, central and/or peripheral, can be a dramatic primary-care presentation. Current literature describes mostly referral caseloads. This study aimed to investigate the prevalence, presentation, management, and outcomes of vestibular disease in dogs in primarycare UK practices. Methods: The study explored the VetCompass™ primary-care database. Potential vestibular disease cases during 2016 were identified before manual verification and further information was extracted. Results: From 905,544 study dogs, 759 vestibular cases were confirmed giving an overall prevalence of 0.08% (95% CI 0.07–0.09%). Springer Spaniels had 3.74 (95% CI 2.97– 5.06, P < 0.001), Golden Retrievers 3.30 (95% CI 2.19– 4.97, P < 0.001), Border Collies 2.78 (95% CI 2.03–3.80, P < 0.001) and Cavalier King Charles Spaniels 2.70 (95% CI 1.90–3.84, P < 0.001) times the odds for vestibular disease compared with crossbreeds. Mean age at first diagnosis was 12 (SD: 3) years. The most common presenting signs were head tilt (69.8%), nystagmus (68.1%) and ataxia (64.5%). Central involvement was recorded in 14.1% cases. The most frequently used treatments were antiemetics (43.2%), corticosteroids (33.1%), antimicrobials (25%) and propentofylline (23.25%). Only 27/759 (3.6%) cases were referred. Improvement was recorded in 317/759 (41.8%) of the cases after a mean of 10 days from diagnosis. Of 232/759 (30.6%) deaths during the study period, vestibular disease contributed to death in 144/232 (62%). Statement (Conclusions): This study confirms low referral rates for vestibular disease cases, suggesting that primary-care data sources offer more generalisable information for benchmarking to help clinicians review their own clinical activities. Veterinarians should be aware of the strong breed predispositions identified here. (See August 2020 study's abstract below.)
Clinical signs, MRI findings and outcome in dogs with peripheral vestibular disease: a retrospective study. Rocio Orlandi, Rodrigo Gutierrez-Quintana, Beatrice Carletti, Camilla Cooper, Josep Brocal, Sara Silva, Rita Gonçalves. BMC Vet. Res. May 2020; doi: 10.1186/s12917-020-02366-8 Quote: Background: Vestibular dysfunction is relatively common in dogs, with a prevalence of 0.08% reported in primary veterinary care in the UK. There are several studies investigating how to differentiate between peripheral and central vestibular disease but only limited information regarding the possible underlying causes for peripheral vestibular dysfunction in dogs. This study therefore aimed to describe the clinical signs, magnetic resonance imaging findings (MRI), underlying causes and outcome in a large population of dogs diagnosed with peripheral vestibular disease. Results: One hundred eighty-eight patients were included in the study with a median age of 6.9 years (range 3 months to 14.6 years). ... The most commonly affected breeds were the Cavalier King Charles spaniel (n = 38, 20%), Boxer (n = 22, 12%), Cocker spaniel (n = 21, 11%), Labrador (n = 11, 6%), French bulldog (n = 9, 5%) and English springer spaniel (n = 8, 4%). ... Neurological abnormalities included head tilt (n = 185), ataxia (n = 123), facial paralysis (n = 103), nystagmus (n = 97), positional strabismus (n = 93) and Horner syndrome (n = 7). The most prevalent diagnosis was idiopathic vestibular disease (n = 128), followed by otitis media and/or interna (n = 49), hypothyroidism (n = 7), suspected congenital vestibular disease (n = 2), neoplasia (n = 1) and cholesteatoma (n = 1). Long-term follow-up revealed persistence of head tilt (n = 50), facial paresis (n = 41) and ataxia (n = 6) in some cases. Recurrence of clinical signs was observed in 26 dogs. Increasing age was associated with a mild increased chance of diagnosis of idiopathic vestibular syndrome rather than otitis media and/or interna. History of previous vestibular episodes was associated with an increased likelihood of resolution of the clinical signs whilst contrast enhancement of cranial nerves VII and/or VIII on MRI was associated with a decreased chance of resolution of the clinical signs. Conclusions: Idiopathic vestibular disease is the most common cause of peripheral vestibular dysfunction in dogs and it is associated with advanced age. Incomplete recovery from peripheral vestibular disease is common, especially in dogs presenting with cranial nerve enhancement on MRI but less so if there is previous history of vestibular episodes.
Vestibular disease in dogs under UK primary veterinary care: Epidemiology and clinical management. Sinziana Maria Radulescu, Karen Humm, Louis Mark Eramanis, Holger A. Volk, David B. Church, David Brodbelt, Dan Gerard O'Neill. J. Vet. Intern. Med. August 2020; doi: 10.1111/jvim.15869. Quote: Background: Vestibular disease (VD), central or peripheral, can be a dramatic primary-care presentation. Current literature describes mostly dogs examined in referral centers. Hypothesis/Objectives: Describe the prevalence, presentation, clinical management, and outcomes of VD in dogs under primary veterinary care at UK practices participating in VetCompass. Animals: Seven hundred and fifty-nine [759] vestibular cases identified out of 905,544 study dogs. Methods: Retrospective cohort study. Potential VD cases clinically examined during 2016 were verified by reviewing clinical records for signalment, presenting clinical signs, treatments, and outcomes. Multivariable logistic regression was used to evaluate factors associated with VD. Results: The overall prevalence of VD was 8 per 10,000 dogs. Median age at first diagnosis was 12.68 years. Compared with crossbreeds, breeds with the highest odds of VD diagnosis included French Bulldogs, Bulldogs, King Charles Spaniels, Cavalier King Charles Spaniels, and Springer Spaniels. ... CKCS are known to be predisposed to several neurological syndromes that can cause vestibular signs, including occipital hypoplasia/syringomyelia, granulomatous meningoencephalomyelitis (GME), and VD. Moreover, CKCS have a tendency toward cerebrovascular disease, particularly rostral cerebellar artery infarction. In immature dogs, the first presenting sign of syringomyelia could be scoliosis, which can appear similar to a head tilt of vestibular origin. VD in CKCS can be also idiopathic -- CKCS is one of the most commonly seen breeds with idiopathic facial nerve paralysis and facial and vestibular neuropathy of unknown origin. Aside from central and IPVD, CKCS are also predisposed to primary secretory otitis media, known to commonly be associated with peripheral VD. ... The most common presenting signs were head tilt (69.8%), nystagmus (68.1%), and ataxia (64.5%). The most frequently used treatments were antiemetics (43.2%), systemic glucocorticoids (33.1%), antimicrobials (25%), and propentofylline (23.25%). There were 3.6% of cases referred. Improvement was recorded in 41.8% cases after a median of 4 days. Conclusions: Our study identifies strong breed predispositions for VD. The low referral rates suggest that primary-care data sources offer more generalizable information for benchmarking to help clinicians review their own clinical activities.
Clinical reasoning in canine vestibular syndrome: Which presenting factors are important? Eleanor Harrison, Nick J. Grapes, Holger A. Volk, Steven De Decker. Vet. Rec. February 2021; doi: 10.1002/vetr.61. Quote: Background: Although the use of clinical reasoning has been evaluated for several neurological presentations, this approach has not yet been investigated for dogs with vestibular syndrome. Methods: Two hundred and thirty‐nine dogs presenting with vestibular syndrome were included in this retrospective study. ... The Cavalier King Charles spaniel was the most common breed (n = 26 dogs) [11%]. ... Univariate analysis of variables (clinical history, signalment, clinical presentation and neurological examination findings) was performed. Variables with p < 0.3 were selected for logistic regression. Results: Ninety‐five percent of dogs were represented by eight conditions: idiopathic vestibular disease (n = 78 dogs), otitis media interna (n = 54), meningoencephalitis of unknown origin [MUO] (n = 35), brain neoplasia (n = 26), ischaemic infarct (n = 25), intracranial empyema (n = 4), metronidazole toxicity (n = 3) and neoplasia affecting the middle ear (n = 3). Idiopathic vestibular disease was associated with higher age, higher bodyweight, improving clinical signs, pathological nystagmus, facial nerve paresis, absence of Horner's syndrome and a peripheral localisation. Otitis media interna was associated with younger age, male gender, Horner's syndrome, a peripheral localisation and a history of otitis externa. Ischaemic infarct was associated with older age, peracute onset of signs, absence of strabismus and a central localisation. Conclusions: Discrete clinical features can be used to identify the most likely diagnosis in dogs with vestibular syndrome.
The Use of Ondansetron for the Treatment of Nausea in Dogs With Vestibular Syndrome. S. Foth, Sebastian Meller, Hannah Kenward, J. Elliot, L. Pelligand, Holger Andreas Volk. Research Square. March 2021; doi: 10.21203/rs.3.rs-279349/v1. Quote: Background: Vestibular syndrome is often accompanied by nausea. Drugs currently approved for its treatment have been developed to stop vomiting but not nausea. The efficacy of 5‑HT3 receptor antagonists to reduce nausea has been described for chemotherapy, but not for nausea secondary to vestibular disorders. Methods: Sixteen dogs with vestibular syndrome-associated nausea were included in the open-label, multicentric study. ... (Golden Retriever [n = 4], mix breeds [n = 2], and one of each of Australian Shepherd, Beagle,Boxer, Chihuahua, Cocker Spaniel, French Bulldog, Irish Soft coated Wheaten Terrier, Lurcher, Malinois and Yorkshire Terrier). ... The intensity of nausea-like behaviour was analysed before ondansetron administration (0.5 mg/kg i.v.) and 2 h afterwards, using a validated 5-point-scale. The occurrence and frequency of salivation, lip licking, restlessness, vocalisation, lethargy, and vomiting were assessed. Results: All dogs initially showed signs of nausea, whereas only 31% showed vomitus. The intensity of nausea was significantly reduced in all dogs 2 h after ondansetron administration, including the clinical signs of nausea analysed in 11 dogs (salivation, lip licking, restlessness , and lethargy) except for vocalisation. Conclusion: The results provide preliminary evidence of the potential benefit of ondansetron in the treatment of nausea, which was present in all examined dogs. Vomiting was only observed in 5 dogs indicating that nausea can occur separately and should not be perceived only as a preceding stimulation of the vomiting centre.
Ondansetron in dogs with nausea associated with vestibular disease: A double-blinded, randomized placebo-controlled crossover study. Lea Henze, Sarah Foth, Sebastian Meller, Friederike Twele, Marios Charalambous, Hannah Kenward, Jonathan Elliott, Ludovic Pelligand, Holger A. Volk. J. Vet. Intern. Med. July 2022; doi: 10.1111/jvim.16504. Quote: Background: Nausea and emesis can be, among other signs, common manifestations of acute vestibular system dysfunction in dogs. Currently, antiemetic drugs, such as maropitant and metoclopramide, are used commonly, but do not appear to control nausea. A non-placebo-controlled preliminary study suggested good efficacy of 5-HT3-receptor antagonists, such as ondansetron, against nausea in dogs with vestibular syndrome. Objectives: To assess and confirm the effect of ondansetron on behavior suggestive of nausea in dogs with vestibular syndrome. Animals: Fourteen dogs with vestibular syndrome and clinical signs of nausea presented to a neurology service. Methods: Placebo-controlled, double-blinded, crossover study. Behavioral assessment was performed hourly for 4 hours using an established numerical rating scale. The criteria salivation, lip licking, vocalization, restlessness, lethargy, and general nausea were scored. The occurrence of emesis was recorded. After scoring at T0 (pre-dose) and T2 (2 hours post-dose) either ondansetron (0.5 mg/kg) or placebo was injected IV. Two hours post-dose, treatments were switched. Blood samples were collected to measure serum arginine vasopressin (AVP) concentration, which previously has been shown to correlate with clinical signs of nausea. Results: Clinical resolution of nausea was observed 1 hour after administration of ondansetron, whereas serum AVP concentration decreased 4 hours after ondansetron administration. Conclusion and clinical importance: Administration of ondansetron IV is beneficial for dogs with nausea secondary to acute vestibular syndrome. Ondansetron substantially and rapidly decreased clinical signs of nausea behavior and stopped emesis.
Clinical features and outcome of 10 dogs with suspected idiopathic vestibular epilepsy. Tania Al Kafaji, Fabio Tocco, Samuel Okonji, Antonella Gallucci. J. Vet. Intern. Med. March 2024; doi: 10.1111/jvim.17046. Quote: Background: In humans, vestibular epilepsy (VE) is described as focal seizures with transient signs of vestibular disease. In dogs, 2 cases of vestibular episodes, called vestibular paroxysmia, are reported. Hypothesis/objectives: The objective of this study was to define the clinical features, phenotypical manifestation, and outcome of suspected VE in dogs. Animals: Ten dogs with recurrent vestibular episodes [including 5 pugs and 1 cavalier King Charles spaniel]. Methods: Retrospective study. Medical records between 2009 and 2023 were reviewed, and dogs with a normal neurological examination, a history of transient signs of vestibular disease, absence of abnormalities detected on blood exams and brain magnetic resonance imaging (MRI) or computed tomography (CT), besides a minimum 10-month follow-up were included. Clinical improvement was defined as a ≥50% reduction in frequency or the cessation of clinical signs after the onset of antiseizure medications (ASMs). Results: Pugs were the most prevalent breed (5/10; 50%). In 2 cases, additional generalized tonic-clonic (GTC) seizures were reported. MRI exam was performed in most cases (9/10; 90%), whereas 1 dog underwent a CT scan (1/10; 10%). Electroencephalography (EEG) was carried out in 3 dogs that showed interictal spikes in the fronto-temporal and fronto-parietal areas. All cases received ASMs, with clinical improvement in 10/10 dogs (100%). Conclusion and clinical importance: The presence of GTC seizures, EEG interictal spikes, and responsiveness to ASMs supported the hypothesis of an epileptic origin of vestibular episodes and thus the existence of VE in these dogs, with a presumed idiopathic cause and apparent favorable outcome.

 What
It Is
What
It Is
CONNECT WITH US