Immune-Mediated Polyarthritis (IMPA)
in the Cavalier King Charles
Spaniel
-
 What It Is
What It Is - Symptoms
- Diagnosis
- Treatment
- What You Can Do
- Research News
- Related Links
- Veterinary Resources
Immune-mediated polyarthritis (IMPA) is an idiopathic form of arthritis, causing recurring episodes of lameness and joint swelling, usually in mulitple joints. It is a commonly diagnosed inflammatory disease in dogs and has been reported in cavalier King Charles spaniels in at least five published veterinary journal articles.
What It Is
IMPA can be “erosive” or “non-erosive. The erosive condition is known
as rheumatoid arthritis (RA). The non-erosive type is
called idiopathic because there is no evidence of any primary disease
nor any serological
 (blood serum) evidence regarding its immunological
properties.
(blood serum) evidence regarding its immunological
properties.
Forms of polyarthritis in dogs have been classified into four types:
Type I: Uncomplicated Arthritis: polyarthritis with none of the associations reported in the other types. This also is referred to as idiopathic IMPA or primary IMPA.
Type II: Reactive Arthritis: Polyarthritis associated with an infective disease process remote from the joints, such as a respiratory or urinary tract infection. This also is referred to as systemic inflammation or infection.
Tpye III: Enteropathic Arthritis: polyarthritis associated with gastro-intestinal disease; such as gastro-enteritis, ulcerative colitis
Type IV: Neoplastic Related Polyarthritis: polyarthritis associated with neoplastic disease remote from the joints.
RETURN TO TOP
Symptoms
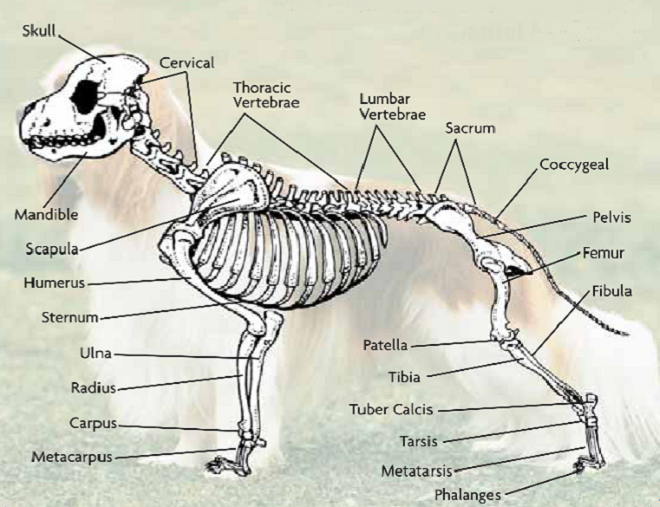
Polyarthritis produces swelling and tenderness at one or more of the affected dog's joints. The main symptoms are joint pain, stiffness, lameness. The affected dog also likely will have a high fever and appear anorexic and/or lethargic. In some cases, the dog has no swelling or lameness but shows signs of a vague systemic illness.
The most commonly affected joints are the carpal (wrist), tarsal (hock), stifle (knee joint), and elbow.
Non-erosive IMPA typically also produces lesions (open sores) on the skin near the affected joints.
Erosive IMPA lesions can result in damage to the soft-tissues which
support the affected joints, and also the
 bones at those joints. Dogs
with erosive IMPA may develop unstable joints due to damage or
destruction of the soft-tissue structures.
bones at those joints. Dogs
with erosive IMPA may develop unstable joints due to damage or
destruction of the soft-tissue structures.
In a November 2016 article, a team of Wisconsin and Michigan researchers studied the clinical records of 79 dogs diagnosed with immune-mediated polyarthritis (IMPA). Of those 79 dogs, 13 had erosive IMPA, of which, two were cavalier King Charles spaniels. The 13 affected dogs had erosive lesions in their carpal joints. The estimated median synovial fluid lymphocyte count for dogs with erosive IMPA was significantly greater than that for dogs with nonerosive IMPA. Results indicated erosive IMPA most commonly affected the carpal joints of middle-aged small-breed dogs. (See from this article, at above left, the carpus of an 8-year-old spayed female Cavalier King Charles Spaniel with subjectively moderate subchondral bone lysis accompanied by severe synovial swelling -- in x-ray at right.)
 Courtesy of The Dog Channel
Courtesy of The Dog Channel
RETURN TO TOP
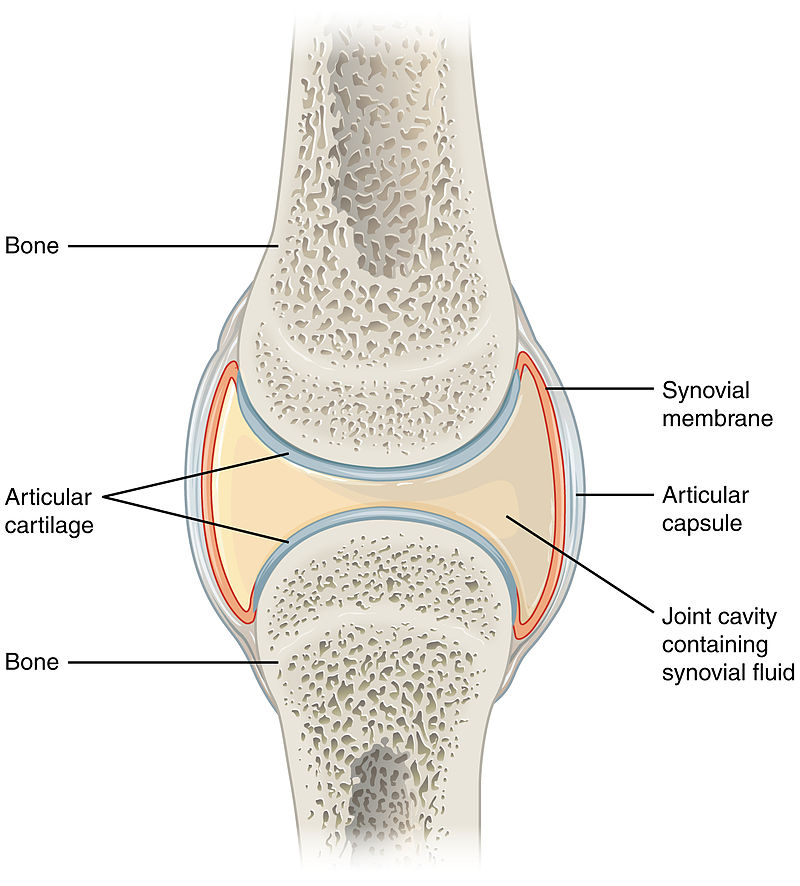
Diagnosis
Several procedures normally are performed to diagnose IMPA, the primary one being the collection and examination of fluid samples from the sac of the synovial membrane situated at the affected joints. Biopsies of the synovial membrane, muscle, and skin also may be taken.
X-rays (radiographs) of the affected joints, chest, and abdomen will be taken, especially to determine if any bone damage or loss has occurred. X-rays are used to look for changes in the joints which would indicate that the IMPA is erosive rather than non-erosive.
Apart from x-rays of joints, a main reason for performing x-rays and other diagnostic imaging (ultrasound, CT scans) with IMPA is to ensure they can be safely immunosuppressed and any possible causes of secondary IMPA have been ruled out. Chest x-rays, looking for related disorders, have been found to not be useful in most cases.
Ultrasounds of the abdomen may be performed, searching for related disorders. As with chest x-rays, these have not been found useful in most cases.
Blood serum and other testing should be performed to determine the presence of, or rule out, other causes such as bacterial infections. Urinalysis may be performed, to screen for the presence of proteinuria, a common abnormality found in dogs otherwise diagnosed with non-erosive IMPA, according to this May 2022 article.
RETURN TO TOP
Treatment
Treatment may vary depending upon the type of IMPA. Typically, drugs to suppress the immune system, such as leflunomide or prednisone, are the drugs of choice to deal with primary IMPA (Type I) inflammation at the joints, with dosages increased if necessary.
If evidence of infections have been identified (Type II), antibiotics will be administered.
Cytotoxic drugs, which affect the growth and action of some cells that cause joint pain, swelling, and damage due to arthritis, likely will be prescribed, particularly if the IMPA is resistant to prednisone. They include cyclophosphamide (Cytoxan), azathioprine (Imuran), and methotrexate (Rheumatrex, MTX, Amethopterin). Cytotoxic drugs rarely are used for more than 8 weeks and require periodic monitoring of blood cell counts.
Medications which may be prescribed include NSAIDs (nonsteroidal anti-inflammatory drugs), which are designed to relieve pain and reduce inflammation. An NSAID growing in popularity for treating arthritis in dogs is grapiprant (Galliprant). A COX-2 selective NSAID, enflicoxib, has been found in a September 2021 study to be effective when administered orally. See, also, this February 2024 article regarding the safetly and efficacy of long-term use of enflicoxib. Other NSAIDs include Loxicom (Meloxicam). NSAIDs are known to have potentially harmful side effects, including gastrointestinal (vomiting, diarrhea, ulceration) and affecting kidney functions.
Polysulfated glycosaminoglycan (PSGAG) (Adequan) is injected into the muscles to relieve pain and inflammation and improve range of motion due to arthritis in dogs. Studies have found that it prevents catabolic enzymes from degrading cartilage and bone, the causes of arthritis. PSGAG has been approved by the US Food & Drug Administration (FDA) for the management of OA in dogs.
Amantadine (Endantadine, Gocovri, Osmolex ER, Symmetrel), is an N-methyl-d-aspartate antagonist (NMDA), which is used for control of the symptoms of Parkinson's disease in humans, together with gabapentin or pregabalin. Amantadine is believed to release brain dopamine from nerve endings making it more available to activate dopaminergic receptors. See this January 2008 article, in which the researchers found clinical improvement in dogs with chronic osteoarthritis pain when amantadine was used in combination with meloxicam. See Dr. Rusbridge's YouTube video on this drug.
Pentosan polysulfate sodium (Zydax) reportedly will reduce inflammation and slow the progression of arthritic damage to cartilage. It is injected every 4 weeks and has shown effectiveness within 6 weeks. Currently it is available for treating dogs only in New Zealand and Australia.
Bedinvetmab (Librela, Beransa) is a injectable solution to alleviate pain
associated with osteoarthritis (OA) in dogs. It is administered monthly.
It is a monoclonal antibody which binds to and targets
Nerve Growth
Factors (NGF), which have key involvement in OA pain. It is manufactured
by Zoetis. In May 2023, Zoetis announced that the USA Food & Drug
Administration approved Librela (bedinvetmab injection) for the control
of pain associated with osteoarthritis (OA) in dogs. Zoetis stated in
its press release that Librela is the first and only once-monthly,
anti-NGF monoclonal antibody treatment for canine OA pain and is
approved as
 safe and effective in providing long-term control of OA pain
symptoms in dogs, which can improve their mobility and overall quality
of life. Librela does not reduce inflammation or improve joint function.
It just masks feeling the pain associated with those conditions.
safe and effective in providing long-term control of OA pain
symptoms in dogs, which can improve their mobility and overall quality
of life. Librela does not reduce inflammation or improve joint function.
It just masks feeling the pain associated with those conditions.
Nevertheless, bedinvetmab is the subject of controversy due to reports of unanticipated adverse reactions, including ataxia, hind-end weakness, inability to walk, new or worsened seizures, pancreatitis, and organ damage. Among expressed concerns are that blocking NGF may prevent its known protective and reparative roles elsewhere in the body. See this May 2015 article and this October 2023 article.
Veterinary neurologist Dr. Curtis Dewey, who is conducting an investigation into the adverse reactions caused by bedinvetmab, makes this recommendation as of February 2025:
"This drug is for dogs with radiographically documented osteoarthritis (OA). This drug should not be administered to dogs with pre-existing neurologic disorders. All dogs for whom this drug is to be considered should have a neurologic examination performed first. In older dogs (9 years and up), a cognitive questionnaire should be completed by the pet parent to evaluate for potential cognitive dysfunction prior to injection."
See this May 2025 article in which reported:
"This study reveals a striking disparity in musculoskeletal adverse event reports to Librela compared to six comparator drugs. Ligament/tendon injuries, polyarthritis, fractures, musculoskeletal neoplasia, and septic arthritis were reported nine times more frequently in Librela-treated dogs. Worryingly, since its European release, Librela has accumulated 20 times more reports than the highest-ranking comparator drug (Rimadyl) and three times more than all comparator drugs combined over a 20-year period. Furthermore, independent expert review of a subset of cases strongly supported a causal association between Librela and accelerated joint destruction. ... Given NGF’s diverse roles and prior evidence of RPOA, subchondral bone fractures, and atraumatic joint luxations in humans and animals, bedinvetmab-associated MSAEs are an expected consequence of NGF inhibition."
 See also this
July 2025 commentary on the May 2025 article, and this
August 2025 article. In an August 2025 post on Facebook by the
owner of a cavalier, Sam, she reported that he experienced rapidly progressive osteoarthritis (RPOA),
attributed to Librela and ended up having major arthrodesis (joint
fusion) surgery
(right) to remove his ankle joint and pin and plate his leg so that
he could walk again. Sam was originally prescribed Librela for
elbow dysplasia.
See also this
July 2025 commentary on the May 2025 article, and this
August 2025 article. In an August 2025 post on Facebook by the
owner of a cavalier, Sam, she reported that he experienced rapidly progressive osteoarthritis (RPOA),
attributed to Librela and ended up having major arthrodesis (joint
fusion) surgery
(right) to remove his ankle joint and pin and plate his leg so that
he could walk again. Sam was originally prescribed Librela for
elbow dysplasia.
Before even considering having an arthritic dog injected with bedinvetmab (Librela, Beransa), check out the current information on the Pet Advocate website about this drug.
Synovetin OA is a "conversion electron therapeutic veterinary device" which is injected into the dog's elbow joints which are afflicted with osteoarthritis to reduce pain and inflammation of the synovial membrane which lines the elbow (synovitis).
Krill oil has antioxidant and anti-inflammatory effects of omega-3 polyunsaturated fatty acids (PUFAs). It has been found to provide pain relief in dogs with OA without any adverse effects.
Palmitoylethanolamide (PEA) is a
N-acylethanolamine molecule in a family of long-chain fatty acid
 amides
called ALIAmides. PEA has been found in rat and mice studies to limit
hyperactvity in immune cells and thereby control inflammatory responses
and resulting tissue damage. PEA is produced by the animal's body as
needed in response to certain types of injuries. PEA is a product of
normal fatty acid synthesis from palmitic acid. It is found in many
common foods, particularly palm oil, soy beans, egg yolks, and peanuts.
The commercial version is most commonly manufactured from palm oil*.
amides
called ALIAmides. PEA has been found in rat and mice studies to limit
hyperactvity in immune cells and thereby control inflammatory responses
and resulting tissue damage. PEA is produced by the animal's body as
needed in response to certain types of injuries. PEA is a product of
normal fatty acid synthesis from palmitic acid. It is found in many
common foods, particularly palm oil, soy beans, egg yolks, and peanuts.
The commercial version is most commonly manufactured from palm oil*.
Not all PEA is alike. There are at least 4 types of PEA, and the differences of those 4 are described below here. The differences are mainly the sizes of the particles. The larger the size of particle, the less soluble and less bioavailable. Micronization reduces the size of the particles of PEA. In short, since the basic (naïve) PEA is almost totally insoluble in water and therefore has very poor bioavailability, researchers use micronized or ultra-micronized PEA or water-dispersible PEA in their published studies.
• Basic PEA, called "naïve PEA", is almost totally insoluble in water and under gastrointestinal conditions and therefore the oral intake of it (rather than being injected directly into the abdomen) has very poor bioavailability, meaning that it does not get absorbed well in the dog's gut. See this May 2021 article and this July 2025 article.
• Micronized PEA (m-PEA or micro-palmitoylethanolamide) is a patented technique that reduces the diameter of PEA particles, making them absorbable in the intestine, which has been found to be more effective than ordinary basic PEA in activating PEA levels in blood plasma in dogs. See this August 2014 article.
• Ultra-micronized PEA (um-PEA), also patented, reduces the PEA particle size further, to enable it to cross the blood-brain barrier, likewise has been found to be much more effective than basic PEA. See this August 2014 article.
• Water-Dispersible PEA (PEA-WD), also patented, reduces the PEA to a powder which can be dispersed in cold water. It has been found to be 16 times more effective than basic PEA. See this July 2025 article.
• Hybrid versions of PEA: Additionally, PEA has been combined with other ingredients and used in some published studies. These include FenuMat-PEA (P-fen), which is a PEA hybrid combined with the herb fenugreek (trigonella foenum-graecum), and hybrids combined with resveratrol, quercetin, fisstin, and boswellic acid. See this July 2025 article.
PEA micronization and ultra-micronization are patented (by Italian company, EPITECH Group SpA) processing techniques that reduce the diameter of the PEA particle to a micronized or ultra-micronized size which optimizes the PEA's absorbability along the intestine. Micronization increases the drug's surface area, thereby improving its dissolution rate and minimizing its absorption difficulties. The ultra-micronized size also enables the PEA to cross the blood-brain barrier. See this February 2021 article.
 If a PEA product is not advertised as being micronized or
ultra-micronized, then
Dr. Clare Rusbridge advises that
"You
probably are wasting your money."
A variety of brands of
micronized and ultra-micronized PEA are offered on-line.
If a PEA product is not advertised as being micronized or
ultra-micronized, then
Dr. Clare Rusbridge advises that
"You
probably are wasting your money."
A variety of brands of
micronized and ultra-micronized PEA are offered on-line.
As for dosages, the studies using micronized PEA, the range was from 10 to 15 mg/kg/day, and the range for ultra-micronized was 24 mg/kg (for osteoarthritis in humans).
There are no published veterinary journal articles about treating canines with PEA for osteoarthritis (OA). This is very limited research regarding a combination of ultramicronized PEA (um-PEA) and quercetin (PEA-Q), first in rats and finally in dogs.
The rat research has been an August 2017 article. The authors report that a combination of ultramicronized PEA and quercetin (PEA-Q), given orally to 10 rats. They reported:
"PEA-Q is a novel co-ultramicronized formulation of PEA and quercetin whose effects were investigated in two pre-clinical models of OA pain in rats. Oral administration of PEA-Q decreased pain sensitivity, improved locomotor function, reduced inflammatory signs and mediators and lowered histological damage score."
In that article, the authors go to great lengths to suggest that their "collective observations presented here propose that PEA-Q shows promise for multimodal pain management in canine and feline OA."
In a September 2018 report, 13 dogs diagnosed with chronic OA and lameness received supplements of PEA-Q for four weeks, at the rate of 24 mg/kg per day. Pain scores were taken, showing successful improvement in 7 of the dogs by the second week. Lameness also reportedly improved durint the treatment period.
Nevertheless, at least one PEA vendor advertises that PEA alone (meaning, not even ultramicronized PEA and not combined with quercetin) "may be beneficial for ... Osteoarthritis pain". So, Buyer Beware. See more about this type of hazard below.
PEA's fellow ALIAmide, micronized palmitoyl-glucosamine (m-PGA), has been teamed with curcumin (m-PGA-Cur) to treat dogs with osteoarthritis. In an October 2020 report of 181 dogs diagnosed with OA, they were given m-PGA-Cur for 2 months in addition to their conventional medications. The dogs were scored for lameness and pain at the start of the study and each 30 days thereafter, along with having the dogs' owners evaluate their dogs' mobility impairment and pain behaviors. At the end of the study, 74% of the owners scored their dogs' quality of life as improved, and 87% of the 27 participating veterinarians expressed satisfaction with the addition of m-PGA-Cur in the daily management of the OA. This was not a controlled clinical trial, however.
In a February 2023 article, m-PGA and curcumin again were teamed (m-PGA-Cur) to treat 58 dogs having chronic OA pain. All of the dogs had been treated with meloxicam and continued to do so during the 18-week testing period. The aim of the study was to determine if adding m-PGA-Cur to the treatment regime enabled the meloxicam to be tapered at the rate of 25% during the first 8 weeks of combined treatment without experiencing worsening of pain. The investigators found that 75% of the dogs were assessed as having no pain increases 10 weeks after the withdrawal of meloxicam. They concluded that the m-PGA-Cur was able to maintain the level of pain relief previously maintained only by the meloxicam.
Read more about PEA on our PEA webpage.
* Palm oil: The palm oil cultivation industry has been destroying rainforests in Sumatra and Borneo in Indonesia and Malaysia, the only habitats of orangutans. If you are going to obtain PEA, we suggest that you do so only from vendors whose PEA has been manufactured with palm oil from sustainable sources and not the deforestation of rainforests. Read more about finidng sources of sustainable palm oil at www.orangutanlandtrust.com. To avoid palm oil as the source of PEA, read the ingredients descriptions on the brands of PEA in which you are interested.
Nutraceuticals are nutrients necessary for supporting or improving normal structure and function of the weight-bearing joints. They have been found to:
• Support or enhance metabolism of cartilage cells (chondrocyte) and joint membranes (synoviocyte) -- an anabolic effect;
• Inhibit damaging enzymes within synovial fluid and cartilage -- a catabolic effect;
• Inhibit formation of thrombi in small blood vessels supplying the joint (antithrombolic).
The most common nutraceuticals are glucosamine and chondroitin. Glucosamine regulates the synthesis of collagen in cartilage, and may provide mild anit-inflammatory effects. Crystalline glucosamine sulphate has the greatest efficacy and bioavailablity for osteoarthritis. Chondroitin sulfate inhibits destructive enzymes in joint fluid and cartilage. Both of them also contribute to the building blocks synthesis of glycoaminoglycans and proteoglycans) for the formation and repair of cartilage.
Undenatured type-II collagen (UC-II), a patented form of collagen extracted from the cartilage of the chicken’s sternum, has been found effective in reducing pain and discomfort experienced by dogs suffering from (osteoarthritis.
Microlactin (Duralactin) is a nutraceutical consisting of a protein concentrate derived from the milk of hyper-immunized cows, called hyper-immune milk factor (HIMF). It reportedly impedes inflammation and can be used safely in dogs. It is slow to respond to pain, taking a week to two weeks for maximum effectiveness.
 Cannabinol (CBD) is
is a cannabinoid compound produced from hemp and marijuana (Cannabis
Sativa) plants. CBD oil mimics the endocannabinoid molecules which the
dog’s (and our) body produces in several different organs. They play
roles in reducing pain, regulating inflammation, and affecting the
immune system, by initially binding to receptors in the brain.
Cannabinol (CBD) is
is a cannabinoid compound produced from hemp and marijuana (Cannabis
Sativa) plants. CBD oil mimics the endocannabinoid molecules which the
dog’s (and our) body produces in several different organs. They play
roles in reducing pain, regulating inflammation, and affecting the
immune system, by initially binding to receptors in the brain.
CBD is non-psychoactive, unlike tetrahydrocannabinol (THC), another cannabinoid compound from marijuana, which is considered psychoactive by altering the mental state, and can be highly toxic to dogs.
Varieties of CBD: Cannabidiol-based veterinary products are derived mainly from hemp (Cannabis sativa) and must contain less than 0.3% tetrahydrocannabinol (THC). This form of CBD can be processed into “full spectrum” or “broad spectrum” and also may be in the form of a “distillate”, in which all THC has been removed, or in the form of CBD “isolate”, which is a purifed powder.
• Full Spectrum: Full spectrum CBD contains other extracts found in the cannabis plant, including terpenes, and up to 0.3% THC.
• Broad Spectrum: Broad spectrum CBD also contains some other cannabis compounds but no more than trace amounts of THC.
• CBD Isolate: CBD isolate is pure CBD and contains no other cannabis plant compounds.
• Naked CBD: Naked CBD describes CBD oil by itself, as opposed to being capsultated or microcapsulated or combined with any other substance, such as deoxycholic acid (DCA).
• Liposomal CBD: This is an orally administered encapsultated CBD which is packaged within liposomes, small fatty cellular sacs which improve bioavailability of the CBD by enabling it to be withstand digesstion in the stomach and degradation in the liver. Lipsomal CBD was tested on dogs in this September 2020 article.
• Cannabidiolic acid (CBDA) is an acid precursor of CBD. It forms CBD when heated. It has been shown in some studies to be more potent that CBD for treating rats. It has been found to be more readily absorbed into the human bloodstream than CBD. Aa theory is that adding CBDA to doses of CBD may make the CBD more absorbable. In this September 2020 article, the investigators found that CBDA is absorbed at least twice as well as CBD in dogs within a 24 hour period, with some differences depending upon the medium used to deliver the oral treatment.
 The most canine studies of CBD thus far have been regarding
osteoarthritis (OA). The results have been fairly favorable, with the
clear exception of one study, the one reported in the
March 2021 article. Each of them is summarized below.
The most canine studies of CBD thus far have been regarding
osteoarthritis (OA). The results have been fairly favorable, with the
clear exception of one study, the one reported in the
March 2021 article. Each of them is summarized below.
Interestingly, only one of the studies thus far has included any cavalier King Charles spaniels. And in the March 2020 article below, the two CKCSs were singled out as requiring the highest dose of CBD to achieve any measurable relief.
In a July 2018 article, researchers report on a study of 16 dogs to determine the safety of CBD extract and its efficacy in allevieating pain in dogs diagnosed with osteoarthritis (OA). The equal mix of CBD and carboxylic acid of CBD (CBDA), was administered at 2mg/kg every 12 hours for 4 weeks. The treated dogs were:
"... perceived to be more comfortable and active. There appear to be no observed side effects of the treatment ... dogs undergoing OA treatment for a month duration. There were some dogs with incidental rises in alkaline phosphatase that could be related to the treatment. Further long-term studies with larger populations are needed to identify long-term effects of CBD rich industrial hemp treatment, however short term effects appear to be positive."
In a March 2020 article about a pilot study of 32 osteoarthritic dogs, in which two cavalier King Charles spaniels were included, hemp-derived CBD oil administered to the dogs reportedly "appears to positively affect dogs with chronic maladaptive pain by decreasing their pain, thereby improving their mobility and quality of life." The specific ingredients of the CBD oil and its dosages were:
"At the initial evaluation and enrollment, qualified dogs received a CBD oil product at a dose of 0.25 mg/kg delivered on food QD for 3 days and then morning and night (approximately every 12 hours). The product given was a certified organic, cold-pressed hemp seed oil infused with 1,000 mg of full-spectrum hemp extract derived from organically grown hemp plants, cultivated in Colorado. Full-spectrum extract includes cannabinoids (such as cannabidiolic acid, CBD, cannabigerol, cannabichromene), flavonoids, terpenes, and other constituents within the cannabis plant."
Most interestingly, the investigators singled out the two CKCSs:
"Among these 30 dogs, the dose of CBD needed to achieve a positive effect ranged from 0.3 up to 4.12 mg/kg BID. The 2 dogs in the study requiring the highest dose of the CBD product were both Cavalier King Charles spaniels (not related to one another), and neither of these dogs experienced any changes/elevations in liver enzymes."
In an August 2020 article, 9 dogs being treated for chronic osteoarthritis-related pain with conventional medications were dosed with oral transmucosal (OTM) cannabidiol (CBD) (2 mg/kg) every 12 hours for 12 weeks. The investigators report that the Pain Severity Score and the Pain Interference Score were significantly lower in CBD than in the control group of 12 other dogs, and the Quality of Life Index was significantly higher in the CBD group. They concluded:
"The addition of OTM CBD showed promising results. Further pharmacokinetics and long-term studies in larger populations are needed to encourage its inclusion into a multimodal pharmacological approach for canine osteoarthritis-related pain."
In a September 2020 article, 15 dogs diagnosed with osteoarthritis were divided into 3 groups and administered (a) 20 mg/day (0.5 mg/kg) naked CBD, (b) 50 mg/day (1.2 mg/kg) naked CBD, or (c) 20 mg/day liposomal CBD for 30 days. The dogs were tested on the first and last days for four different movements: sitting to standing, lying to standing, walking, and running. The investigators report that, among the 5 dogs receiving 20 mg/day of naked CBD, there generally were no improvements noted among all four movement categories. As for the 5 dogs being dosed 50 mg/day, there were "significant improvements" among all four assessment categories, as also were the 5 dogs receiving 20 mg/day liposomal CBD.
In a March 2021 article, 23 dogs with naturally occurring osteoarthritis of appendicular joints received 2.5 mg/kg of a CBD isolate in hempseed oil for six weeks. The investigators measured outcome objective gait analysis, activity counts (via accelerometry) and clinical metrology instruments. They report finding no differences noted between the CBD group and the placebo group at any time point for any of the recorded outcome measures. As adverse events, then noted elevation in liver enzymes in a majority of the dogs, and vomiting in two. They concluded that, "The pilot data from this study do not support the use of CBD as a symptom-relieving agent for canine OA."
See our Cannabis webpage for additional details about CBD, including delivery methods, bioavailability, dosages, and adverse reactions.
Laser therapy, called "photobiomodulation" (PBM), which is continuous wave laser treatments at acupuncture sites, is a treatment option, either with or without medication.
RETURN TO TOP
What You Can Do
Owners may provide their affected dogs with supplements such as
glucoamine HCI,
 methylsulfonylmethane (MSM), N,N-Dimethylglycine HCI
(DMG), and manganese. Retail combinations of these supplements include
Vetri-Science GlycoFlex Joint Support.
methylsulfonylmethane (MSM), N,N-Dimethylglycine HCI
(DMG), and manganese. Retail combinations of these supplements include
Vetri-Science GlycoFlex Joint Support.
An aid to cavaliers suffering from arthritis is an elevated dog food bowl. The Ergo Feeder (at right) is an example.
RETURN TO TOP
Research News
January 2024:
Cavaliers ranked fourth among 84 cases of immune-mediated
polyarthritis cases in one UK hospital study.
 In
a
January 2024 article, UK researchers (Judith Cruzado Perez
[right], Victoria Travail, Valerie Lamb, Darren Kelly) reviewed 84
cases of canine immune-mediated polyarthritis at one UK animal hospital
during the years 2011-2021. Dogs with neutrophilic inflammation in 2 or
more joints were included. Three of the dogs (3.5%) were cavalier King
Charles spaniels. The object of the study was to describe the patients,
their symptoms, physical condtions, treatments, and outcomes. They
concluded that "IMPA carries a fair prognosis, but relapses occur in
many cases and euthanasia due to relapsing or refractory disease is not
uncommon."
In
a
January 2024 article, UK researchers (Judith Cruzado Perez
[right], Victoria Travail, Valerie Lamb, Darren Kelly) reviewed 84
cases of canine immune-mediated polyarthritis at one UK animal hospital
during the years 2011-2021. Dogs with neutrophilic inflammation in 2 or
more joints were included. Three of the dogs (3.5%) were cavalier King
Charles spaniels. The object of the study was to describe the patients,
their symptoms, physical condtions, treatments, and outcomes. They
concluded that "IMPA carries a fair prognosis, but relapses occur in
many cases and euthanasia due to relapsing or refractory disease is not
uncommon."
May 2022:
Cavaliers were the second most prevalent breed in a UK study of
dogs with immune-mediated polyarthritis (IMPA).
 In
a
May 2022 article, UK veterinary researchers Lucy A. Barker
(right), S. McManus, S. Adamantos, and V. Black examined the
medical records of 58 dogs diagnosed with idiopathic non-erosive
immune-mediated polyarthritis (IMPA) to determine the clinical role
which proteinuria may play in IMPA and to determine if proteinuria
resolves on the treatment of the underlying IMPA. The most common
affected breed was the cocker spaniel at 8.6%, followed by the cavalier
King Charles spaniel at 7%. They found that proteinuria was a common
abnormality in IMPA-affected dogs being studied and appears to
frequently resolve on the treatment of the underlying disease.
In
a
May 2022 article, UK veterinary researchers Lucy A. Barker
(right), S. McManus, S. Adamantos, and V. Black examined the
medical records of 58 dogs diagnosed with idiopathic non-erosive
immune-mediated polyarthritis (IMPA) to determine the clinical role
which proteinuria may play in IMPA and to determine if proteinuria
resolves on the treatment of the underlying IMPA. The most common
affected breed was the cocker spaniel at 8.6%, followed by the cavalier
King Charles spaniel at 7%. They found that proteinuria was a common
abnormality in IMPA-affected dogs being studied and appears to
frequently resolve on the treatment of the underlying disease.
November 2016:
Cavaliers were 15+% of dogs with erosive immune-mediated
polyarthritis (IMPA).
 In
a
November 2016 article, a team of Wisconsin and Michigan researchers
(Magen L. Shaughnessy, Susannah J. Sample, Carter Abicht, Caitlin
Heaton, Peter Muir) studied the clinical records of 79 dogs
diagnosed with immune-mediated polyarthritis (IMPA). Of those 79 dogs,
13 had erosive IMPA, of which, two were cavalier King Charles spaniels.
The 13 affected dogs had erosive lesions in their carpal joints. The
estimated median synovial fluid lymphocyte count for dogs with erosive
IMPA was significantly greater than that for dogs with nonerosive IMPA.
Results indicated erosive IMPA most commonly affected the carpal joints
of middle-aged small-breed dogs. (See left carpus of an 8-year-old
spayed female Cavalier King Charles Spaniel with subjectively moderate
subchondral bone lysis accompanied by severe synovial swelling -- in
x-ray at right.)
In
a
November 2016 article, a team of Wisconsin and Michigan researchers
(Magen L. Shaughnessy, Susannah J. Sample, Carter Abicht, Caitlin
Heaton, Peter Muir) studied the clinical records of 79 dogs
diagnosed with immune-mediated polyarthritis (IMPA). Of those 79 dogs,
13 had erosive IMPA, of which, two were cavalier King Charles spaniels.
The 13 affected dogs had erosive lesions in their carpal joints. The
estimated median synovial fluid lymphocyte count for dogs with erosive
IMPA was significantly greater than that for dogs with nonerosive IMPA.
Results indicated erosive IMPA most commonly affected the carpal joints
of middle-aged small-breed dogs. (See left carpus of an 8-year-old
spayed female Cavalier King Charles Spaniel with subjectively moderate
subchondral bone lysis accompanied by severe synovial swelling -- in
x-ray at right.)
RETURN TO TOP
RETURN TO TOP
Veterinary Resources
Idiopathic, non-infectious, non-erosive arthritis in a bitch. C.R. Hutchings, G.A. Verkerk, K.J. Kissling. New Zealand Vet. J. 1980;28(5). Quote: A 2 1/2-year-old Cavalier King Charles Spaniel bitch was examined because of recurring episodes of lameness and joint swelling over a period of 2 years. Clinical examination, radiography, serology, joint-fluid analysis and histopathology of the joint capsule led to a diagnosis of idiopathic, non-infectious, non-erosive arthritis. Combination therapy with prednisolone, cyclophosphamide and azothioprine produced a rapid improvement in the dog's condition. The features of this disease and its relationship to rheumatoid arthritis and systemic lupus erythematosis are discussed.
Immune-based non-erosive inflammatory joint disease of the dog. 3. Canine idiopathic polyarthritis. David Bennett. J. Sm. Anim. Pract. October 1987; doi: 10.1111/j.1748-5827.1987.tb01316.x. Quote: The features of 67 cases of canine idiopathic polyarthritis are described. Idiopathic polyarthritis includes cases of non-infective polysynovitis which cannot be classified into more defined groups. It most often affects young adult dogs, and pyrexia, inappetence and lethargy are exhibited as well as lameness. Radiography usually shows soft tissue changes. Four types are identified according to certain associations; [34 dogs with] Type I (uncomplicated), [19 dogs with] Type II (infection elsewhere in the body), [8 dogs with] Type III (gastro-intestinal disease) [including one cavalier King Charles spaniel (12.5%)] and [6 dogs with] Type IV (neoplastic disease elsewhere in the body). ... Type III (enteropathic arthritis): polyarthritis associated with gastro-intestinal disease; eg, gastro-enteritis, ulcerative colitis. ... In Type III cases the gastro-intestinal disease was treated usually with antibiotics and kaolin preparations. ... Prednisolone was the drug of choice in the Type I cases and was also used in Types II and III to help resolve the joint inflammation. ... If the animal relapsed at a later date, the dosage regime was repeated. In some cases, especially where relapses were common [including the CKCS], cytotoxic drugs were used; ie, cyclophosphamide or azathioprine.
Alphal-Proteinase Inhibitor Deficiency and Bartonella Infection in Association with Panniculitis, Polyarthritis, and Meningitis in a Dog. P.J. Mellor, K. Fetz, R.G. Maggi, S. Haugland, M. Dunning, E.J. Villiers, R.J. Mellanby, D. Williams, E. Breitschwerdt, M.E. Herrtage. J. Vet. Intern. Med. July 2006; doi: 10.1111/j.1939-1676.2006.tb01823.x. Quote: A 7-year-old male neutered Cavalier King Charles Spaniel dog presented to the referring veterinarian with a 1-day history of right forelimb lameness and was symptomatically treated with carprofen. ... Fourteen weeks (day 98) after the onset of clinical signs, the dog was referred to the Queen’s Veterinary School Hospital, University of Cambridge for the investigation of ongoing lethargy and shifting lameness. ... Panniculitis is an uncommon inflammatory disease of subcutaneous fat characterized by painful, subcutaneous nodules that may ulcerate and form sinus tracts discharging oily material. The dermatologic presentation also may be accompanied by systemic signs. It is an infrequently documented condition in the dog and in many cases the etiopathogenesis remains unknown, or it is putatively described as an immune-mediated disorder. ... A primary presenting sign in the patient was severe shifting lameness with nonlocalized pain. There was neither clinical nor histopathologic evidence of subcutaneous tissue inflammation in the limbs. A complete skeletal radiographic survey failed to identify any lesions. Concurrent bone marrow fat necrosis has been reported in association with canine panniculitis, and bone pain has been noted as a clinical manifestation. Marrow core biopsy did not provide evidence of fat necrosis in the patient. The dog lacked clear clinical and radiographic evidence of joint inflammation, but arthrocentesis supported a diagnosis of neutrophilic polyarthritis. The clinical signs of neck pain and the CSF analysis were consistent with meningitis. ... Bone marrow examination revealed adequate neutrophil production. The degree of neutrophil infiltration within joint fluid and CSF was cytologically assessed as mild to moderate (ie, not suggestive of massive sequestration of blood neutrophils into these areas). The cause of this patient’s neutropenia was not conclusivedly identified, but seems likely to be because of underlying Bartonella infection or immune-mediated neutropenia. ... We suspect that Bartonella acted in concert with A1PI deficiency [alpha1-proteinase inhibitor deficiency], facilitating the clinical manifestation of panniculitis in the patient. To the authors’ knowledge, this is the 1st reported case for either Bartonella-associated or alpha1-proteinase inhibitor deficiency–associated panniculitis in the dog.
Progressive lameness in a Cavalier King Charles Spaniel. Mark Longley, Kinley Smith. BSAVA Companion. April 2011; doi: 10.22233/20412495.0411.10. Quote: An 8-year-old Cavalier King Charles Spaniel presented with a 6-month history of progressive forelimb lameness. The diagnosis and treatment of rheumatoid arthritis is described.
Micronized/ultramicronized palmitoylethanolamide displays superior oral efficacy compared to nonmicronized palmitoylethanolamide in a rat model of inflammatory pain. Daniela Impellizzeri, Giuseppe Bruschetta, Marika Cordaro, Rosalia Crupi, Rosalba Siracusa, Emanuela Esposito, Salvatore Cuzzocrea. Neuroinflammation. August 2014; doi: 10.1186/s12974-014-0136-0. Quote: Background: The fatty acid amide palmitoylethanolamide (PEA) has been studied extensively for its anti-inflammatory and neuroprotective actions. The lipidic nature and large particle size of PEA in the native state may limit its solubility and bioavailability when given orally, however. Micronized formulations of a drug enhance its rate of dissolution and reduce variability of absorption when orally administered. The present study was thus designed to evaluate the oral anti-inflammatory efficacy of micronized/ultramicronized versus nonmicronized PEA formulations. Methods: Micronized/ultramicronized PEA was produced by the air-jet milling technique, and the various PEA preparations were subjected to physicochemical characterization to determine particle size distribution and purity. Each PEA formulation was then assessed for its anti-inflammatory effects when given orally in the carrageenan-induced rat paw model of inflammation, a well-established paradigm of edema formation and thermal hyperalgesia. Results: Intraplantar injection of carrageenan into the right hind paw led to a marked accumulation of infiltrating inflammatory cells and increased myeloperoxidase activity. Both parameters were significantly decreased by orally given micronized PEA (PEA-m; 10 mg/kg) or ultramicronized PEA (PEA-um; 10 mg/kg), but not nonmicronized PeaPure (10 mg/kg). Further, carrageenan-induced paw edema and thermal hyperalgesia were markedly and significantly reduced by oral treatment with micronized PEA-m and ultramicronized PEA-um at each time point compared to nonmicronized PeaPure. However, when given by the intraperitoneal route, all PEA formulations proved effective. Conclusions: These findings illustrate the superior anti-inflammatory action exerted by orally administered, micronized PEA-m and ultramicronized PEA-um, versus that of nonmicronized PeaPure, in the rat paw carrageenan model of inflammatory pain.
Nerve Growth Factor: A Focus on Neuroscience and Therapy. Luigi Aloe, Maria Luisa Rocco, Bijorn Omar Balzamino, Alessandra Micera. Curr. Neuropharmacol. May 2015; doi: 10.2174/2F1570159X13666150403231920 Quote: Nerve growth factor (NGF) is the firstly discovered and best characterized neurotrophic factor, known to play a critical protective role in the development and survival of sympathetic, sensory and forebrain cholinergic neurons. NGF promotes neuritis outgrowth both in vivo and in vitro and nerve cell recovery after ischemic, surgical or chemical injuries. Recently, the therapeutic property of NGF has been demonstrated on human cutaneous and corneal ulcers, pressure ulcer, glaucoma, maculopathy and retinitis pigmentosa. NGF eye drops administration is well tolerated, with no detectable clinical evidence of systemic or local adverse effects. The aim of this review is to summarize these biological properties and the potential clinical development of NGF.
Clinical features and pathological joint changes in dogs with
erosive immune-mediated polyarthritis: 13 cases (2004–2012).
Magen L. Shaughnessy, Susannah J. Sample, Carter Abicht, Caitlin
Heaton, Peter Muir. JAVMA. November 2016;249(10):1156-1164. Quote:
Objective: To evaluate the clinical features and pathological joint
changes in dogs with erosive immune-mediated polyarthritis (IMPA).
Design: Retrospective case series. Animals: 13 dogs with erosive
IMPA [including two cavalier King Charles spaniels
(15.4%)] and 66 dogs with nonerosive IMPA. Procedures: The medical
record database of a veterinary teaching hospital was reviewed to
identify dogs with IMPA that were examined between October 2004 and
December 2012.
 For
each IMPA-affected dog, information extracted from the medical
record included signalment, diagnostic test results, radiographic
findings, and treatments administered. Dogs were classified as
having erosive IMPA if review of radiographs revealed the presence
of bone lysis in multiple joints, and descriptive data were
generated for those dogs. All available direct smears of synovial
fluid samples underwent cytologic evaluation. The synovial fluid
total nucleated cell count and WBC differential count were estimated
and compared between dogs with erosive IMPA and dogs with nonerosive
IMPA. Results: 13 of 79 (16%) dogs had erosive IMPA. Dogs with
erosive IMPA had a mean ± SD age of 7.1 ± 2.4 years and body weight
of 8.3 ± 3.4 kg (18.3 ± 7.5 lb). All 13 dogs had erosive lesions in
their carpal joints. (See left carpus of an 8-year-old spayed
female Cavalier King Charles Spaniel with subjectively moderate
subchondral bone lysis accompanied by severe synovial swelling -- in
x-ray at right).The estimated median synovial fluid lymphocyte
count for dogs with erosive IMPA was significantly greater than that
for dogs with nonerosive IMPA. All dogs received immunosuppressive
therapy with leflunomide (n = 9), prednisone (3), or
prednisone-azathioprine (1). Conclusions & Clinical Relevance:
Results indicated erosive IMPA most commonly affected the carpal
joints of middle-aged small-breed dogs. Further genetic analyses and
analysis of lymphocyte-subsets are warranted for dogs with erosive
IMPA.
For
each IMPA-affected dog, information extracted from the medical
record included signalment, diagnostic test results, radiographic
findings, and treatments administered. Dogs were classified as
having erosive IMPA if review of radiographs revealed the presence
of bone lysis in multiple joints, and descriptive data were
generated for those dogs. All available direct smears of synovial
fluid samples underwent cytologic evaluation. The synovial fluid
total nucleated cell count and WBC differential count were estimated
and compared between dogs with erosive IMPA and dogs with nonerosive
IMPA. Results: 13 of 79 (16%) dogs had erosive IMPA. Dogs with
erosive IMPA had a mean ± SD age of 7.1 ± 2.4 years and body weight
of 8.3 ± 3.4 kg (18.3 ± 7.5 lb). All 13 dogs had erosive lesions in
their carpal joints. (See left carpus of an 8-year-old spayed
female Cavalier King Charles Spaniel with subjectively moderate
subchondral bone lysis accompanied by severe synovial swelling -- in
x-ray at right).The estimated median synovial fluid lymphocyte
count for dogs with erosive IMPA was significantly greater than that
for dogs with nonerosive IMPA. All dogs received immunosuppressive
therapy with leflunomide (n = 9), prednisone (3), or
prednisone-azathioprine (1). Conclusions & Clinical Relevance:
Results indicated erosive IMPA most commonly affected the carpal
joints of middle-aged small-breed dogs. Further genetic analyses and
analysis of lymphocyte-subsets are warranted for dogs with erosive
IMPA.
Prevalence, duration and risk factors for appendicular osteoarthritis in a UK dog population under primary veterinary care. Katharine L. Anderson, Dan G. O’Neill, David C. Brodbelt, David B. Church, Richard L. Meeson, David Sargan, Jennifer F. Summers, Helen Zulch, Lisa M. Collins. Sci. Repts. April 2018;8:5641. Quote: Osteoarthritis is the most common joint disease diagnosed in veterinary medicine and poses considerable challenges to canine welfare. This study aimed to investigate prevalence, duration and risk factors of appendicular osteoarthritis in dogs under primary veterinary care in the UK. The VetCompassTM programme collects clinical data on dogs attending UK primary-care veterinary practices. The study included all VetCompassTM dogs under veterinary care during 2013. Candidate osteoarthritis cases were identified using multiple search strategies. A random subset was manually evaluated against a case definition. Of 455,557 study dogs, 16,437 candidate osteoarthritis cases were identified; 6104 (37%) were manually checked and 4196 (69% of sample) were confirmed as cases. Additional data on demography, clinical signs, duration and management were extracted for confirmed cases. Estimated annual period prevalence (accounting for subsampling) of appendicular osteoarthritis was 2.5% (CI95: 2.4–2.5%) equating to around 200,000 UK affected dogs annually. Risk factors associated with osteoarthritis diagnosis included breed (e.g. Labrador, Golden Retriever), being insured, being neutered, of higher bodyweight and being older than eight years. Duration calculation trials suggest osteoarthritis affects 11.4% of affected individuals’ lifespan, providing further evidence for substantial impact of osteoarthritis on canine welfare at the individual and population level. ... Prevalence estimate. The estimated annual period prevalence of osteoarthritis diagnosis in dogs under primary veterinary care in the UK during 2013 was 2.5% (CI95: 2.4–2.5%). Prevalence of the most frequently affected breeds was also calculated with the most prevalent breeds being large breeds, specifically: Golden Retriever (7.7% of all Golden retrievers), Labrador Retriever (6.1% of all Labradors), Rottweiler (5.4% of all Rottweilers) and German Shepherd Dog (4.9% of all German Shepherds). ... Cavalier King Charles (2.42%).
Spontaneous Septic Arthritis of Canine Elbows: Twenty-One Cases. Ben Mielke, Eithne Comerford, Kate English, Richard Meeson. Vet Comp Orthop Traumatol. November 2018;31(6):488-493. Quote: Objective: This study provides information on clinical features, diagnosis, treatment and associated risk factors of spontaneous septic elbow arthritis in the dog. Methods: Medical records between March 2007 and June 2015 were searched for cases of spontaneous septic elbow arthritis with a diagnosis based on clinical signs, arthrocentesis, cytological and microbiological analysis of elbow joint synovial fluid, radiography and outcome following treatment. Results: Twenty-one cases of septic arthritis were identified [including one cavalier King Charles spaniel]. Pre-existing osteoarthritis was present in 14/15 elbows for which diagnostic imaging was available. Although all cases had increased neutrophil count on synovial fluid cytology, culture was only positive in 12/21. Despite initial improvement in lameness scores (pre-treatment 9/10 [range: 1-10] versus post-treatment 3/10 [range: 1-5]), 11/12 had residual long-term lameness. Recurrence of infection was noted in 3/12 elbows for which long-term (>8 weeks) follow-up was available. There was an acute mortality rate of 2/21 associated with severe systemic sepsis. Clinical significance: Septic arthritis, even in the absence of pyrexia, should be considered as a major differential diagnosis in middle aged, large breed dogs, with pre-existing elbow arthritis, that suffer an acute onset lameness, with elbow joint effusion and discomfort. Antibiotic therapy alone was effective for treatment with high initial response rates. Chronic lameness post-treatment was common, and a high rate of recurrence was seen with 3/12 dogs suffering more than one episode.
The Use of Cannabidiol-Rich Hemp Oil Extract to Treat Canine Osteoarthritis-Related Pain: A Pilot Study. Lori Kogan, Peter Hellyer, Robin Downing. AHVMA J. March 2020;58(Spring):42-45. Quote: The objective of this 90-day pilot clinical trial was to assess the impact of a full-spectrum product containing hemp extract and hemp seed oil on dogs with chronic mal adaptive pain. A total of 37 dogs diagnosed with chronic maladaptive pain primarily as a result of osteoarthritis were enrolled in the study. The dogs were given an initial physical examination that included systematic pain palpation, mapping of pain patterns, informal gait analysis, metabolic profile, and owner interview. The same palpa tions and mappings were performed during each biweekly assessment to identify trends, chart progress, and inform dose adjustments. ... Among these 30 dogs, the dose of CBD needed to achieve a positive effect ranged from 0.3 up to 4.12 mg/kg BID. The 2 dogs in the study requiring the highest dose of the CBD product were both Cavalier King Charles spaniels (not related to one another), and neither of these dogs experienced any changes/elevations in liver enzymes. It is unclear why some patients responded to a very small dose of the CBD product (0.3 mg/kg per dose), whereas the majority required dosing in the range of 1 to 2 mg/kg per dose. ... The metabolic parameters were repeated at the end of the study. Of the 32 dogs that completed the study, 30 dogs demonstrated improved pain support. Of the 23 dogs in the study that were taking gabapentin at the time of enrollment, 10 dogs were able to discontinue the gabapentin, and an additional 11 dogs were able to have their daily dose reduced with the addition of the cannabidiol (CBD) oil. Conclusion: The addition of a hemp- derived CBD oil appears to positively affect dogs with chronic maladaptive pain by decreasing their pain, thereby improving their mobility and quality of life. The reduction in gabapentin dose may be the result of changes in analgesia and/or sedation with the addition of the hemp oil extract.
Oral Transmucosal Cannabidiol Oil Formulation as Part of a Multimodal Analgesic Regimen: Effects on Pain Relief and Quality of Life Improvement in Dogs Affected by Spontaneous Osteoarthritis. Federica Alessandra Brioschi, Federica Di Cesare, Daniela Gioeni, Vanessa Rabbogliatti, Francesco Ferrari, Elisa Silvia D’Urso, Martina Amari, Giuliano Ravasio. Animals. August 2020; doi: 10.3390/ani10091505. Quote: The aim of this study was to evaluate the efficacy of oral transmucosal (OTM) cannabidiol (CBD), in addition to a multimodal pharmacological treatment for chronic osteoarthritis-related pain in dogs. Twenty-one dogs were randomly divided into two groups: in group CBD (n = 9), OTM CBD (2 mg kg−1 every 12 h) was included in the therapeutic protocol (anti-inflammatory drug, gabapentin, amitriptyline), while in group C (n = 12), CBD was not administered. Dogs were evaluated by owners based on the Canine Brief Pain Inventory scoring system before treatment initiation (T0), and one (T1), two (T2), four (T3) and twelve (T4) weeks thereafter. Pain Severity Score was significantly lower in CBD than in C group at T1 (p = 0.0002), T2 (p = 0.0043) and T3 (p = 0.016). Pain Interference Score was significantly lower in CBD than in C group at T1 (p = 0.0002), T2 (p = 0.0007) and T4 (p = 0.004). Quality of Life Index was significantly higher in CBD group at T1 (p = 0.003). The addition of OTM CBD showed promising results. Further pharmacokinetics and long-term studies in larger populations are needed to encourage its inclusion into a multimodal pharmacological approach for canine osteoarthritis-related pain.
A randomized, double-blind, placebo-controlled study of daily cannabidiol for the treatment of canine osteoarthritis pain. Chris D. Verrico, Shonda Wesson, Vanaja Konduri, Colby J. Hofferek, Jonathan Vazquez-Perez, Emek Blair, Kenneth Dunner Jr, Pedram Salimpour, William K. Decker, Matthew M. Halpert. Pain. September 2020; doi: 10.1097/j.pain.0000000000001896. Quote: Over the last 2 decades, affirmative diagnoses of osteoarthritis (OA) in the United States have tripled due to increasing rates of obesity and an aging population. Hemp-derived cannabidiol (CBD) is the major nontetrahydrocannabinol component of cannabis and has been promoted as a potential treatment for a wide variety of disparate inflammatory conditions. Here, we evaluated CBD for its ability to modulate the production of proinflammatory cytokines in vitro and in murine models of induced inflammation and further validated the ability of a liposomal formulation to increase bioavailability in mice and in humans. Subsequently, the therapeutic potential of both naked and liposomally encapsulated CBD was explored in a 4-week, randomized placebo-controlled, double-blinded study in a spontaneous canine model of OA. In vitro and in mouse models, CBD significantly attenuated the production of proinflammatory cytokines IL-6 and TNF-α while elevating levels of anti-inflammatory IL-10. In the veterinary study, CBD significantly decreased pain and increased mobility in a dose-dependent fashion among animals with an affirmative diagnosis of OA. Liposomal CBD (20 mg/day) was as effective as the highest dose of nonliposomal CBD (50 mg/day) in improving clinical outcomes. Hematocrit, comprehensive metabolic profile, and clinical chemistry indicated no significant detrimental impact of CBD administration over the 4-week analysis period. This study supports the safety and therapeutic potential of hemp-derived CBD for relieving arthritic pain and suggests follow-up investigations in humans are warranted.
Point prevalence and clinical course of proteinuria in dogs with idiopathic non-erosive immune-mediated polyarthritis. L. Barker, S. McManus, S. Adamantos, V. Black. J. Sm. Anim. Pract. May 2022; doi: 10.1111/jsap.13503. Quote: Objectives: To describe the point prevalence and clinical course of proteinuria in dogs diagnosed with idiopathic non-erosive immune-mediated polyarthritis. Materials and Methods: Cases presenting to a single referral centre with a diagnosis of idiopathic non-erosive immune-mediated polyarthritis were retrospectively recruited from January 2009 to August 2018. Data including signalment, urinalysis, clinicopathological results, cytology from arthrocentesis, treatment and long-term follow-up were analysed. Dogs were defined as: non-proteinuric (UPC <0.2), borderline proteinuric (UPC 0.2-0.5) or overtly proteinuric (UPC >0.5). Results: Fifty-eight dogs met the inclusion criteria. ... Presenting breeds included cocker spaniel (n=5), Cavalier King Charles spaniel (n=4) [7%], Labrador retriever (n=4), whippet (n=4), springer spaniel (n=3), Chinese crested (n=2), corgi (n=2), Jack Russell terrier (n=2), English pointer (n=2), and 13 dogs of mixed breeds and one each of 18 other breeds. ... Twenty-two dogs were overtly proteinuric (38%), eight dogs were borderline proteinuric (14%) and 28 dogs were non-proteinuric (48%). Repeated urinalysis was performed in nine of 12 dogs with UPC greater than 2.0. The UPC decreased in all nine dogs, with the UPC decreasing to less than 0.5 in 44% of dogs. A greater than 50% decrease in UPC was noted in 44% of dogs, despite seven of nine (77%) receiving prednisolone as either monotherapy or in conjunction with an adjunctive immunosuppressive medication. Clinical Significance: Proteinuria was common in this cohort of dogs diagnosed with primary idiopathic non-erosive immune-mediated polyarthritis. The use of prednisolone does not appear to be contraindicated in proteinuric dogs with idiopathic non-erosive immune-mediated polyarthritis.
Efficacy and safety of cannabidiol for the treatment of canine osteoarthritis: a systematic review and meta-analysis of animal intervention studies. Chanthawat Patikorn, Osot Nerapusee, Kumpanart Soontornvipart, Kanta Lawonyawut, Kachapong Musikpodok, Kanisorn Waleethanaphan, Puree Anantachoti. Front. Vet. Sci. September 2023; doi: 10.3389/fvets.2023.1248417. Quote: Introduction: Canine osteoarthritis (OA) is a degenerative disease with chronic inflammation of internal and external joint structures in dogs. Cannabis spp. contains cannabidiol (CBD), a substance known for various potential indications, such as pain relief and anti-inflammatory in various types of animals, including dogs with OA. As CBD is increasingly in the spotlight for medical use, we aimed to perform a systematic review and meta-analysis to evaluate the efficacy and safety of CBD in treating canine OA. Methods: We searched PubMed, Embase, Scopus, and CAB Direct for animal intervention studies investigating the effects of CBD for canine OA from database inception until February 28, 2023. Study characteristics and findings were summarized. A risk of bias in the included studies was assessed. Meta-analyses were performed using a random-effects model to estimate the effects of CBD on pain scores (0–10), expressed as mean difference (MD) and 95% confidence interval (95% CI). Certainty of evidence was assessed using GRADE. Results: Five articles were included, which investigated the effects of CBD in 117 dogs with OA. All studies were rated as having a high risk of bias. CBD products varied substantially, i.e., oral full-spectrum CBD oil in four studies, and isolated CBD oil and liposomal CBD oil in another study. Treatment duration varied from 4–12 weeks. Meta-analyses of three studies found that, in dogs with OA, treatment with oral full-spectrum CBD oil may reduce pain severity scores (MD; −0.60, 95% CI; −1.51 to 0.31, I2 = 45.64%, p = 0.19) and pain interference scores (MD; −1.52, 95% CI; −3.84 to 0.80, I2 = 89.59%, p = 0.20) but the certainty of evidence was very low. CBD is generally considered safe and well-tolerated in the short-run, with few mild adverse events observed, such as vomiting and asymptomatic increase in alkaline phosphatase level. Conclusion: CBD is considered safe for treating canine OA. CBD may reduce pain scores, but the evidence is very uncertain to conclude its clinical efficacy. High-quality clinical trials are needed to further evaluate the roles of CBD in canine OA.
Librela (Beransa) – Wonder Drug Or Disaster In The Making? Edward Bassingthwaighte. Dogs Naturally. October 2023. Quote: In my professional opinion, there is no way that Librela should ever be considered as a first treatment or intervention for arthritis in dogs.
Canine immune-mediated polyarthritis: A review of 84 cases in the UK between 2011 and 2021. Judith Cruzado Perez, Victoria Travail, Valerie Lamb, Darren Kelly. Vet. Med. & Sci. January 2024; doi: 10.1002/vms3.1306. Background: Immune-mediated polyarthritis (IMPA) is a well-recognised disease in dogs, but studies evaluating the response rates, relapse rates and long-term outcomes are scarce. Objectives: To provide an updated description of the signalment, clinical signs, clinico- pathological findings, distribution between subgroups, rates of response and relapse and long-term outcome of 84 dogs diagnosed with IMPA at a single referral hospital. Methods: Dogs diagnosed with IMPA between January 2011 and December 2021 were identified. Dogs with neutrophilic inflammation in ≥2 joints were included. Cases with <1 month of follow-up, or those missing pertinent data, were excluded. Results: A total of 84 cases were included. ... Cocker spaniels (9/84), Labrador retrievers (6/84), Border col- lies (6/84), Springer spaniels (5/84), Cavalier King Charles spaniels (3/84), Boxers (3/84), German shepherds (2/84), West Highland White terriers (2/84) and Golden retrievers (2/84) were included. The remain- ing cases (32/84) were represented by one individual of different pure breeds. ... An initial response was achieved in 77/84 (92%) cases. Of the cases that initially responded, 37/77 (48%) suffered at least one relapse and 18/77 (23%) suffered multiple relapses. Indefinite treatment was recom- mended in 17/84 (20%) cases. Of the 70 dogs for which at least 12 months of follow-up data were available, 12/70 (17%) were euthanised due to IMPA or for unknown reasons. Conclusion: IMPA carries a fair prognosis, but relapses occur in many cases and euthanasia due to relapsing or refractory disease is not uncommon.
A blinded, randomized and controlled multicenter field study investigating the safety and efficacy of long-term use of enflicoxib in the treatment of naturally occurring osteoarthritis in client-owned dogs. Josep Homedes, Marion Ocak, Sebastian Riedle, Marta Salichs. Frontiers in Vet. Sci. February 2024; doi: 10.3389/fvets.2024.1349901. Quote: Background Enflicoxib is a COX-2 selective NSAID shown to be efficacious and safe in the treatment of pain and inflammation associated with canine osteoarthritis (OA) in clinical studies of 6 weeks duration. Objective This prospective, multisite, blinded, randomized, placebo-controlled, parallel-group field study aimed to confirm the safety and efficacy of enflicoxib in long-term canine OA treatments. Animals A total of 109 client owned dogs with clinical and radiographic signs of OA for at least 3 weeks were enrolled with 78 dogs completing all study visits. Methods Dogs were randomized at a 3:1 ratio to receive enflicoxib (n = 83) or placebo (n = 26) once weekly during 6 months. Dogs underwent veterinary assessments from Day 0 to Day 189 using a clinical sum score (CSS). Efficacy was also assessed by the owners using the Canine Brief Pain Inventory (CBPI). Safety was assessed clinically and by repeated blood and urine sample analysis. The efficacy outcome measure was the treatment response according to the CSS and secondarily the treatment response according to the CBPI. The primary safety outcome was the incidence of adverse events (AEs) and secondarily the evolution of the clinical pathology parameters. Results Percentages of CSS responders for enflicoxib were 71.6; 74.6 and 71.6% on Days 44, 135 and 189 respectively, always showing statistically significant differences (p < 0.05) vs. placebo (41.7, 33.3, and 20.8% respectively). Treatment response according to owner assessments followed the same pattern, achieving significant differences compared to placebo after 2 weeks of treatment. The incidence and type of AEs were as described in previous enflicoxib studies of shorter duration and as for other NSAIDs, with no tendency to increase over time. No relevant changes in hematology, biochemistry or urine parameters were observed. Conclusions and clinical relevance Enflicoxib safety and efficacy profile is maintained after a long-term treatment, which together with its weekly administration, makes it a good alternative for the chronic treatment of dogs with naturally occurring OA.
Cannabidiol plus krill oil supplementation improves chronic stifle osteoarthritis in dogs: A double-blind randomized controlled trial. K. Soontornvipart, P. Wongsirichatchai, A. Pongphuwanun, K. Chatdarong, S. Vimolmangkang. Vet. J. August 2024; doi: 10.1016/j.tvjl.2024.106227. Quote: Osteoarthritis (OA) is the most common orthopedic disorder characterized by chronic inflammation and pain in dogs and cats. Cannabis spp. contains cannabidiol (CBD), a substance with pain relief and anti-inflammatory properties in different animals including dogs with OA. The use of CBD supplements has been increasingly intertwining in veterinary medicine. This study aimed to evaluate the clinical efficacy of CBD + krill oil-supplemented biscuit against canine OA. In total, 30 dogs with stifle OA were randomized and divided into the placebo, krill oil, and CBD + krill oil groups. The Canine Brief Pain Inventory questionnaire was used to evaluate the efficacy of each treatment against pain. Stifle temperature was monitored to identify degrees of stifle inflammation. Two and one dogs in the placebo group were excluded from the study due to worsening lameness and increased pain interference score (PIS) and pain severity score (PSS) at days 14 and 28, respectively. The PIS and PSS scores of the krill oil and CBD + krill oil groups gradually and significantly improved after two weeks of treatment. The CBD + krill oil group had better PIS and PSS scores than the placebo and krill oil groups. However, there was no statistically significant difference in the PIS and PSS scores between the krill oil and CBD + krill oil groups. The stifle temperature of the three groups at different periods did not significantly differ. In conclusion, CBD + krill oil supplements are safe against canine OA. CBD can reduce pain and inflammation. Highlights: • CBD + krill oil-supplemented biscuit significantly reduced pain and inflammation in OA dogs. • Krill oil or CBD + krill oil biscuits both reduced pain, with the latter showing slightly better results. • No side effects were observed when giving the dog the CBD + krill oil-supplemented biscuit.


CONNECT WITH US