Cherry Eye and the
Cavalier King Charles Spaniel
Some cavaliers may develop "prolapsed gland of nictitans", also known as
"cherry eye". Cavaliers are not predisposed to cherry eye, but the
Beagle, Boston terrier, bulldogs, Cocker spaniel, and Lhasa Apso are.
What It Is
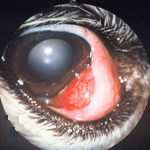 The nictitating membrane is the dog's third eyelid, a small triangular
flap of cartilage in the inner corner of the eye, which covers a tear
gland. If and when the gland should flip upward (prolapses), it becomes
inflamed and protrudes and bulges over the third eyelid, giving the
appearance of a reddish cherry. (See a CKSC's cherry eye,
at left.) While the appearance of cherry eye is disturbing, it
usually is not painful to the dog. Nevertheless, cherry eye should be
treated promptly, because it may lead to chronic irritation of the
cornea, conjunctiva, and dry eye
(keratoconjunctivitis sicca or KCS).
The nictitating membrane is the dog's third eyelid, a small triangular
flap of cartilage in the inner corner of the eye, which covers a tear
gland. If and when the gland should flip upward (prolapses), it becomes
inflamed and protrudes and bulges over the third eyelid, giving the
appearance of a reddish cherry. (See a CKSC's cherry eye,
at left.) While the appearance of cherry eye is disturbing, it
usually is not painful to the dog. Nevertheless, cherry eye should be
treated promptly, because it may lead to chronic irritation of the
cornea, conjunctiva, and dry eye
(keratoconjunctivitis sicca or KCS).
RETURN TO TOP
Diagnosis
Cherry eye is easily diagnosed by visual observation. The bulging inflamed gland at the corner of the eye is obvious.
RETURN TO TOP
Treatment
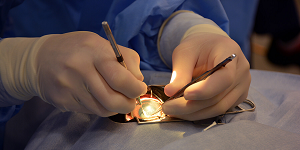
Cherry eye usually requires surgical treatment. In rare, mild instances,
the ophthalmologist may be able to relocate the gland into its proper
position without surgery.
This procedure is most effective if
performed as soon as the cherry eye is discovered. So, it is recommended
that the dog be taken to the eye specialist
 immediately upon noticing
the condition is first noticed.
immediately upon noticing
the condition is first noticed.
The most preferable of the two surgical options is to re-position the gland back into its normal location and then suturing it to enable the gland to remain in that position. The second surgical option is to remove the gland. In some instances, that is the only effective choice. Unfortunately, a high percentage of gland-removal surgeries result in the loss of the eye’s tear-producing ability, causing dry eye.
RETURN TO TOP
Research News
August 2015: Dutch study finds post-operative reoccurrence of cherry eye is linked to other eye disorders. In a July 2015 doctoral thesis at Utrecht University, the Netherlands, Dr. Karin Stegmeijer examined the results of two different types of surgeries to correct cherry eye on 157 dogs, including 6 cavalier King Charles spaniels. She found no significant difference in the results of the two surgical techniques. However, she also observed a definite correlation between the presence of additional eye problems and the rate of reoccurrence of cherry eye after a corrective surgery.
The study also showed that 19.1% of the dogs had additional eye problems like dry eye, macroblepharon, entropion, ectropion, trichiasis, or distichiasis, prior to developing cherry eye.
RETURN TO TOP
Related Links
Veterinary Resources
Retrospective study of 155 cases of prolapse of the nictitating membrane gland in dogs. S. Mazzucchelli, M. D. Vaillant, F. Wéverberg, H. Arnold-Tavernier, N. Honegger, G. Payen, M. Vanore, L. Liscoet, O. Thomas, B. Clerc, S. Chahory. Vet.Rec. Apr. 2012;170:443. Quote: "A retrospective study of 155 cases (114 dogs). The breed, sex and age at the time of the first and opposite onset of nictitans gland prolapse were recorded. Long-term follow-up with a minimum of one-year duration was performed by telephone conversations. One hundred and fourteen dogs representing 155 nictitans gland prolapses were included [including 5 cavalier King Charles spaniels]. 75.4 per cent of the first prolapse occur before one year of age. Unilateral nictitans gland prolapse was observed in 64 per cent of cases. When the condition was bilateral, it occurred simultaneously in 41.4 per cent. When it was bilateral but not simultaneous (24/41), the opposite gland prolapse occurred within three months in 70.8 per cent of the cases. Five breeds were most commonly affected by the bilateral condition: French bulldog, shar pei, great dane, English bulldog and cane corso."
Comparison between the conventional and a modified Morgan “pocket technique” for the treatment of prolapsed nictitans gland (“cherry eye”) in dogs. Karin Stegmeijer. Utrecht Univ. thesis. July 2015. Quote: "Purpose: The aim of this study was to determine whether a modified surgical technique for nictitans gland prolapse (NGP) correction resulted in a significant decreased number of NGP reoccurrences, as compared to the number of reoccurrences after the ”regular” Morgan pocket technique. Furthermore, we aimed to find out if other factors concerning the ocular condition or the surgery, such as additional eye disease or the surgeon’s experience, influenced the number of reoccurrences. Methods: A total of 157 dogs with unilateral or bilateral hyperplasia of the gland of the nictitating membrane participated in this study, consisting of thirty-nine different dog(cross)breeds [including 6 cavalier King Charles spaniels -- 3.8%]. The total number of eyes that were diagnosed and operated on was 256. All eyes were treated surgically prior to this study, either by using the regular Morgan pocket technique (n=125) or using the modified pocket technique (n=131) in the period from March 1994 until April 2010 at ‘Het Medisch Centrum voor Dieren’ in Amsterdam or at the ‘University Clinic for Companion Animals’ in Utrecht. All owners with dogs were asked by telephone to participate in this study. If they were willing to participate, a questionnaire was verbally conducted through the telephone. The data collected from the questionnaires was statistically analyzed with the Chi-square test and the Likelihood Ratio test to determine a possible significant difference in reoccurrence between the two surgical techniques and to asses if certain variables could possibly influence the rate of reoccurrence. Results: The surgical technique used to correct NGP was in 48.8% (n=125) cases the “regular” Morgan pocket technique and in 51.2% (n=131) cases the modified pocket technique. The Morgan pocket technique had nineteen (=15.2%) reoccurrences and the modified pocket technique had fifteen reoccurrences (=11.5%). Of the 256 eyes that were diagnosed with NGP and were operated on, 19.1% had additional eye problems like kerato-conjunctivitis sicca (7%), macroblepharon (2%), tear quality problems (0.8%) or follicular conjunctivitis (0.8%). 12.9% had ‘other’ eye problems like entropion, trichiasis, distichiasis or ectropion. There were six different veterinary eye specialists or residents that operated the dogs with NGP in this study. Their experience (in days) was calculated for each particular NGP surgery. The average number of days of experience for NGP that had a reoccurrence is 4449.9 with a standard deviation of 4482.8 days (minimum=90 days and maximum=12317 days). The average number of days of experience for NGP that did not have a recurrence is 4726.0 with standard deviation of 4312.2 days (minimum=90 days and maximum=11204 days). After the dogs had undergone NGP surgery, 90.5% of the dog owners were satisfied about the results, 3.8% were dissatisfied and 5.7% did not give a conclusive answer. Conculsions: Results demonstrated no significant difference in the rate of reoccurrence between the two surgical techniques (p-value=0.377). Furthermore, the statistical analysis concluded that surgical experience of the veterinary ophthalmologist did not have an effect on the reoccurrence of NGP. This study did show that there is a link between the number of reoccurrences and the presence of additional eye disease. ... This study showed that 19.1% of the dogs had additional eye problems like KCS, macroblepharon, entropion, ectropion, trichiasis or distichiasis, prior to developing NGP. This study proved a correlation between the presence of additional eye problems and the rate of reoccurrence of NGP after a corrective surgery."
An Evidence-Based Rapid Review of Surgical Techniques for Correction of Prolapsed Nictitans Glands in Dogs. Constance White, Marnie L. Brennan. Vet. Sci. September 2018;5(3):75. Quote: Prolapsed nictitans gland (PNG) is an important ocular condition of dogs. Various surgical interventions have been described, but effective technique is currently considered to be a matter of personal clinician preference. The aim of this rapid review was to evaluate existing peer-reviewed evidence of effectiveness for surgical techniques and their subsequent effects on quantitative and clinical lacrimal outcomes for PNG. We performed a structured bibliographic search of CAB Abstracts, PubMed, and Medline using terms relevant to dogs, nictitans gland, and surgery on 13 September 2017. Included studies were assessed for study design, reporting characteristics, surgical techniques, and surgical and lacrimal outcomes. Fifteen of three hundred fifteen identified studies were eligible for inclusion. Seven different replacement techniques were identified, along with gland excision. All studies were observational or descriptive, with the exception of a single crossover trial. Outcomes reporting was heterogeneous and provided limited detail on lacrimal outcomes or on breed propensity for recurrence. Insufficient data precluded comparison of techniques for either surgical failure rates or lacrimal outcomes, although proportional meta-analysis yielded an overall failure rate of 3% (95% CI 1–7%) for the Morgan’s pocket procedure. Improved reporting of veterinary surgical studies will improve evidence appraisal and synthesis, as well as reduce potential sources of bias.


CONNECT WITH US