Epilepsy and Other Seizures in
Cavalier King Charles Spaniels
-
 Seizures,
In General
Seizures,
In General - What Epilepsy Is
- Symptoms
- Other Seizure Disorders
- Diagnosis
- Treatment
- Breeders' Responsibilities
- What You Can Do
- Research News
- Related Links
- Veterinary Resources
The topic of epilepsy discussed here also includes several different types of seizures and not just the classic idiopathic epilepsy (IE) which is prevalent in cavalier King Charles spaniels.
Seizures, In General
A seizure is a sudden, uncontrolled electrical disturbance in the dog’s brain, that causes behavioral changes. They are classified in two main types, generalized and focal, based upon their signs and and the brain areas affected.
Seizures can be caused by a variety of factors, which also are classified either as primary or secondary to some other underlying cause. Primary seizures include idiopathic epilepsy, meaning that the seizure has no known underlying cause and may be hereditary. Secondary seizures are caused by some identifiable underlying health condition, which may include (1) metabolic disorders (low blood sugar, imbalance in the body chemistry); (2) neurological disorders (brain abnormalities); (3) electrolyte imbalances (abnormal electrolyte levels affecting neuronal functions); (4) trauma to the head; (5) infections in the brain (meningitis, encephalitis); (6) exposure to toxins (chemicals, plants, medications).
Flea and tick treatments which contain isoxazolines can increase the likelihood that dogs susceptible to seizures will experience them. Isoxazolines lower the threshold of seizures. These flea and tick products include Bravecto, Credelio, Nexgard, Revolution Plus, and Simparica Trio.
What Epilepsy Is
Epilepsy is a disease of the dog's brain, which results in repeated physical attacks, called seizures. In dogs, a seizure is caused by an undesired signal sent from the brain through the nervous system to the muscles, resulting in uncontrolled shaking, twitching, often unconsiousness, and occasionally loss of senses and unintentional behaviors. While the brain sends the signal, that does not mean that the brain is the underlying cause of the seizure.
A form of epilepsy, called "idiopathic epilepsy" (IE), is inheritable. While the common definition of "idiopathic" means that the cause is unknown, in veterinary medicine it means that it is a recognized syndrome where there appears to be no structural abnormality. Idiopathic epilsepsy means that it is a disorder that is independent of other disorders or causes (sui generis). IE is believed to be caused by a mutation in a specific gene which the dogs have inherited from their parents. IE is the most common chronic neurological disorder in dogs and is prevalent in cavalier King Charles spaniels.*
* See Neurological diseases of the Cavalier King Charles spaniel.
Because by definition, idiopathic epilepsy's cause is unknown, reseachers have examined IE in dogs with other disorders, called comorbidities or concurrent conditions, such as urinary tract infections. To complicate this issue further, some anti-seizure medications (ASM), such as phenobartital, may have side effects that mimic or cause such concurrent conditions.
According to a June 2004 report, idiopathic epilepsy has been found to occur more frequently in descendants from bloodlines originating from whole-colored CKCS ancestors from the late 1960s, especially from matings of blood relatives, such as half-siblings. See also a follow up report in July 2005.
In a 2012 report, UK neurology researchers examined the magnetic resonance images (MRIs) of 85 cavaliers, looking for a relationship between Chiari-like malformation (CM), ventriculomegaly, and seizures in the dogs. The 85 CKCSs all had CM; 27 of them also had had seizures. They found no association between CM, ventriculomegaly, and the seizures. The seizures were classified as having partial onset -- meaning that they occur in in one area of the brain, unlike generalized seizures which typically affect nerve cells throughout the brain -- in 61% of the dogs. They also stated that "Another cause of recurrent seizures in CKCS (such as familial epilepsy) is suspected, as previously reported."
RETURN TO TOP
Symptoms
There are many different types of seizures in dogs. Common signs include:
• Collapsing or falling – with or without loss of consciousness
• Uncontrolled movements – jerking or twitching movements of the head, legs, or entire body
• Stiffness – a rigid posture of the legs and/or entire body, usually lying on a side, with an arched back
• Paddling or running motions – while lying on a side
• Vocalizations – barking, whining, or howling
• Loss of bladder or bowel control — Involuntary • urination or defecation
The most common is the generalized major motor seizure, characterized by paddling of the limbs. (See photo at upper right.) The dog may cry, bark or whine during the seizure, and it may snap or bite, not quite fully aware of its surroundings. Urination and defecation are common during a generalized seizure.
A brief seizure, called the absence seizure, may last for only seconds, during which the dog may just seem to be staring into space. Other seizures may be localized to only certain parts of the dog's body, called focal seizures, such as head nodding or twitching of the face. Such seizures which continue for over 5 minutes are called Status Epilepticus (SE). Another version of SE is if more than one seizure event occurs within 5 minutes. Some SE seizures may last for over a half hour.
The most severe of seizures, once called a grand mal seizure, is a generalized tonic-clonic seizure, (GTCS) which has two phases of muscle activity, a "tonic" phase (stiffening) and a "clonic" phase (twitching or jerking). Such seizures may progress to SE. See this June 2022 article about a cavalier with GTCS.
![]() See this
YouTube video of a Tibetan spaniel experiencing a seizure. The onset of epilepsy in cavaliers is most common between the ages of six
months and five years.
See this
YouTube video of a Tibetan spaniel experiencing a seizure. The onset of epilepsy in cavaliers is most common between the ages of six
months and five years.
Post seizural signs may last from a few minutes to an hour. It usually takes about 30 minutes for a dog to appear to have fully recovered from epileptic convulstions of a seizure. Any seizure lasting more than five minutes would be an emergency case requiring immediate veterinary care. If the dog remains unconscious following convulsions, that sign also calls from immediate care.
The most common form of hereditary epilepsy in cavaliers is flycatcher's syndrome which is discussed on its own webpage.
RETURN TO TOP
Other Seizure Disorders
- Canine Cognitive Dysfunction
- Encephalitis
- Environmental Causes
- Flycatcher's Syndrome
- Myoclonus
- Oligodendroglioma
- Vestibular Syndrome
Here we describe disorders other than epilepsy but which may include seizures among their signs and symptoms.
Canine Cognitive Dysfunction
Canine cognitive dysfunction (CCD) is the term which describes behavioral changes resulting in impairment of such qualities as awareness, perception, reasoning, and judgment. In dogs, it may be indicated by anxiety, disorientation in familiar places, altered sleep-wake cycles, reduced activity, "sundowning" (agitation, restlessness, pacing, barking in evenings and nights), interior urination and/or defecation. CCD episodes may be temporary or permanent and static or progressive. In dogs having epileptic seizures, CCD is common in idiopathic epilepsy (IE) and may be concurrent with their onset and/or continuation, but CCD may also be independent of such seizures. Epilepsy is believed to have a role in cognitive decline. See this February 2018 article and this January 2020 article.
Encephalitis
Encephalitis is inflammation of the brain, and autoimmune encephalitis occurs when the dog's immune system mistakenly attacks healthy brain cells, leading to that inflammation. GABA is the main inhibitory neurotransmitter in the brain, which enables the regulation of neuronal activity. GABAAR are ion channels in the brain control the rapid transmission of nerve impulses between neurons.
In a June 2022 article, German veterinary neurologists described the first reported case of a dog -- a 1-year-old cavalier -- diagnosed with anti-GABAAR (γ-aminobutyric acid-A receptor) autoimmune encephalitis. The cavalier (right) had multiple generalized seizures and showed alternating stupor and hyperexcitability, ataxia, repetitive muscle contractions, and circling to the left side. Auto-antibody encephalitis, with antibody-mediated dysfunction of receptors was suspected. Despite treatment with multiple antiseizure medications (diazepam followed by phenobarbital) the seizures and behavior abnormalities continued, and the dog alternated between stupors and hyperexcitability. Immunotherapy with dexamethasone, a corticosteroid, led to rapid improvement of the clinical signs and the CKCS improved continuously. A month later, GABAAR auto-antibodies had decreased significantly. An antibody search in the cerebral-spinal fluid (CSF) and serum located a neuropil staining pattern of GABAAR antibodies. At the examination four weeks after the start of immunotherapy, the dog was clinically normal; the GABAAR antibody titer in serum had strongly decreased; and the antibodies were no longer detectable in the CSF. The clinicians report that this is "the first veterinary patient with an anti-GABAAR encephalitis with a good outcome following ASM and corticosteroid treatment." They concluded:
"Based on the clinical signs and presentation (epileptic seizures lacking any response to ASMs, erratic behavioral changes) and the results of the initial diagnostics (lack of abnormal findings on conventional MRI and CSF examination), an autoimmune encephalitis was suspected, proven, and successfully treated. Clinicians should consider to test for autoantibodies and start immunotherapy in cases with a similar clinical presentation and lack of response to anti-seizure medication even if an inflammatory/infectious or neoplastic cause was clinically excluded on MRI and CSF."
Environmental Causes
In a December 2021 article, a 4-month-old cavalier with localized seizures -- head nodding and eyelid twitching -- was suspected of epilepsy. However, further examination revealed that a grass seed was lodged within the gums near a molar tooth. Once the seed was surgically removed, the dog's clinical symptoms disappeared. The clinicians determined that an inflammatory reaction caused pain (neuralgia) at the trigeminal nerve, that resulted in the head nodding and twitching. They recommended that trigeminal neuralgia be considered as a differential diagnosis of facial seizures before starting any anti-epileptic treatments.
Flycatcher's Syndrome
Symptoms similar to those of idiopathic epilepsy may be due to other causes. It is to be distinguished from Flycatcher's Syndrome, which is a separate disorder of the CKCS. It also is to be distinguished from malformations of the skull, including either meningoencephalocele (MEC), which is a herniation of cerebral tissue and meninges through a defect in the cranium, or a meningocele (MC), a herniation of the meninges alone. See this January 2017 article.
Myoclonus
Myoclonus is a syndrome displaying symptoms of spasmodic jerky contractions of groups of muscles, mainly of the head (such as, rapid eye movements, nodding, or shuddering) and forelimbs when the dog is standing or sitting. The syndrome can be progressive with affected dogs suffering frequent jerks which may cause the dog to fall or stumble.
Oligodendroglioma
Oligodendroglioma is a tumor located in glial cells in the dog's brain. it is a common tumor in dogs and humans and is graded by the World Health Organization (WHO) by its severity and malignancy. WHO grade 2 tumors are called "low-grade", which typically grow slowly, and respond to treatments such as chemotherapy, radiation, and surgery. WHO grade 3 tumors are "high-grade" and are cancerous, aggressive, and spread rapidly.
In a 2022 abstract, the clinicians reported the case of a 9 month old female cavalier which had a 3 month history of sudden onset episodes of pain and scratching at the neck. The signs progressed over the following 3 years to generalized tonic-clonic epileptic seizures progressed within 48 hours to the point of stupor, cardiac arrest and death. Post-mortem examination revealed that the tumor was "an anaplastic oligodendroglioma (WHO grade III) with subarachnoidal and intraventricular drop metastasis".
Vestibular Syndrome
Vestibular syndrome symptoms may be confused with epileptic signs. In particular, vestibular epilepsy (VE) is described as focal seizures with vestibular disease as the only or main symptom. The signs range from mild disequilibrium to dizziness and vertigo. These seizures tend to have a short duration of even just a few seconds to minutes and an abrutp ending. Diagnosis of VE may be confused with vestibular paroxysmia (VP), a much rarer disorder among dogs. consisting of brief episodes of spinning or non-spinning vertigo. In this March 2024 article, VE was diagnosed in 10 dogs, including a cavalier King Charles spaniel. The episodes of VE in this study were recurrent, as may be epileptic seizures. See the linked article for details. Its authors suspect an epileptic origin for the VE episodes. See our Vestibular Disorders webpage.
RETURN TO TOP
Diagnosis
All
dogs should be examined by a veterinarian after their first seizure for
determination of the cause. Diagnosing epilepsy in dogs is difficult. It begins by attempting to rule out
other causes for the seizures. Some cases of epileptic seizures have a specific structural cause. The age of onset, breed, weight, historical findings, and
neurological exam findings are important in estimating the likelihood that there
is a structural problem and therefore a specific treatment and prognosis.
structural cause. The age of onset, breed, weight, historical findings, and
neurological exam findings are important in estimating the likelihood that there
is a structural problem and therefore a specific treatment and prognosis.
Video recordings of the dog during the event can be very helpful to the treating veterinarian in diagnosing the cause. The most useful type of video is of the dog moving about during the seizure event.
Since diagnosis of idiopathic epilepsy is largely a "rule out" effort, other tests would be performed to rule out other underlying causes. They include:
Blood tests
Urinalysis
Neurological examination
Metabolic disoders testing
Infectious diseases testing
Autoimmune encephalitis antibody titers
Cerebrospinal fluid (CSF) analysis
DNA testing
 Other possible disorders, such as vestibular
disease, may be diagnosed instead of epilepsy becasue their symptoms
can be similar in sume cases.
Other possible disorders, such as vestibular
disease, may be diagnosed instead of epilepsy becasue their symptoms
can be similar in sume cases.
The electroencephalogram (EEG) (right) is a frequently used device in diagnosing epilepsy. Electroencephalography uses electrodes that detect the flow of electrical current between the cells of the brain, spinal cord, heart, and other organs, to view brain function. EEG provides data regarding nerve cell activity. However, EEG has some serious drawbacks in animals.
Advanced imaging, such as magnetic resonance imaging (MRI) (left) or computed tomography (CT) scans, is necessary to be able to actually see the structure of the brain. By imaging the brain, veterinarians are able to diagnose diseases such as brain tumors or hydrocephalus (water on the brain) which can cause seizures. Essentially, MRI scans serve to rule out structural abnormalities. Veterinary neurologist Dr. Clare Rusbridge published two YouTube videos on MRI scanning epilepsy patients in May 2024. The first one is titled "Epileptic pet -- should I get a MRI?", and the second one is "MRI Epilepsy Protocol for pets: A Step-by-Step Guide".
In a September 2015 article, the International Veterinary Epilepsy Task Force issued a consensus proposal on diagnosing epilepsy in dogs. They outlined "two fundamental steps: to establish if the events the animal is demonstrating truly represent epileptic seizures and if so, to identify their underlying cause." They then described a three-tier system for the diagnosis of idiopathic epilepsy (IE):
"Tier I confidence level for the diagnosis of IE is based on a history of two or more unprovoked epileptic seizures occurring at least 24 h apart, age at epileptic seizure onset of between six months and six years, unremarkable inter-ictal physical and neurological examination, and no significant abnormalities on minimum data base blood tests and urinalysis.
Tier II confidence level for the diagnosis of IE is based on the factors listed in tier I and unremarkable fasting and post-prandial bile acids, magnetic resonance imaging (MRI) of the brain (based on an epilepsy-specific brain MRI protocol) and cerebrospinal fluid (CSF) analysis.
Tier III confidence level for the diagnosis of IE is based on the factors listed in tier I and II and identification of electroencephalographic abnormalities characteristic for seizure disorders. The authors recommend performing MRI of the brain and routine CSF analysis, after exclusion of reactive seizures, in dogs with age at epileptic seizure onset <6 months or >6 years, inter-ictal neurological abnormalities consistent with intracranial neurolocalisation, status epilepticus or cluster seizure at epileptic seizure onset, or a previous presumptive diagnosis of IE and drug-resistance with a single antiepileptic drug titrated to the highest tolerable dose. This consensus article represents the basis for a more standardised diagnostic approach to the seizure patient. These recommendations will evolve over time with advances in neuroimaging, electroencephalography, and molecular genetics of canine epilepsy."
RETURN TO TOP
Treatment
- primary drugs
- secondary drugs
- surgery
- natural alternative remedies
- dietary remedies
- neurostimulation
 Any
seizure lasting more than five minutes would be an emergency case
requiring immediate veterinary care. If the dog remains unconscious
following convulsions, that sign also calls from immediate care.
Any
seizure lasting more than five minutes would be an emergency case
requiring immediate veterinary care. If the dog remains unconscious
following convulsions, that sign also calls from immediate care.
Immediately after a seizure, the dog should be handled with caution. The dog likely will pant after a seizure, due to heat generated by the intense brain activity and seizure. Cool, wet compresses place at the base of the skull and in the groin area will help decrease the body temperature. The dog should be offered a drink of water, but should not be left unattended with a water bowl.
The owner should keep a calendar noting the frequency of the seizures, and the dog that seizures more than once a month should treated long term with anti-convulsants. The patient on any of these drugs should be monitored closely for effectiveness and any adverse reactions. Monitoring includes frequent blood testing.
Medical treatment for frequent and/or long-lasting seizures should be started as quickly as possible, because such seizures can have serious consequences to the brain, heart, bladder, kidneys, and other essential organs.
Most of the medications described below are labeled "anti-seizure drugs (ASDs)" or "anti-seizure medications (ASMs)". Unfortunately, however, less than 50% of dogs treated with these anti-convulsants become seizure-free without significant side-effects. Typical adverse reactions to ASDs are: ataxia (loss of the ability to coordinate muscular movement), lethargy, increased thirst, and increased appetite. The ASDs associated with increased appetite have been phenobarbital, imepitoin, potassium bromide, zonisamide, and levetiracetam. These drugs are discussed in some detail below.
In general, the side effects from most conventional ASDs may reduce the dogs' quality of life, due to blood and liver toxicity. Periodic bloodwork monitoring to check for changes in liver conditions is recommended.
• primary drugs
The four drugss considered most effective in the initial treatment of epilepsy by many clinicans are phenobarbital (PB), potassium bromide (KBr), zonisamide (ZNS), and imepitoin. They are called "primary drugs" because one of them, or a combmination of them, is most frequently prescribed and in many cases may be the only treatment ever prescribed for affected dogs which respond well to them.
Medication will usually not eliminate seizures entirely, and is considered effective if a seizure occurs no more than every four to six weeks. Any time the dog exhibits a cluster of seizures, the veterinarian should be consulted, and may require immediate emergency treatment by the veterinarian, due to the possibility of permanent brain damage.
In an October 2014 report, UK researchers found evidence to support the efficacy of oral phenobarbital and imepitoin and a "fair level of evidence" to support the efficacy of oral potassium bromide and levetiracetam. However, for zonisamide, primidone, gabapentin, pregabalin, sodium valproate, felbamate, and topiramate, they found "insufficient evidence to support their use due to lack of bRCTs [blinded randomized clinical trials]". They concluded that "there is a need for greater numbers of adequately sized bRCTs evaluating the efficacy of AEDs [antiepileptic drugs] for IE."
Anti-convulsants (ASMs) do not always work. For example, in a June 2022 article, German veterinary clinicians report a case of a 1-year-old cavalier which had endured multiple generalized tonic-clonic epileptic seizures, episodic hyperexcitability alternating with episode of stupor, and intermittent left circling behavior. The CKCS did not respond to multiple ASMs -- diazepam followed by phenobarbital. An autoimmune encephalitis was suspected, and GABAAR antibodies were detected in his blood serum and cerebral-spinal fluid (CSF), confirming a diagnosis of anti-GABAA receptor encephalitis. The cavalier recovered following treatment of immunotherapy with corticosteroids.
Phenobarbital
Oral phenobarbital (PB) (Epiphen, Soliphen, Solfoton, Luminal, Phenoleptil) may be started once the seizures recur frequently. This drug lowers the neuron activity in the dog’s brain. It probably is the most effective drug, particularly for dogs suffering from severe epilepsy (having a tonic-clonic seizure or grand mal seizue more frequently than every two months). The usually starting dose is 3mg/kg every 12 hours. Administering this drug requires blood sampling periodically, starting at 2 weeks following the first dose. Phenobarbital has potential adverse effects, including drowsiness, inactivity, loss of coordination (ataxia), increased appetite and weight gain, and liver enzyme issues. Daily doses should not exceed 12 mg/kg to avoid liver dysfunction. The range of serum concentration should be 120-130 µmol/l (25-35 mg/l).
For more information on phenobarbital in treating epilepsy, watch this YouTube video by Dr. Clare Rusbridge.
In a February 2016 report, an international panel of veterinary neurologists and other specialists published a "2015 ACVIM Consensus Statement" on seizure management in dogs based on current literature and clinical expertise, authorized by the American College of Veterinary Internal Medicine (ACVIM). In that report, they rated phenobarbital, "High recommendation and likely be effective treatment."
Potassium bromide (KBr)
Another anti-convulsant medication is potassium bromide (KBr) (Bromav, Epilease, KBroVet-ca1, Libromide). In the February 2016 report in which an international panel of veterinary neurologists and other specialists published a "2015 ACVIM Consensus Statement" on seizure management in dogs based on current literature and clinical expertise, those authors gave potassium bromide a "Moderate recommendation and most likely to be effective treatment."
KBr does not cause liver problems because it is eliminated by the kidneys. Common side effects are increased drinking and urination, increased appetite and weight gain, sedation, and a wobbly gait, mainly in the rear legs.
Excessive intake of bromide may result in bromide toxicity, resulting in severe paralysis and twitching and excessively high levels of chlorine in the blood stream. See this section on bromide toxicity for a discussion of veterinary journal articles reporting bromide toxicity in cavaliers.
In an April 2014 report, a cavalier suffered loss of muscle control and repetitive leg twitching due to an overdose of potassium bromide. Also, 30% of dogs treated with these drugs still will demonstrate poor seizure control or chronic resistance to the drugs.
Zonisamide
Zonisamide (ZNS) (Zonegram) is an anticonvulsant which in clinical trials appears to be effective for generalized seizures in dogs. It’s anti-seizure effect is believed to work through sodium and calcium channels. The 2015 ACVIM Consensus Statement rated zonisamide, "Low recommendation and may not be effective treatment." A May 2024 article concluded that zonisamide "is effective and well-tolerated in dogs with newly diagnosed IE." However, some owners of affected dogs report that it appears to cause their dogs to develop mobility problems and pehaps increase liver values.
When combined with phenobarbital (PB), the PB will increase elimination of ZNS, and so the dog may need a higher dose of ZNS to offset this side effect. Dr. Curtis Dewey reports that "There are two reports of liver failure in dogs associated with zonisamide; a subsequent investigation showed that the likelihood of this happening is less than 1%."
Imepitoin
Imepitoin (Pexion, ELB138) is available in the UK and Europe but not in the USA. Imepitoin is a centrally acting antiepileptic substance which inhibits seizures by acting on a specific receptor in the brain cells to reduce the amount of excessive electrical activity present, in order to reduce the number of seizures the dog experiences. In addition, imepitoin has a weak calcium-channel-blocking effect. See this April 2015 report discussing its safety and effectiveness. In the 2015 ACVIM Consensus Statement, the panel gave imepitoin a "High recommendation and likely be effective treatment."
In a February 2017 article, Belgium researchers tested adding phenobarbital or potassium bromide as additional drugs for treatment with imepitoin. These drugs were evaluated in 27 dogs by comparing monthly seizure frequency (MSF), monthly seizure day frequency (MSDF), the presence of cluster seizures during a retrospective 2-month period with a prospective follow-up of 6 months, and the overall responder rate. They concluded that when idiopathic epilepsy is not well controlled with maximum doses of imepitoin alone, either phenobarbital or potassium bromide can be an effective add-on drug which decreases median MSF and MSDF in epileptic dogs unmanageable with a maximum dose of imepitoin. They stated that combination therapy was generally well tolerated and resulted in an improvement in seizure management in the majority of the dogs.
Others
An initial anti-convulsant medication often may be a benzodiazepine (diazepam [Valium], alprazolam, clonazepam, lorazepam), a category of psychoactive drugs which act as tranquilizers by blocking neurotransmitters in the dog’s brain. They are not recommended for dogs with liver or kidney disorders. Side effects in some dogs include diarrhea, vomiting, loss of coordination, and a reduced heart rate.
A July 2006 study of the use of acepromazine maleate (i.e., acetylpromazine), which is a common sedative administered to dogs, involved administering it for tranquilization during hospitalization to 36 dogs with a prior history of seizures and to 11 other dogs to decrease seizure activity. No seizures were observed within 16 hours of its administration in the 36 dogs that received the drug for tranquilization, and seizures abated for from 1.5 to 8 hours or did not recur in 8 of 10 of the 11 dogs that had been actively seizing. Also, excitement-induced seizure frequency was reduced for 2 months in one dog.
• secondary drugs
Secondary drugs are those which may be added to any of the primary drugs if and when the primary drugs do not manage the condition by themselves. In some cases, some clinicians may choose to prescribe a secondary drug as a sole initial treatment.
Levetiracetam
Levetiracetam (Keppra, Elepsia, Spritam) is an anticonvulsant which can also be used in conjunction with phenobarbital and/or potassium bromide. it appears to be relatively safe for dogs, and reportedly rarely has any adverse side effects and does not appear to affect the liver or liver enzymes. In a July 2014 study, researchers found that the adding phenobarbital to a dosage of Levetiracetam significantly altered the disposition of the levetiracetam. See, also, this February 2015 study. The 2015 Consensus Statement rated levetiracetam, "Low recommendation and may not be effective treatment."
In a November 2015 article, six of twelve affected dogs were treated solely with levetiracetam and six were treated solely with phenobarbital. The researchers found that, in the levetiracetam treated dogs, there was no significant difference in the monthly number of seizures before and after treatment, whereas in the phenobarbital treated dogs, there were "significantly fewer seizures after treatment". They concluded that: "In this study levetiracetam was well tolerated but was not effective at the given doses as mono-therapy in dogs with idiopathic epilepsy."
In a May 2007 article, North Carolina State University clinicians reported on a 6-month-old cavalier which had seizures over the period of a year, which were difficult to control with standard anti-convulsants. They diagnosed anorganic aciduria with excessive excretion of hexanoylglycine when the dog was 20 months old. Recurrent and cluster seizures were eventually controlled with the addition of levetiracetam to potassium bromide and phenobarbital.
When combined with phenobarbital (PB), the PB will increase elimination of levetiracetam, and so the dog may need a higher dose of levetiracetam to offset this side effect.
Gabapentin
The anti-convulsant gabapentin (Neurontin, Gabarone) is being prescribed, following an October 2010 study which has shown that between 41% and 55% of dogs have responded to it. Gabapentin works through a receptor on the membranes of brain and peripheral nerve cells. It binds to calcium channels and modulates calcium influx as well as influences GABergic neurotransmission. In humans, gabapentin reportedly does not interact with any other medications, and it is not metabolized, so it is fully excreted in the urine and has no affect upon the liver. However, in dogs, gabapentin is partially metabolized in the liver, and therefore the prescribing neurologist may be expected to order periodic blood tests to check the liver enzymes.
In an October 2018 article, Turkish veterinarians report on the diagnosis and treatment of a 3-year-old neutered female cavalier diagnosed with mitral valve disease which began to experience epileptic seizures. The epilepsy first was treated with levetiracetam, which resulted in the epileptic seizures disappearing. Then, three months later, the cavalier was treated for fleas and ticks with fipronil (Frontline TopSpot, Fiproguard, Flevox, PetArmor). The epileptic attacks "dramatically increased and became more severe just after the fipronil treatment (~7 times per day)." Gabapentin was added to the levetiracetam treatment protocol, and the epileptic seizures. The researchers concluded:
"Fipronil, phenylpyrazole origin and other antiparasitic drugs should be used very carefully and under veterinary consultant supervision due to their side effects especially in epileptic dogs. Finally, gabapentin could be a good option for the alternative add-on therapy to control epileptic seizures in CKCSs."
Oddly, the 2015 ACVIM Consensus Statement does not mention gabapentin.
Pregabalin
A newer anti-convulsant, pregabalin (Lyrica, Accord, Alzain, Lecaent, Milpharm, Prekind, Rewisca, Sandoz, Zentiva), is being prescribed by some neurologists. Dr. Curtis Dewey, board certified veterinary neurologist at Cornell University's college of veterinary medicine, has reported that 78% of dogs responded to pregabalin, and that there was a 57% mean reduction in seizures for the participants who finished the study; all had been diagnosed with difficult-to-control seizures. For more details, see this December 2009 report.
Pregabalin is closely related to gabapentin and was developed by Pfizer, which also developed gabapentin. Pfizer reports that pregabalin is more potent than gabapentin and achieves its effect at lower doses. Doses of pregabalin also reportedly have a longer lasting effect than gabapentin. In a May 2016 study of six brands of pregabalin, the researchers found that "all brands are pharmaceutically equivalent in their quality aspects." They concluded that the lower cost brands of pregabalin could be used to treat epilepsy. The rearchers do not identify the names of the six brands of pregabalin.
Oddly, the 2015 ACVIM Consensus Statement does not mention pregabalin.
Others
Other anti-convulsants, such as topiramate (Topamax), lamotrigine (Lamictal), oxcarbazepine (Trileptal), tiagabine (Gabitril), primidone, sodium valproate, and felbamate (felbatol) may be prescribed. Dr. Rusbridge provides a detailed discussion of topiramate on her YouTube channel at this link.
Ketamine (Ketalar) is an intraveous NMDA used as an induction and maintenance agent for sedation and to provide general anesthesia. It is being used more frequently in treatind CM/SM dogs which no longer respond to gabapentin and pregabalin. It blocks sensory perception in humans. It reportedly provides pain relief and controls symptoms of epilspsy.
RETURN TO TOP
• surgery
It is estimated that roughly 30% of dogs diagnosed with epilepsy do not respond to anti-seizure drugs. The alternative option in such cases, other than neurostimulation and/or dietary changes, is a form of surgery called corpus callostomy, described below. Other neurosurgical procedures are performed on humans but not yet on dogs. They are categorized as "resection", "disconnection", and "neurostimulation" surgeries.
corpus callostomy
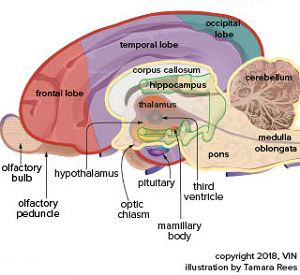 The
corpus callosum is a thick band of nerve fibers (called "commissural
fibers") beneath the cerebral
cortex in the brain, which connects the two hemispheres of the brain and
enables communication between them. It is divided into four parts:
rostrum, genu, body, and splenium.
The
corpus callosum is a thick band of nerve fibers (called "commissural
fibers") beneath the cerebral
cortex in the brain, which connects the two hemispheres of the brain and
enables communication between them. It is divided into four parts:
rostrum, genu, body, and splenium.
A corpus callosotomy (CC) is an intra-cranial surgical procedure to treat epileptic seizures if medications are not successful. It is estimated that roughly 30% of dogs diagnosed with epilepsy do not respond to anti-seizure drugs.
The CC procedure involves cutting all parts or fewer of the band of fibers which make up the corpus callosum. Afterward, the nerves no longer can send seizure signals between the brain’s two hemispheres, making seizures less severe and frequent and may stop them completely. This type of procedure is labeled "disconnection surgery" because it involves a partial severing of a neuronal connection to inhibit the spreading of the seizure activity.
In a November 2021 article, Japanese veterinary neurology specialists performed corpus callosotomies on three cavalier King Charles spaniels diagnosed with drug-resistant epilepsy (DRE). In Case #1, the cavalier required two partial CC surgeries (retaining only the splenium), because the first one ultimately did not reduce the frequency or severity of seizures. Two-plus years after the second surgery, the frequency of seizures was reduced by 93.4%. "The dog’s consciousness and activity improved after both surgeries", and "the patient showed positive behavior, running around and playing with toys with her owners." In Case #2, by a year following a total CC surgery, the seizure rate was reduced by 100%. The cavalier in Case #3 died immediately after partial CC surgery (retaining the genu) of cardiopulmonary arrest, possibly due to mitral valve disease but not confirmed.
multiple subpial transection
Multiple subpial transection (MST) is a disconnection surgery aimed at stopping seizures but preserving areas of the cortex which control functions, such as sensory, language, and motor actions. These also are known as "eloquent" areas of the cortex. In an October 2020 abstract, two laboratory dogs diagnosed with idiopathic epilepsy originating in the frontal lobe. MST surgery was performed in the area where epileptic discharges (ED)were recorded by electrocorticography (ECoG) until the discharges almost disappeared. Both dogs were followed up for seven years and showed no neurological abnormalities following discharge after surgery. ED was observed less frequently and not in the area where MST was performed, for 27 months afterward.
RETURN TO TOP
• natural alternative remedies
In a 2004 article, Dr. H. C. Gurney of Colorado reports success in treating dogs during epileptic seizures by applying ice directly to the dogs' backs at T10 to L4 of the spine. They summarized:.
"Fifty-one epileptic canine patients were successfully treated during an epileptic seizure with a technique involving the application of ice on the back (T10 to L4). This technique was found to be effective in aborting or shortening the duration of ictus. ... Ice is applied as soon as the seizure is observed. Theapplication itself is either a block of ice (i.e., water frozen in a metal ice tray, with the tray applied directly to the seizing patient), or ice (cubes or crushed ice in a plastic bag). The ice is held firmly to the dog’s back, on the area superior to the spinal process from T10 (palpable at the 'low spot' on the canine spine) to L4 (Figure at right). The size of a given ice application is sufficient to cover the described area. Maintain firm pressure in that location until the patient spontaneously recovers sternal recumbency and makes efforts to rise and walk. If the patient is prone to 'chain' episodes or displays evidence of returning to ictus after removal of the ice, the ice should once again be applied until the patient regains sternal recumbence (when chain seizures occur, aggressive medical intervention is necessary). Clients have used bags or boxes of frozen vegetables, but such applications are reported to be less effective. ... The sooner ice was applied during an epileptic event, the more effective the intervention was in stopping or abbreviating the seizure. Also of note was the observation that the canines’ post-ictus recovery time was shorter, and recovery appeared to be augmented."
Holistic veterinarians who practice Traditional Chinese Medicine use acupuncture, Chinese and Western herbal therapy, nutrition, veterinary chiropractic, homeopathy, and homotoxicology as treatment therapies which may be highly beneficial for treating epileptic conditions and other seizures, where a conventional approach either fails to provide relief or produces unacceptable side effects. In a January 2007 article, the researcher reported the success in treating ten affected dogs affected with homeopathic Belladonna therapy.
Traditional Chinese herbal medicines (TCM) and other holistic supplements should be taken only if prescribed by a licensed veterinarian who also is holistically trained in TCM. Search webpages for finding holistic veterinarians in the United States are located here and here.
 Cannabinol (CBD
oil) is produced from hemp and marijuana (Cannabis
Sativa) plants. CBD oil mimics the endocannabinoid molecules which the
dog’s (and our) body produces in several different organs. They play
roles in reducing pain, regulating inflammation, and affecting the
immune system, by initially binding to receptors in the brain.
Recommended dosages very widely, from 0.25 mg per kg per day to as much
as 9 mg/kg/day (for epilepsy). However, the maximum recommended dose for
adult humans is only 0.15 mg/kg/daily, the equivalent of 5 drops of 5%
CBD oil.
Cannabinol (CBD
oil) is produced from hemp and marijuana (Cannabis
Sativa) plants. CBD oil mimics the endocannabinoid molecules which the
dog’s (and our) body produces in several different organs. They play
roles in reducing pain, regulating inflammation, and affecting the
immune system, by initially binding to receptors in the brain.
Recommended dosages very widely, from 0.25 mg per kg per day to as much
as 9 mg/kg/day (for epilepsy). However, the maximum recommended dose for
adult humans is only 0.15 mg/kg/daily, the equivalent of 5 drops of 5%
CBD oil.
Varieties of CBD: Cannabidiol-based veterinary products are derived mainly from hemp (Cannabis sativa) and must contain less than 0.3% tetrahydrocannabinol (THC). This form of CBD can be processed into “full spectrum” or “broad spectrum” and also may be in the form of a “distillate”, in which all THC has been removed, or in the form of CBD “isolate”, which is a purifed powder.
• Full Spectrum: Full spectrum CBD contains other extracts found in the cannabis plant, including terpenes, and up to 0.3% THC.
• Broad Spectrum: Broad spectrum CBD also contains some other cannabis compounds but no more than trace amounts of THC.
• CBD Isolate: CBD isolate is pure CBD and contains no other cannabis plant compounds.
• Naked CBD: Naked CBD describes CBD oil by itself, as opposed to being capsultated or microcapsulated or combined with any other substance, such as deoxycholic acid (DCA).
• Liposomal CBD: This is an orally administered encapsultated CBD which is packaged within liposomes, small fatty cellular sacs which improve bioavailability of the CBD by enabling it to be withstand digesstion in the stomach and degradation in the liver. Lipsomal CBD was tested on dogs in this September 2020 article.
• Cannabidiolic acid (CBDA) is an acid precursor of CBD. It forms CBD when heated. It has been shown in some studies to be more potent that CBD for treating rats. It has been found to be more readily absorbed into the human bloodstream than CBD. Aa theory is that adding CBDA to doses of CBD may make the CBD more absorbable. In this September 2020 article, the investigators found that CBDA is absorbed at least twice as well as CBD in dogs within a 24 hour period, with some differences depending upon the medium used to deliver the oral treatment.
 Otherwise untreatable (refractory or intractable) seizures attribured to idiopathic
epilepsy has been the most promising category of disorders responding to
CBD. Again, the numbers of participating dogs have been exceedingly low,
but for the most part, the success rates have been fairly high. In each
of the published studies thus far, the affected dogs continued to be
treated with their previously prescribed antiseizure drugs (ASD).
Otherwise untreatable (refractory or intractable) seizures attribured to idiopathic
epilepsy has been the most promising category of disorders responding to
CBD. Again, the numbers of participating dogs have been exceedingly low,
but for the most part, the success rates have been fairly high. In each
of the published studies thus far, the affected dogs continued to be
treated with their previously prescribed antiseizure drugs (ASD).
As an "add-on" treatment, a very high does of 9 mg/kg of CBD twice a day may have some benefit, but at the risk of impacting the liver.
In a June 2019 article, 9 dogs with intractable idiopathic epilepsy received CBD-infused oil (2.5 mg/kg) twice daily for 12 weeks in addition to their existing antiepileptic treatments. Seven other dogs were in a placebo group. All 9 dogs in the CBD group experienced a reduction in the frequency of seizures, with a 33% median change. However, only 2 dogs were considered responders to the treatment, as defined by reducing seizure frequency by at least 50%. The CBD group dogs also had significant increases in their serum ALP levels by the end of the 12 weeks. The investigators concluded by recommending additional research being necessary to determine the effect of oral CBD treatments on seizure frequency in dogs with epilepsy.
In a July 2022 article, 14 dogs diagnosed with epileptic seizures which were only partially responsive to conventional medications (refractory) were treated orally with a CBD and CBDA-rich hemp product at 2 mg/kg orally every 12 hours for 12 weeks. The dogs also continued to be treated with their prescribed medications. Epileptic seizure frequency decreased. Six of the 14 dogs (43%) experienced a 50% or higher reduction in epileptic activities while being treated with the CBC/CBDA-rich hemp extract. Adverse events included somnolence (drowsiness/strong desire to sleep) and increases in ataxia (loss of coordination). The investigatore concluded that CBD/CBDA-rich hemp extract, in conjunction with other medications, appears safe and can have benefits in reducing the incidence of epileptic seizures.
In a
November 2023 article, two separate and different studies of
treating epiletic dogs with CBD were reported, involving a total of 51
dogs. All of the dogs previously had at least 2 seizures per month while
being treated with at least one antiseizure drug (ASD), most commonly
phenobarbital and/or levetiracetam. The CBD being used was
full-spectrum, containing approximately 100 mg/mL of CBD with trace
amounts of other cannabinoids. The other ingredients were cold-pressed
hemp seed oil and chicken flavoring
The dogs continued to be
administered their prescribed ASDs during these studies.
In the first of these two November 2023 studies, 12 of the dogs were treated with 2.5 mg/kg of CBD oil twice daily for 3 months, without evidence of a treatment effect. In the second study, 39 dogs were treated with 4.5 mg/kg of CBD oil twice daily for 3 months. The overall result of the second study was a 24.1% decrease in seizure activity. The investigators recommended that potential interactions between the CBD and phenobarbital "warranted continued investigation." They concluded that:
"Cannabidol shows promise as an anticonvulsant and warrants further investigation. Care should be taken to monitor liver enzyme activity and bile acid concentrations when this drug is administered chronically to dogs."
See our Cannabis webpage for additional details about CBD, including delivery methods, bioavailability, dosages, and adverse reactions.
RETURN TO TOP
• dietary remedies
Ketogenic diets*, which include adding medium chain triglycerides (MCTs), which provide the medium chain fatty acids and ketone bodies as auxiliary brain energy, have been shown to be beneficial in treating epiletptic dogs. However, the cavalier King Charles spaniel, as a breed, may be an exception to that general finding that MCTs are beneficial. See this webpage.
* Ketogenic diets are high in fat content (70% to 90% of total calories) and very low in carbohydrates (3% to 5% of total calories).
 In a
September 2015 article,
a team of UK researchers fed 21 dogs suspected to have idiopathic epilepsy,
including a cavalier, a dry food kibble
which was either a ketogenic medium-chain TAG (triacylglycerol) diet
(MCTD) or a placebo diet, for three months. Then the dogs were switched
from the one diet to the other for another three months. The results
overall showed that seizure frequencies were "significantly lower when
dogs were fed the MCTD in comparison with the placebo diet. The CKCS's
seizure frequency was reduced from 10 per month on the placebo diet to 5
per month while on the MCTD. The researchers concluded:
In a
September 2015 article,
a team of UK researchers fed 21 dogs suspected to have idiopathic epilepsy,
including a cavalier, a dry food kibble
which was either a ketogenic medium-chain TAG (triacylglycerol) diet
(MCTD) or a placebo diet, for three months. Then the dogs were switched
from the one diet to the other for another three months. The results
overall showed that seizure frequencies were "significantly lower when
dogs were fed the MCTD in comparison with the placebo diet. The CKCS's
seizure frequency was reduced from 10 per month on the placebo diet to 5
per month while on the MCTD. The researchers concluded:
"In conclusion, the data show antiepileptic properties associated with ketogenic diets and provide evidence for the efficacy of the MCTD used in this study as a therapeutic option for epilepsy treatment."
In a February 2016 report, the same team studied 21 dogs affected with idiopathic epilepsy (IE), feeding them a ketogenic MCTD for three months and then a placebo diet for three months. They were looking for attention-deficit/hyperactivity disorder (ADHD) behaviors in the dogs -- excitability, chasing, and trainability. They found that their "data support the supposition that dogs with IE may exhibit behaviors that resemble ADHD symptoms seen in humans and rodent models of epilepsy and that a MCTD may be able to improve some of these behaviors, along with potentially anxiolytic effects."
In February 2017, Purina announced the launch in the USA of a dry dog food for canine epilepsy patients. The food reportedly is based upon a September 2015 study by veterinary neurologist Dr. Holger Volk. Unfortunately, the ingredients* of this product are a common grain-laden mess of dry food with a few supplements at the end, totally expected from Purina. We cannot imagine how any of these vitamins and other supplements are kept fresh when combined in a bag of triple-cooked kibble. A healthful canned food combining fresh meats and vegetables, topped off with appropriate supplements tailored to the particular disorder and sealed in capsules to maintain freshness, would be much, much better than this joke of a recipe.
*INGREDIENTS: Chicken, chicken meal, corn gluten meal, brewers rice, ground yellow corn, ground wheat, medium-chain triglyceride vegetable oil, corn germ meal, barley, natural flavor, fish oil, dried egg product, L-Arginine, wheat bran, fish meal, mono and dicalcium phosphate, potassium chloride, salt, calcium carbonate, L-Lysine monohydrochloride, Vitamin E supplement, choline chloride, L-ascorbyl-2-polyphosphate (Vitamin C), zinc sulfate, ferrous sulfate, niacin, manganese sulfate, Vitamin A supplement, thiamine mononitrate, soybean oil, calcium pantothenate, Vitamin B-12 supplement, copper sulfate, riboflavin supplement, pyridoxine hydrochloride, garlic oil, folic acid, menadione sodium bisulfite complex (Vitamin K), calcium iodate, biotin, Vitamin D-3 supplement, sodium selenite.
In a November 2020 article, a multi-national team of veterinary reseachers tested the cognitive abilities of 29 dogs diagnosed with epilepsy by including MCT oil as a supplement to the dogs' food over the course of three months. They found from the 18 dogs which completed cognitive testing that consumption of MT oil as 9% of the dogs' total caloric intake that the dogs' spatial-working memory, problem-solving ability, and trainability improved. (See diagram below.) They also report that the MCT oil supplementation increased beta-hydroxybutyrate (BHB) serum concentration, which correlates with improvement in problem-solving tasks.
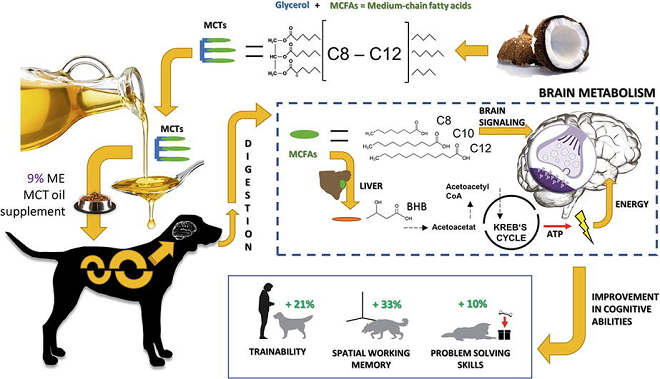
Are cavaliers an exception to the rule about MCTs being beneficial? Medium-chain acyl-coenzyme A dehydrogenase is an enzyme which is controlled by the ACADM gene. A protein-changing variant of the ACADM gene causes medium-chain acyl-coenzyme A dehydrogenase z9 (MCAD) deficiency. MCAD-deficiency is a presumably inherited disorder (an organic aciduria) that prevents the dog's body from converting certain fats to energy, particularly medium-chain fatty acids and particularly during periods without food. Two published studies suggest that MCAD deficiency is fairly common among CKCSs.
In particular, in an October 2022 study of 162 cavaliers, researchers found that 52 of them were carriers of the protein changing variant of ACADM, and another 12 cavaliers were homozygous mutant dogs. That research was prompted by examination of a 3 year old, male neutered cavalier which displayed complex focal seizures and prolonged lethargy. The dog was found to have a single insertion deletion variant of ACADM causing the MCAD deficiency. The affected dog was treated with various dosages of levetiracetam and phenobarbital and was prescribed a low fat diet and a midnight snack consisting of carbohydrates. Prolonged periods of fasting and formulas that contained medium chain triglycerides as primary source of fat were also advised to avoid.
The authors of the November 2020 article advise that MCT-enriched diets may be inappropriate for some CKCSs, based upon the findings of the October 2022 study. They report that they have been testing cavaliers for the ACADM mutation before recommending MCT-enriched diets for those dogs.
RETURN TO TOP
• neurostimulation
Neurostimulation of epileptic dogs involves stimulating the neural tissues to alter their electrical properties and chemical environment and also promoting glial cell activation and proliferation of neuronal progenitor cells. The current methods of neurostimulation of epileptic dogs include vagal (vagus) nerve stimulation (VNS), deep brain stimulation (DBS), and transcranial magnetic stimulation (TMS).
• vagal nerve stimulation (VNS)
The vagus nerve is located next to the trachea. Vagal nerve stimulation (VNS) is a procedure which involves implanting an electrical device under the skin, behind the shoulder blade and connected to the vagal nerve. The device sends impulses through the vagus nerve to the brain periodically with the intent of reducing seizures and their severity. In an October 2010 article, Dr. Curtis Dewey reported that vagal stimulators have "failed to demonstrate significant reduction of seizure activity" in dogs.
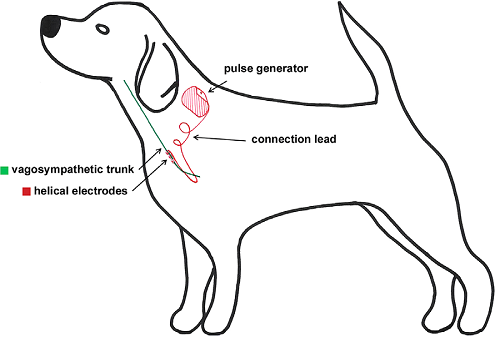 In
a January 2016
article, Belgium veterinary surgeons reported on the implantation of
VNS devices in a group of ten lab Beagles. They reported that
implantation was "safe and feasible in dogs; however, seroma formation,
twisting of the lead, and dislodgement of the anchor tether were
common." They recommended practical improvements in the technique,
including stable device placement, use of a compression bandage, and
exercise restriction. And they advised that regular evaluation of the
electric lead impedance was important, because altered values can result
in "serious complications".
In
a January 2016
article, Belgium veterinary surgeons reported on the implantation of
VNS devices in a group of ten lab Beagles. They reported that
implantation was "safe and feasible in dogs; however, seroma formation,
twisting of the lead, and dislodgement of the anchor tether were
common." They recommended practical improvements in the technique,
including stable device placement, use of a compression bandage, and
exercise restriction. And they advised that regular evaluation of the
electric lead impedance was important, because altered values can result
in "serious complications".
In a February 2017 article, Dr. Thomas Harcourt-Brown reports some vague success in implanting a VNS device in a UK border collie named Jago. He states:
"Although VNS is rarely curative of epilepsy in humans or dogs, we are very hopeful that that surgery will be effective in helping control Jago’s fits. In recent months his seizures have become so frequent that he has had difficulty in walking and eating. His device will need regular programming over the next few months to get to optimum settings. If it proves effective, it may be possible to reduce the amount of anti-seizure medications he has to take. Its early days yet but this treatment might offer hope for other families with epileptic dogs."
See also the application of vagus nerve stimulation being used experimentally to improve left ventricular dysfunction and slow the progression of heart failure in dogs, on our Mitral Valve Disease page.
• deep brain stimulation (DBS)
Deep brain stimulation (DBS) involves embedding an electronic
stimulator (right) into the nucleus of the dog's
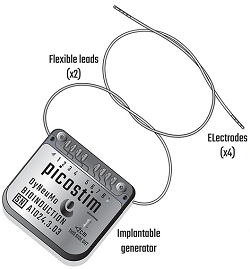 thalamus,
to select stimulation frequencies which should reinforce normal
physiological behavior and avoid pathological rhythms leading to
seizures. The goal is to reduce and possibly even eliminate epileptic
seizures.
thalamus,
to select stimulation frequencies which should reinforce normal
physiological behavior and avoid pathological rhythms leading to
seizures. The goal is to reduce and possibly even eliminate epileptic
seizures.
In a September 2021 case study article, a 4-year-old Newfoundland/Saint Bernard male with severe drug-resisant idiopathic epilepsy was treated with DBS which was programed with an integrated algorithm that allowed for stimulation to be adjusted to the ultradian, circadian and infradian patterns observed in the patient through slowly-varying adjustments of stimulationand which also enabled adaption of stimulation based on the immediate physiological needs such as a breakthrough seizure or change of posture. Prior to implantation, the dog experiecned cluster seizures which evolved to status epilepticus (SE - continuing attacks of epilepsy without intervals of consciousness, which could lead to brain damage and death) and required emergency treatment. The probes were implanted into the centromedian nucleus of the thalamus. Using combinations of time-based modulation, thalamocortical rhythm-specific tuning of frequency parameters as well as fast-adaptive modes based on activity, the dog experienced no further SE eventsand, no significant cluster seizures.
• transcranial magnetic stimulation (TMS)
Transcranial magnetic stimulation (TMS) is a non-invasive means of
low-frequency brain stimulation, using
 alternating
magnetic fields to create a secondary electric field in the affected
dog, primarily in the cortical areas of the brain. The device is a round
coil whihc rests on the sedated dog's skull. See photo at right.
alternating
magnetic fields to create a secondary electric field in the affected
dog, primarily in the cortical areas of the brain. The device is a round
coil whihc rests on the sedated dog's skull. See photo at right.
In an October 2020 article, seven dogs diagnosed with drug-resistant idopathic epilepsy were sedated and treated with the TMS device for an hour daily for five days. Five other dogs were similarly treated with a sham device. Then in a second phase of the study, the five sham-treated dogs also were treated with the active TMS device. Among the actively treated dogs, seizure frequency reportedly decrased significantly, with the overall effect lasting four months. Howevr, cluster seizures did not change significantly.
RETURN TO TOP
Breeders' Responsibilities
The Canine Inherited Disorders Database recommends that cavaliers which have had seizures should not be bred, nor should their parents and siblings.
RETURN TO TOP
What You Can Do
If your dog has a seizure, take these steps:
• Keep calm. Your dog can sense your emotions, so remain calm and reassuring.
• Keep the dog safe. Clear the area to prevent injury, moving any objects.
• Time the seizure. Write down its duration. If the episode lasts longer than 5 minutes or the dog has multiple seizures in a row, it becomes an emergency, so take the dog to a veterinary clinic immediately.
• Keep track of the symptoms. Write down which behaviors the dog had during the seizure. See the list above for examples.
• Video the seizure, if possible.
• Avoid physical contact with the dog. Do not hold the dog down during a seizure, and avoid contact with or near the dog’s mouth.
• Notify the veterinarian, for advice as to what to do next.
Flea and tick treatments which contain isoxazolines can increase the likelihood that dogs susceptible to seizures will experience them. Isoxazolines lower the threshold of seizures. These flea and tick products include Bravecto, Credelio, Nexgard, Revolution Plus, and Simparica Trio.
 The
Canine Epilepsy Project, led by
Dr. Ned Patterson, of the University of
Minnesota's College of Veterinary Medicine, and by Dr. Gary Johnson, of the
University of Missouri's College of Veterinary Medicine, is a collaborative
study into the causes of epilepsy in dogs. Its goal is to find the genes
responsible for epilepsy in dogs so that wise breeding can decrease the
incidence of the disease in dogs, and that, knowing what genes regulate epilepsy
in dogs may help better tailor therapy to the specific cause. Participation by owners of affected dogs and their relatives is essential to the success of this
project. Researchers need DNA samples from dogs who have experienced seizures,
and immediate relatives, both normal and affected. Specifically, they need
samples from all available siblings, parents, and grandparents. If the affected
dog has been bred, all offspring and mates should be sampled as well. Useful
research families are explained in more detail here. Participation in this
research project is confidential - the names of individual owners or dogs will
not be revealed. Data and DNA sample collection instructions and sample
submission forms are available on www.canine-epilepsy.net, or the packet will be
mailed or faxed upon request. Contact Liz Hansen, at the Animal Molecular
Genetics Laboratory, University of Missouri - College of Veterinary Medicine,
email hansenl@missouri.edu Go to the
Canine Epilepsy
Network website for more information.
The
Canine Epilepsy Project, led by
Dr. Ned Patterson, of the University of
Minnesota's College of Veterinary Medicine, and by Dr. Gary Johnson, of the
University of Missouri's College of Veterinary Medicine, is a collaborative
study into the causes of epilepsy in dogs. Its goal is to find the genes
responsible for epilepsy in dogs so that wise breeding can decrease the
incidence of the disease in dogs, and that, knowing what genes regulate epilepsy
in dogs may help better tailor therapy to the specific cause. Participation by owners of affected dogs and their relatives is essential to the success of this
project. Researchers need DNA samples from dogs who have experienced seizures,
and immediate relatives, both normal and affected. Specifically, they need
samples from all available siblings, parents, and grandparents. If the affected
dog has been bred, all offspring and mates should be sampled as well. Useful
research families are explained in more detail here. Participation in this
research project is confidential - the names of individual owners or dogs will
not be revealed. Data and DNA sample collection instructions and sample
submission forms are available on www.canine-epilepsy.net, or the packet will be
mailed or faxed upon request. Contact Liz Hansen, at the Animal Molecular
Genetics Laboratory, University of Missouri - College of Veterinary Medicine,
email hansenl@missouri.edu Go to the
Canine Epilepsy
Network website for more information.
RETURN TO TOP
Research News
November 2023:
Fecal transplants and MCT diet fail to reduce seizures in
cavalier with idiopathic epilepsy.
 In a
November 2023 article, veterinary researchers at the University of
Ghent (Fien Verdoodt [right], Myriam Hesta , Tijmen Willemse,
Luc Van Ham, Sofie Bhatti) reported the results of a variety of treatments of a 1.5 year old
female cavalier King Charles spaniel with a history of seizures due to
Tier II idiopathic epilepsy (IE). They started with anti-seizure
medications – first levetiracetam, then phenobarbital, followed by
potassium bromide – without success. Then they switched the cavalier’s
diet to a medium chain triglycerides dog food, Purina Pro Plan
Neurocare, also without a reduction in the frequency of seizures.
Finally, they performed a series of fecal (faecal) microbial transplants
(FMT) over a 10 week period. The FMTs resulted in a “negligible” and
“clinically irrelevant” reduction in seizure frequency. They concluded:
In a
November 2023 article, veterinary researchers at the University of
Ghent (Fien Verdoodt [right], Myriam Hesta , Tijmen Willemse,
Luc Van Ham, Sofie Bhatti) reported the results of a variety of treatments of a 1.5 year old
female cavalier King Charles spaniel with a history of seizures due to
Tier II idiopathic epilepsy (IE). They started with anti-seizure
medications – first levetiracetam, then phenobarbital, followed by
potassium bromide – without success. Then they switched the cavalier’s
diet to a medium chain triglycerides dog food, Purina Pro Plan
Neurocare, also without a reduction in the frequency of seizures.
Finally, they performed a series of fecal (faecal) microbial transplants
(FMT) over a 10 week period. The FMTs resulted in a “negligible” and
“clinically irrelevant” reduction in seizure frequency. They concluded:
“The lack of effect could be due to three main aspects. Firstly, the current protocol might have caused inadequate donor engraftment. 16sDNA sequencing will reveal performance of the protocol. Secondly, variable effects on MSF [mean seizure frequency] might be seen in different dogs, similar to medical and nutritional management of canine IE. Thirdly, the MGBA [microbiota-gut-brain axis] might not be an ideal target in the management of canine IE.”
 EDITOR’S NOTE: One possible other cause for the lack of success with
the fecal transplants could be the diet change to a medium chain
triglycerides (MCT) dog food. A significant percentage of CKCSs have
been found to have a medium-chain acyl-coenzyme A dehydrogenase z9
deficiency (MCADD) which actually causes seizures as one of its several
nasty side effects. However, the lead investigator, Dr. Verdoodt,
informs us that they did test the cavalier, Pippa, and she was negative
for the mutation. They also switched her daily food to a regular
maintenance diet.
EDITOR’S NOTE: One possible other cause for the lack of success with
the fecal transplants could be the diet change to a medium chain
triglycerides (MCT) dog food. A significant percentage of CKCSs have
been found to have a medium-chain acyl-coenzyme A dehydrogenase z9
deficiency (MCADD) which actually causes seizures as one of its several
nasty side effects. However, the lead investigator, Dr. Verdoodt,
informs us that they did test the cavalier, Pippa, and she was negative
for the mutation. They also switched her daily food to a regular
maintenance diet.
July 2023:
Epileptic cavalier resistant to treatment is diagnosed with
malformation of cortical development.
 In
a
July 2023 post on Facebook, UK veterinary neurologists Laurent
Garosi (right), Ines Carrera, and Simon Platt reported a case
study of a 2-year-old cavalier King Charles spaniel which has had severe
epileptic seizures since age 4 months. Despite treatment with
anti-seizure medications, the seizures continued to worsen to the point
of 3 to 4 episodes of cluster seizures lasting up to 48 hours. Using MRI
imaging, the clinicians diagnosed malformation of cortical development
(MCDs) based upon observing nodular lesions of neurons which had
migrated into abnormal locations – from adjoining white matter to gray
matter. They suspect the diagnosis is subependymal neuronal heterotopia,
but microscopic tissue study would be required to confirm the diagnosis.
They report that this disorder is very rare in dogs (and humans)
affected with MCDs.
In
a
July 2023 post on Facebook, UK veterinary neurologists Laurent
Garosi (right), Ines Carrera, and Simon Platt reported a case
study of a 2-year-old cavalier King Charles spaniel which has had severe
epileptic seizures since age 4 months. Despite treatment with
anti-seizure medications, the seizures continued to worsen to the point
of 3 to 4 episodes of cluster seizures lasting up to 48 hours. Using MRI
imaging, the clinicians diagnosed malformation of cortical development
(MCDs) based upon observing nodular lesions of neurons which had
migrated into abnormal locations – from adjoining white matter to gray
matter. They suspect the diagnosis is subependymal neuronal heterotopia,
but microscopic tissue study would be required to confirm the diagnosis.
They report that this disorder is very rare in dogs (and humans)
affected with MCDs.
October 2022:
Over 39% of cavaliers have medium-chain acyl-coenzyme A
dehydrogenase (MCAD) deficiency in a Swiss study.
 In
an
October 2022 Swiss study of 162 cavalier King Charles spaniels by
Matthias Christen, Jos Bongers, Déborah Mathis, Vidhya Jagannathan,
Rodrigo Gutierrez Quintana, and Tosso Leeb (right), they found
that 52 of them were carriers of the protein changing variant of the
ACADM gene, and another 12 cavaliers wer homozygous mutant dogs. That
research was prompted by examination of a 3 year old, male neutered
cavalier which displayed complex focal seizures and prolonged lethargy.
The dog was found to have a single insertion deletion variant of ACADM
causing medium-chain acyl-coenzyme A dehydrogenase (MCAD) deficiency.
The affected dog was treated with various dosages of levetiracetam and
phenobarbital and was prescribed a low fat diet and a midnight snack
consisting of carbohydrates. Prolonged periods of fasting and formulas
that contained medium chain triglycerides as primary source of fat were
also advised to avoid.
In
an
October 2022 Swiss study of 162 cavalier King Charles spaniels by
Matthias Christen, Jos Bongers, Déborah Mathis, Vidhya Jagannathan,
Rodrigo Gutierrez Quintana, and Tosso Leeb (right), they found
that 52 of them were carriers of the protein changing variant of the
ACADM gene, and another 12 cavaliers wer homozygous mutant dogs. That
research was prompted by examination of a 3 year old, male neutered
cavalier which displayed complex focal seizures and prolonged lethargy.
The dog was found to have a single insertion deletion variant of ACADM
causing medium-chain acyl-coenzyme A dehydrogenase (MCAD) deficiency.
The affected dog was treated with various dosages of levetiracetam and
phenobarbital and was prescribed a low fat diet and a midnight snack
consisting of carbohydrates. Prolonged periods of fasting and formulas
that contained medium chain triglycerides as primary source of fat were
also advised to avoid.
June 2022:
Cavalier with generalized tonic-clonic seizure due to autoimmune
encephalitis is successfully treated with steroids.
 In
a June
2022 article, German veterinary clinicians (Enrice I. Huenerfauth
[right], Christian G. Bien, Corinna Bien, Holger A. Volk, Nina
Meyerhoff) report a case of a 1-year-old cavalier King Charles spaniel
which had endured multiple generalized tonic-clonic epileptic seizures,
episodic hyperexcitability alternating with episode of stupor, and
intermittent left circling behavior. The CKCS did not respond to
multiple antiseizure medications (ASMs) -- diazepam followed by
phenobarbital. An autoimmune encephalitis was suspected, and GABAAR
antibodies were detected in his blood serum and cerebral-spinal fluid
(CSF), confirming a diagnosis of anti-GABAA receptor encephalitis. The
cavalier recovered following treatment of immunotherapy with
corticosteroids.
In
a June
2022 article, German veterinary clinicians (Enrice I. Huenerfauth
[right], Christian G. Bien, Corinna Bien, Holger A. Volk, Nina
Meyerhoff) report a case of a 1-year-old cavalier King Charles spaniel
which had endured multiple generalized tonic-clonic epileptic seizures,
episodic hyperexcitability alternating with episode of stupor, and
intermittent left circling behavior. The CKCS did not respond to
multiple antiseizure medications (ASMs) -- diazepam followed by
phenobarbital. An autoimmune encephalitis was suspected, and GABAAR
antibodies were detected in his blood serum and cerebral-spinal fluid
(CSF), confirming a diagnosis of anti-GABAA receptor encephalitis. The
cavalier recovered following treatment of immunotherapy with
corticosteroids.
December 2021:
Cavalier puppy's epileptic-like seizures were caused by a grass
seed lodged near its trigeminal nerve.
 In
a
December 2021 article by Andrea De Bonis (right), Oliver
Marsh, and Fabio Stabile, a 4-month-old cavalier with localized seizures
-- head nodding and eyelid twitching -- was suspected of epilepsy.
However, further examination revealed that a grass seed was lodged
within the gums near a molar tooth. Once the seed was surgically
removed, the dog's clinical symptoms disappeared. The clinicians
determined that an inflammatory reaction caused pain (neuralgia) at the
trigeminal nerve, that resulted in the head nodding and twitching. They
recommended that trigeminal neuralgia be considered as a differential
diagnosis of facial seizures before starting any anti-epileptic
treatments.
In
a
December 2021 article by Andrea De Bonis (right), Oliver
Marsh, and Fabio Stabile, a 4-month-old cavalier with localized seizures
-- head nodding and eyelid twitching -- was suspected of epilepsy.
However, further examination revealed that a grass seed was lodged
within the gums near a molar tooth. Once the seed was surgically
removed, the dog's clinical symptoms disappeared. The clinicians
determined that an inflammatory reaction caused pain (neuralgia) at the
trigeminal nerve, that resulted in the head nodding and twitching. They
recommended that trigeminal neuralgia be considered as a differential
diagnosis of facial seizures before starting any anti-epileptic
treatments.
November 2021:
Japanese neurologists perform brain surgery on three cavaliers
with drug-resistant epilepsy.
 In
a
November 2021 article, Japanese veterinary neurology specialists
(Rikako Asada, Satoshi Mizuno, Yoshihiko Yu, Yuji Hamamoto, Tetsuya
Anazawa, Daisuke Ito, Masato Kitagawa, Daisuke Hasegawa [right])
performed corpus callosotomies on three cavalier King Charles spaniels
diagnosed with drug-resistant epilepsy (DRE). The corpus callosum is a
thick band of nerve fibers beneath the cerebral cortex in the brain,
which connects the two hemispheres of the brain and enables
communication between them. It is divided into four parts: rostrum,
genu, body, and splenium. A corpus callosotomy (CC) is an intra-cranial
surgical procedure to treat epileptic seizures if medications are not
successful. The procedure involves cutting all parts or fewer of the
band of fibers which make up the corpus callosum. Afterward, the nerves
no longer can send seizure signals between the brain’s two hemispheres,
making seizures less severe and frequent and may stop them completely.
In
a
November 2021 article, Japanese veterinary neurology specialists
(Rikako Asada, Satoshi Mizuno, Yoshihiko Yu, Yuji Hamamoto, Tetsuya
Anazawa, Daisuke Ito, Masato Kitagawa, Daisuke Hasegawa [right])
performed corpus callosotomies on three cavalier King Charles spaniels
diagnosed with drug-resistant epilepsy (DRE). The corpus callosum is a
thick band of nerve fibers beneath the cerebral cortex in the brain,
which connects the two hemispheres of the brain and enables
communication between them. It is divided into four parts: rostrum,
genu, body, and splenium. A corpus callosotomy (CC) is an intra-cranial
surgical procedure to treat epileptic seizures if medications are not
successful. The procedure involves cutting all parts or fewer of the
band of fibers which make up the corpus callosum. Afterward, the nerves
no longer can send seizure signals between the brain’s two hemispheres,
making seizures less severe and frequent and may stop them completely.
In Case #1, the cavalier required two partial CC surgeries (retaining only the splenium), because the first one ultimately did not reduce the frequency or severity of seizures. Two-plus years after the second surgery, the frequency of seizures was reduced by 93.4%. "The dog’s consciousness and activity improved after both surgeries", and "the patient showed positive behavior, running around and playing with toys with her owners." In Case #2, by a year following a total CC surgery, the seizure rate was reduced by 100%. The cavalier in Case #3 died immediately after partial CC surgery (retaining the genu) of cardiopulmonary arrest, possibly due to mitral valve disease but not confirmed.
January 2021:
Medium-chain triglycerides at 9% caloric intake improved
cognition in 18 epileptic dogs.
 In
a
November 2020 article, a multi-national team of veterinary
reseachers (Benjamin Andreas Berk [right], Rowena Mary Anne
Packer, Tsz Hong Law, Annette Wessmann, Andrea Bathen-Nöthen, Tarja
Susanna Jokinen, Anna Knebel, Andrea Tipold, Ludovic Pelligand, Holger
Andreas Volk) tested the cognitive abilities of 29 dogs diagnosed with
epilepsy by including medium-chain triglycerides (MCT) oil as a
supplement to the dogs' food over the course of three months. They found
from the 18 dogs which completed cognitive testing that consumption of
MT oil as 9% of the dogs' total caloric intake that the dogs'
spatial-working memory, problem-solving ability, and trainability
improved. They also report that the MCT
oil supplementation increased beta-hydroxybutyrate (BHB) serum
concentration, which correlates with improvement in problem-solving
tasks.
In
a
November 2020 article, a multi-national team of veterinary
reseachers (Benjamin Andreas Berk [right], Rowena Mary Anne
Packer, Tsz Hong Law, Annette Wessmann, Andrea Bathen-Nöthen, Tarja
Susanna Jokinen, Anna Knebel, Andrea Tipold, Ludovic Pelligand, Holger
Andreas Volk) tested the cognitive abilities of 29 dogs diagnosed with
epilepsy by including medium-chain triglycerides (MCT) oil as a
supplement to the dogs' food over the course of three months. They found
from the 18 dogs which completed cognitive testing that consumption of
MT oil as 9% of the dogs' total caloric intake that the dogs'
spatial-working memory, problem-solving ability, and trainability
improved. They also report that the MCT
oil supplementation increased beta-hydroxybutyrate (BHB) serum
concentration, which correlates with improvement in problem-solving
tasks.
November 2018:
Cavalier's epilepsy is aggravated by tick/flea anti-parasite
drug fipronil and treated with levetiracetam and gabapentin.
 In
an
October 2018 article, a team of Turkish veterinarians (Sinan Kandır
[right], Cengiz Yüce Kayabek, Bilge Kaan Tekelioğlu) report on
the diagnosis and treatment of a 3-year-old neutered female cavalier
King Charles spaniel diagnosed with mitral valve disease which began to
experience epileptic seizures. The epilepsy first was treated with
levetiracetam, which resulted in the epileptic seizures disappearing.
Then, three months later, the cavalier was treated for fleas and ticks
with fipronil (Frontline TopSpot, Fiproguard, Flevox, PetArmor). The
epileptic attacks "dramatically increased and became more severe just
after the fipronil treatment (~7 times per day)." Gabapentin was added
to the levetiracetam treatment protocol, and the epileptic seizures. The
researchers concluded:
In
an
October 2018 article, a team of Turkish veterinarians (Sinan Kandır
[right], Cengiz Yüce Kayabek, Bilge Kaan Tekelioğlu) report on
the diagnosis and treatment of a 3-year-old neutered female cavalier
King Charles spaniel diagnosed with mitral valve disease which began to
experience epileptic seizures. The epilepsy first was treated with
levetiracetam, which resulted in the epileptic seizures disappearing.
Then, three months later, the cavalier was treated for fleas and ticks
with fipronil (Frontline TopSpot, Fiproguard, Flevox, PetArmor). The
epileptic attacks "dramatically increased and became more severe just
after the fipronil treatment (~7 times per day)." Gabapentin was added
to the levetiracetam treatment protocol, and the epileptic seizures. The
researchers concluded:
"Fipronil, phenylpyrazole origin and other antiparasitic drugs should be used very carefully and under veterinary consultant supervision due to their side effects especially in epileptic dogs. Finally, gabapentin could be a good option for the alternative add-on therapy to control epileptic seizures in CKCSs."
February 2017: Purina launches a grain-laden dry food laced with epilepsy treatment supplements. In February 2017, Purina announced the launch in the USA of a dry dog food for canine epilepsy patients. The food reportedly is based upon a September 2015 study by veterinary neurologist Dr. Holger Volk, which we reported on in this October 2015 article.
EDITOR'S NOTE: Unfortunately, the ingredients* of this Purina product, as would be expected, are a typical grain-laden mess of dry food with a few supplements at the end, totally expected from Purina. We cannot imagine how any of these vitamins and other supplements are kept fresh when combined in a bag of triple-cooked kibble. A healthful canned food combining fresh meats and vegetables, topped off with appropriate supplements tailored to the particular disorder and sealed in capsules to maintain freshness, would be much, much better than this joke of a recipe.
*INGREDIENTS: Chicken, chicken meal, corn gluten meal, brewers rice, ground yellow corn, ground wheat, medium-chain triglyceride vegetable oil, corn germ meal, barley, natural flavor, fish oil, dried egg product, L-Arginine, wheat bran, fish meal, mono and dicalcium phosphate, potassium chloride, salt, calcium carbonate, L-Lysine monohydrochloride, Vitamin E supplement, choline chloride, L-ascorbyl-2-polyphosphate (Vitamin C), zinc sulfate, ferrous sulfate, niacin, manganese sulfate, Vitamin A supplement, thiamine mononitrate, soybean oil, calcium pantothenate, Vitamin B-12 supplement, copper sulfate, riboflavin supplement, pyridoxine hydrochloride, garlic oil, folic acid, menadione sodium bisulfite complex (Vitamin K), calcium iodate, biotin, Vitamin D-3 supplement, sodium selenite.
January 2017:
Phenobarbital and potassium bromide are effective supplements to
imepitoin treatment of idiopathic epilepsy.
 In
a
February 2017 article, Belgium researchers (Emile Royaux [right],
L. Van Ham, B.J.G. Broeckx, I. Van Soens, I. Gielen, D. Deforce, S.F.M.
Bhatti) tested adding phenobarbital or potassium bromide as additional
drugs for treatment with the new antiepileptic drug imepitoin. These
drugs were evaluated in 27 dogs by comparing monthly seizure frequency
(MSF), monthly seizure day frequency (MSDF), the presence of cluster
seizures during a retrospective 2-month period with a prospective
follow-up of 6 months, and the overall responder rate. They concluded
that when idiopathic epilepsy is not well controlled with maximum doses
of imepitoin alone, either phenobarbital or potassium bromide can be an
effective add-on drug which decreases median MSF and MSDF in epileptic
dogs unmanageable with a maximum dose of imepitoin. They stated that
combination therapy was generally well tolerated and resulted in an
improvement in seizure management in the majority of the dogs.
In
a
February 2017 article, Belgium researchers (Emile Royaux [right],
L. Van Ham, B.J.G. Broeckx, I. Van Soens, I. Gielen, D. Deforce, S.F.M.
Bhatti) tested adding phenobarbital or potassium bromide as additional
drugs for treatment with the new antiepileptic drug imepitoin. These
drugs were evaluated in 27 dogs by comparing monthly seizure frequency
(MSF), monthly seizure day frequency (MSDF), the presence of cluster
seizures during a retrospective 2-month period with a prospective
follow-up of 6 months, and the overall responder rate. They concluded
that when idiopathic epilepsy is not well controlled with maximum doses
of imepitoin alone, either phenobarbital or potassium bromide can be an
effective add-on drug which decreases median MSF and MSDF in epileptic
dogs unmanageable with a maximum dose of imepitoin. They stated that
combination therapy was generally well tolerated and resulted in an
improvement in seizure management in the majority of the dogs.
November 2016: UK and US researchers investigate links between epilepsy, drug-resistance, and affective disorders. A team of UK and US researchers (Rowena Mary Anne Packer, Holger Andreas Volk, Rachel A. Casey, Jan S. Suchodolski, Elizabeth J. Want) announced in October 2016 the start of a study investigating the interplay of extrinsic factors (environment, diet) and intrinsic factors (microbiome, metabolome) for the development of idiopathic epilepsy and affective disorders, such as anxiety, in dogs, and how these factors influence anti-epileptic drug responses.
July 2016:
Researchers find that six brands of pregabalin are "pharmaceutically
equivalent" for treating epilepsy.
 In a
May 2016 study of six brands of pregabalin, the Pakistani
researchers (Muhammad Arif Asghar, Syed Baqir Shayum Naqvi) found that
"all brands are pharmaceutically equivalent in their quality aspects."
They concluded that the lower cost brands of pregabalin could be
used to treat epilepsy.
In a
May 2016 study of six brands of pregabalin, the Pakistani
researchers (Muhammad Arif Asghar, Syed Baqir Shayum Naqvi) found that
"all brands are pharmaceutically equivalent in their quality aspects."
They concluded that the lower cost brands of pregabalin could be
used to treat epilepsy.
The rearchers do not identify the names of the six brands of pregabalin. They are coded as P-1 through P-6. However, one brand -- P-2 -- obviously is Pfizer's Lyrica because the authors point out its high cost, and they used P-2 as the standard to assess the similarity of different brands.
February 2016:
ACVIM issues a Consensus Statement on treating dogs for seizures.
 In a
February 2016 report, an international panel of veterinary
neurologists and other specialists (M. Podell [right], H.A. Volk, M. Berendt, W. Löscher,
K. Muñana, E.E. Patterson, S.R. Platt) published a "Consensus Statement" on
seizure management in dogs based on current literature and clinical
expertise, authorized by the American College of Veterinary Internal
Medicine (ACVIM). The report is divided into a series of questions much
like an FAQ format and focuses primarily upon drug treatments and also
touches upon alternative care methods.
In a
February 2016 report, an international panel of veterinary
neurologists and other specialists (M. Podell [right], H.A. Volk, M. Berendt, W. Löscher,
K. Muñana, E.E. Patterson, S.R. Platt) published a "Consensus Statement" on
seizure management in dogs based on current literature and clinical
expertise, authorized by the American College of Veterinary Internal
Medicine (ACVIM). The report is divided into a series of questions much
like an FAQ format and focuses primarily upon drug treatments and also
touches upon alternative care methods.
Their first question is "When Should Treatment Be Started?" They conclude:
"The panel recommendations to initiate AED [antiepileptic drugs] treatment are summarized as follows: (i) Identifiable structural lesion present or prior history of brain disease or injury; (ii) Acute repetitive seizures or, status epilepticus (ictal event ≥5 minutes or ≥3 or more generalized seizures within a 24-hour period); (iii) ≥2 or more seizure events within a 6-month period; and (iv) Prolonged, severe, or unusual postictal periods."
Then they pose this question and analyze in
detail five specific drugs: "Which Drug Should Be Used First?" Their
list:
• Phenobarbital: High recommendation and likely be effective
treatment.
• Potassium Bromide: Moderate recommendation and most likely
to be effective treatment.
• Primidone: Not recommended for treatment
and may be ineffective and/or dangerous to the patient.
• Imepitoin:
High recommendation and likely be effective treatment.
• Levetiracetam:
Low recommendation and may not be effective treatment.
• Zonisamide:
Low recommendation and may not be effective treatment.
They fail to mention the anti-convulsants such as gabapentin or pregabalin or the sedative acepromazine maleate, presumably because of a lack of much published evidentiary research on these treatments.
They next discuss: "How Should Monitoring Be Performed?" and "What Are The Risks Of Treatment?" and "When Should a Second AED Be Started and Which Should be Used?", Then they turn their attention to "What Alternative Nonpharmacologic Treatments Are Available?" They list four categories of alternative treatments: Vagal nerve stimulation (VNS), dietary alteration treatment, acupuncture, and homeopathy, thereby ignoring other holistic remedies such as Chinese and Western herbal therapy, nutrition, veterinary chiropractic, and homotoxicology.
January 2016:
UK study of epileptic dogs also finds attention-deficit/hyperactivity
disorder (ADHD) behaviors, and that a ketogenic medium chain
triglyceride diet (MCTD) improved the ADHD activities.
 In a
February 2016 report, a team of UK researchers (Rowena M.A. Packer, Tsz
Hong Law, Emma Davies, Brian Zanghi, Yuanlong Pan [right], Holger A. Volk)
studied 21 dogs affected with idiopathic epilepsy (IE), feeding them a
ketogenic medium chain triglyceride diet (MCTD) for three months and
then a placebo diet for three months. They were looking for
attention-deficit/hyperactivity disorder (ADHD) behaviors in the dogs --
excitability, chasing, and trainability. They found that their "data
support the supposition that dogs with IE may exhibit behaviors that
resemble ADHD symptoms seen in humans and rodent models of epilepsy and
that a MCTD may be able to improve some of these behaviors, along with
potentially anxiolytic effects."
In a
February 2016 report, a team of UK researchers (Rowena M.A. Packer, Tsz
Hong Law, Emma Davies, Brian Zanghi, Yuanlong Pan [right], Holger A. Volk)
studied 21 dogs affected with idiopathic epilepsy (IE), feeding them a
ketogenic medium chain triglyceride diet (MCTD) for three months and
then a placebo diet for three months. They were looking for
attention-deficit/hyperactivity disorder (ADHD) behaviors in the dogs --
excitability, chasing, and trainability. They found that their "data
support the supposition that dogs with IE may exhibit behaviors that
resemble ADHD symptoms seen in humans and rodent models of epilepsy and
that a MCTD may be able to improve some of these behaviors, along with
potentially anxiolytic effects."
 December 2015:
Danish research concludes levetiracetam was not effective as
mono-therapy for idiopathic epilepsy. In a
November 2015 article, a team of Danish researchers (Nadia Fredsø
[Andersen] [right], A.
Sabers, N. Toft, A. Møller, M. Berendt) treated six of twelve affected
dogs solely with levetiracetam and treated the other six solely
with phenobarbital. The researchers found that, in the levetiracetam
treated dogs, there was "no significant difference" in the monthly number
of seizures before and after treatment, whereas in the phenobarbital
treated dogs, there were "significantly fewer seizures after treatment".
They concluded that: "In this study levetiracetam was well tolerated but
was not effective at the given doses as mono-therapy in dogs with
idiopathic epilepsy."
December 2015:
Danish research concludes levetiracetam was not effective as
mono-therapy for idiopathic epilepsy. In a
November 2015 article, a team of Danish researchers (Nadia Fredsø
[Andersen] [right], A.
Sabers, N. Toft, A. Møller, M. Berendt) treated six of twelve affected
dogs solely with levetiracetam and treated the other six solely
with phenobarbital. The researchers found that, in the levetiracetam
treated dogs, there was "no significant difference" in the monthly number
of seizures before and after treatment, whereas in the phenobarbital
treated dogs, there were "significantly fewer seizures after treatment".
They concluded that: "In this study levetiracetam was well tolerated but
was not effective at the given doses as mono-therapy in dogs with
idiopathic epilepsy."
October 2015:
UK researchers find anti-epileptic properties in
ketogenic diets reduce seizure frequencies in epileptic dogs.
 In a
September 2015 article by a team of UK researchers (Tsz Hong Law,
Emma S. S. Davies, Yuanlong Pan, Brian Zanghi, Elizabeth Want,
Holger A. Volk [right]), they fed 21 dogs suspected to have idiopathic epilepsy,
including a cavalier King Charles spaniel (CKCS), a dry food kibble
which was either a ketogenic medium-chain TAG (triacylglycerol) diet
(MCTD) or a placebo diet, for three months. Then the dogs were switched
from the one diet to the other for another three months. The results
overall showed that seizure frequencies were "significantly lower when
dogs were fed the MCTD in comparison with the placebo diet. The CKCS's
seizure frequency was reduced from 10 per month on the placebo diet to 5
per month while on the MCTD. The researchers concluded:
In a
September 2015 article by a team of UK researchers (Tsz Hong Law,
Emma S. S. Davies, Yuanlong Pan, Brian Zanghi, Elizabeth Want,
Holger A. Volk [right]), they fed 21 dogs suspected to have idiopathic epilepsy,
including a cavalier King Charles spaniel (CKCS), a dry food kibble
which was either a ketogenic medium-chain TAG (triacylglycerol) diet
(MCTD) or a placebo diet, for three months. Then the dogs were switched
from the one diet to the other for another three months. The results
overall showed that seizure frequencies were "significantly lower when
dogs were fed the MCTD in comparison with the placebo diet. The CKCS's
seizure frequency was reduced from 10 per month on the placebo diet to 5
per month while on the MCTD. The researchers concluded:
"In conclusion, the data show antiepileptic properties associated with ketogenic diets and provide evidence for the efficacy of the MCTD used in this study as a therapeutic option for epilepsy treatment."
September 2015:
International Veterinary Epilepsy Task Force issues a
consensus proposal on diagnosing idiopathic epilepsy.
 In a
September
2015 article, the International Veterinary Epilepsy Task Force,
consisting of neurologists and other veterinary specialists from the US,
UK, and throughout Europe (Velia-Isabel Hülsmeyer, Andrea Fischer, Paul
J.J. Mandigers, Luisa DeRisio, Mette Berendt, Clare Rusbridge, Sofie
F.M. Bhatti, Akos Pakozdy, Edward E. Patterson, Simon Platt, Rowena M.A.
Packer, Holger A. Volk) issues their consensus proposal on diagnosing
epilepsy in dogs. They outline "two fundamental steps: to establish if
the events the animal is demonstrating truly represent epileptic
seizures and if so, to identify their underlying cause." They then
describe a three-tier system for the diagnosis of idiopathic epilepsy
(IE):
In a
September
2015 article, the International Veterinary Epilepsy Task Force,
consisting of neurologists and other veterinary specialists from the US,
UK, and throughout Europe (Velia-Isabel Hülsmeyer, Andrea Fischer, Paul
J.J. Mandigers, Luisa DeRisio, Mette Berendt, Clare Rusbridge, Sofie
F.M. Bhatti, Akos Pakozdy, Edward E. Patterson, Simon Platt, Rowena M.A.
Packer, Holger A. Volk) issues their consensus proposal on diagnosing
epilepsy in dogs. They outline "two fundamental steps: to establish if
the events the animal is demonstrating truly represent epileptic
seizures and if so, to identify their underlying cause." They then
describe a three-tier system for the diagnosis of idiopathic epilepsy
(IE):
"Tier I confidence level for the diagnosis of IE is based on a history of two or more unprovoked epileptic seizures occurring at least 24 h apart, age at epileptic seizure onset of between six months and six years, unremarkable inter-ictal physical and neurological examination, and no significant abnormalities on minimum data base blood tests and urinalysis.
Tier II confidence level for the diagnosis of IE is based on the factors listed in tier I and unremarkable fasting and post-prandial bile acids, magnetic resonance imaging (MRI) of the brain (based on an epilepsy-specific brain MRI protocol) and cerebrospinal fluid (CSF) analysis.
Tier III confidence level for the diagnosis of IE is based on the factors listed in tier I and II and identification of electroencephalographic abnormalities characteristic for seizure disorders. The authors recommend performing MRI of the brain and routine CSF analysis, after exclusion of reactive seizures, in dogs with age at epileptic seizure onset <6 months or >6 years, inter-ictal neurological abnormalities consistent with intracranial neurolocalisation, status epilepticus or cluster seizure at epileptic seizure onset, or a previous presumptive diagnosis of IE and drug-resistance with a single antiepileptic drug titrated to the highest tolerable dose. This consensus article represents the basis for a more standardised diagnostic approach to the seizure patient. These recommendations will evolve over time with advances in neuroimaging, electroencephalography, and molecular genetics of canine epilepsy."
September 2015: International Veterinary Epilepsy Task Force reports on epilepsy in cavaliers. In a September 2015 article, the International Veterinary Epilepsy Task Force, consisting of neurologists and other veterinary specialists from the US, UK, and throughout Europe (Velia-Isabel Hülsmeyer, Andrea Fischer, Paul J.J. Mandigers, Luisa DeRisio, Mette Berendt, Clare Rusbridge, Sofie F.M. Bhatti, Akos Pakozdy, Edward E. Patterson, Simon Platt, Rowena M.A. Packer, Holger A. Volk) issues their massive "current understanding of idiopathic epilepsy of genetic or suspected genetic origin in purebred dogs", including, of course, the cavalier King Charles spaniel. Their primary findings regarding the CKCS:
• Idiopathic epilepsy may occur independently of Chiari-like malformation (CM), but an overlapping of the two diseases cannot be excluded.
• Epilepsy was found more frequently in lines originating from whole-color dogs.
• No detailed data regarding potential modes of inheritance are available.
• Potential breed-specific diseases that may mimic idiopathic epilepsy: episodic falling ("In contrast to epileptic seizures, consciousness usually is not affected during these episodes."); myoclonus [spasmodic jerky contraction of groups of muscles] ("Older Cavalier King Charles spaniels (>5 years old) have a high prevalence of myoclonus, which manifests most commonly as a brief jerking of the head and forelimbs when the dog is standing or sitting. Initially the syndrome is relatively benign but can be progressive with affected dogs suffering frequent jerks which may interfere with function, for example cause the dog to fall or stumble. The syndrome can be confused with focal epileptic seizures but generally does not respond to AEDs [antiepileptic drugs] licenced for dogs although may respond to levetiracetam.")
February 2015: NC State researchers find adding phenobarbital and bromide increases Levetiracetam's movement through epileptic dogs. In a February 2015 study, a team of researchers at North Carolina State University report that the concurrent administration of phenobarbital alone or with bromide increased the clearance of Levetiracetam in epileptic dogs. See, also, this team's July 2014 report on the same topic.
February 2015: UK's Royal Veterinary College's research team finds levetiracetam to effectively reduce seizures. In a February 2015 report by UK's Royal Veterinary College's canine epilepsy research team, it found that in a study of 52 affected dogs, the epilepsy drug levetiracetam was effective and well-tolerated for reducing seizures -- 69% of the dogs had a 50% or greater reduction in seizure frequency while 15% of all the dogs were completely free from seizures.
January 2015:
UK's Royal Veterinary College's new Epilepsy & Stress study needs
affected dogs. The Royal Veterinary College's Canine
Epilepsy Research team (Rowena Packer, Holger Volk, and Rob Fowkes) is
seeking saliva samples from dogs affected with idiopathy epilepsy and
information from their owners about the dogs' quality of life, including
their seizure frequency, type, severity, and how well their seizures are
controlled by medication. They assure that all information will be kept
secure and anonymous. No visit to RVC will be necessary, as all samples
and data will be collected remotely.
If you live in the UK and
have an eligible dog (must not be affected by any known endocrine
disorder, such as Cushing's, hypothyroidism or hyperthyroidism and not
taking any steroids), contact Dr. Packer at rpacker@rvc.ac.uk with this
information: (a) name, age, breed, sex, and neuter status of the dog;
(b) whether you and your dog meet the inclusion criteria; (c) how often
your dog has seizures per month; and (d) where in the UK you are
located.
October 2014:
UK researchers find oral phenobarbital, imepitoin, potassium bromide,
and levetiracetam likely are effective to treat idiopathic epilepsy,
with a big BUT . UK researchers Marios Charalambous, David
Brodbelt, and Holger A. Volk (right) examined various antiepileptic drugs (AEDs)
used for the management of canine idiopathic epilepsy (IE). In
an
October 2014 report, they found evidence to support the efficacy of oral
phenobarbital and imepitoin and a "fair level of evidence" to support
the efficacy of oral potassium bromide and levetiracetam. However, for the remaining AEDs (zonisamide, primidone, gabapentin, pregabalin,
sodium valproate, felbamate, and topiramate), they found "insufficient
evidence to support their use due to lack of bRCTs [blinded randomized
clinical trials]". They concluded that "there is a need for greater
numbers of adequately sized bRCTs evaluating the efficacy of AEDs for
IE."
. UK researchers Marios Charalambous, David
Brodbelt, and Holger A. Volk (right) examined various antiepileptic drugs (AEDs)
used for the management of canine idiopathic epilepsy (IE). In
an
October 2014 report, they found evidence to support the efficacy of oral
phenobarbital and imepitoin and a "fair level of evidence" to support
the efficacy of oral potassium bromide and levetiracetam. However, for the remaining AEDs (zonisamide, primidone, gabapentin, pregabalin,
sodium valproate, felbamate, and topiramate), they found "insufficient
evidence to support their use due to lack of bRCTs [blinded randomized
clinical trials]". They concluded that "there is a need for greater
numbers of adequately sized bRCTs evaluating the efficacy of AEDs for
IE."
April 2014: Epileptic CKCS has leg twitching and loss of muscle control reactions to potassium bromide treatment. In an April 2014 report, a spayed female cavalier diagnosed with idiopathic epilepsy was treated with potassium bromide and phenobarbital. Eight days later, the veterinarians found her suffering from a lack of muscle control and repetitive twitching of the limbs. They concluded she was overdosed with the bromide solution. She had no similar episodes following a reduction in the dosing.
May 2013: UK's Royal Veterinary College needs dogs with idiopathic epilepsy for study. The Royal Veterinary College of the University of London still is seeking dogs suspected of suffering idiopathic epilepsy for a study of the influence of a diet on improving seizure control. Details are available here. See our June 2012 item below for more information.
July 2012: UK researchers find no connection between Chiari-like malformation and epilepsy in cavaliers. In a 2012 report in the Veterinary Journal, UK neurology researchers C.J. Driver, K. Chandler, G. Walmsley, N. Shihab, and H.A. Volk examined the MRIs of 85 cavalier King Charles spaniels, looking for a relationship between Chiari-like malformation (CM), ventriculomegaly, and seizures in the dogs. The 85 CKCSs all had CM; 27 of them also had had seizures. They found no association between CM, ventriculomegaly, and the seizures. The seizures were classified as having partial onset -- meaning that they occur in in one area of the brain, unlike generalized seizures which typically affect nerve cells throughout the brain -- in 61% of the dogs. They also stated that "Another cause of recurrent seizures in CKCS (such as familial epilepsy) is suspected, as previously reported."
 June
2012:
Royal Veterinary College (RVC) conducts study of the influence of
diet on improving seizure control. The RVC is working with a small
animal health and wellness company to confirm the efficacy and safety of a novel
diet in the management of dogs with idiopathic epilepsy being treated with
phenobarbitone and/or potassium bromide. To confirm the efficacy of this new
diet, RVC seeks to recruit dogs which are suspected of having idiopathic
epilepsy, with these qualifications: (a) dogs which have a seizure frequency of
at least three seizures in the last three months; and (b) dogs receiving
phenobarbitone and/or potassium bromide treatment. For more information, contact
RVC by
clicking here, and/or
downloading this brochure.
June
2012:
Royal Veterinary College (RVC) conducts study of the influence of
diet on improving seizure control. The RVC is working with a small
animal health and wellness company to confirm the efficacy and safety of a novel
diet in the management of dogs with idiopathic epilepsy being treated with
phenobarbitone and/or potassium bromide. To confirm the efficacy of this new
diet, RVC seeks to recruit dogs which are suspected of having idiopathic
epilepsy, with these qualifications: (a) dogs which have a seizure frequency of
at least three seizures in the last three months; and (b) dogs receiving
phenobarbitone and/or potassium bromide treatment. For more information, contact
RVC by
clicking here, and/or
downloading this brochure.
March 2012: Intravenous levetiracetam is reported to be safe and potentially effective for treatment of epileptic dogs. University of Minnesota veterinary researchers report in a March 2012 article that intravenous levetiracetam. in addition to IV diazepam treatment, showed a trend toward superiority over placebo and IV diazepam for the treatment of epilepsy and acute repetitive seizures in dogs.
December 2009: Pregabalin (Lyrica) is being studied to treat epileptic dogs. In a December 2009 study, an international panel of neurologists (Curtis W. Dewey, Sofia Cerda-Gonzalez, Jonathan M. Levine, Britton L. Badgley, Julie M. Ducoté, Gena M. Silver, Jocelyn J. Cooper, Rebecca A. Packer, James A. Lavely) report that 78% of dogs respond to pregabalin (Lyrica) and that there was a 57% mean reduction in seizures for the participants who finished the study; all had been diagnosed with difficult-to-control seizures.
May 2007: Levetiracetam, potassium bromide, and phenobarbital finally controls recurrent and cluster seizures in a cavalier. In a May 2007 article, North Carolina State University clinicians reported on a 6-month-old cavalier King Charles spaniel which had seizures over the period of a year, which were difficult to control with standard anti-convulsants. They diagnosed anorganic aciduria with excessive excretion of hexanoylglycine when the dog was 20 months old. Recurrent and cluster seizures were eventually controlled with the addition of levetiracetam to potassium bromide and phenobarbital.
October 2004: New anti-epileptic drug ELB138. Profs. Chris Rundfeldt, Andrea Tipold, Wolfgang Loscher, and others, of the Department of Small Animal Medicine and Surgery, University of Veterinary Medicine, and Center for Systems Neuroscience, Hannover, Germany, have researched, developed, and have been studying the efficacy of a new antiepileptic and anxiolytic drug, ELB138 [later named imepitoin], which is a low-affinity partial BZD-receptor agonist, formerly called AWD 131-138; 1-(4-chlorophenyl)-4-morpholino-imidazolin-2-one. They and others hold a U.S.patent (20050070537) for this drug. They report in their October 2004 veterinary journal article that "the reduction in seizure frequency using ELB138 in dogs with newly diagnosed idiopathic epilepsy was comparable to the reduction in dogs treated either with phenobarbital or primidone. In dogs with chronic epilepsy and add-on therapy with either ELB138 or potassium bromide, such supplementation reduced the seizure frequency and the duration and severity of seizures" with reportedly rare side effects. (ELB138 has since been re-named imepitoin.)
June 2004: Clare Rusbridge finds epilepsy is inheritable in CKCSs, especially whole-colors. UK's Clare Rusbridge reports that idiopathic epilepsy is an inheritable disease in the cavalier King Charles spaniel and is seen imore frequently in lines originating from whole-colored ancestors from the late 1960s, especially where there were half-brother/sister matings.
RETURN TO TOP
Related Links
RETURN TO TOP
Veterinary Resources
Clinical Effects of Longitudinal Division of the Corpus Callosum in Normal Dogs. Rodney S. Bagley, Timothy V. Baszler, Michael L. Harrington, G. Elizabeth Pluhar, Michael P. Moore, Robert D. Keegan, Stephen A. Greene. Vet. Surg. March 1995; doi: 10.1111/j.1532-950X.1995.tb01306.x. Quote: Longitudinal division of the corpus callosum was performed in six normal beagles to determine surgical morbidity. The corpus callosum was divided sagittally on the midline and the effect on neurological function was determined. Five of six dogs were clinically normal within 14 days or less after surgery. One dog had persistent but improving clinical signs consistent with a forebrain disturbance at 30 days after surgery. Overall, minimal morbidity and no mortality was associated with this surgical procedure. Further study is indicated to determine the efficacy of this surgical treatment for seizure control in dogs with idiopathic epilepsy.
Extramedullary Hematopoiesis in the Choroid Plexus of Five Dogs. D. Bienzle, J. M. Kwiecien, J. M. Parent. Vet.Pathol. July 1995; doi:10.1177/030098589503200417 . Quote: Five dogs euthanatized because of refractory seizures were found to have hematopoietic elements in the interstitium of the choroid plexus at the level of the fourth ventricle. None of the dogs had significant hematologic or cerebrospinal fluid abnormalities. Dog No. 4 was a 3-year-old male Cavalier King Charles Spaniel with seizures since the age of 7 months. Five months of phenobarbital therapy had not affected the clinical status, and addition of KBr and dexamethasone yielded no improvement. Relevant laboratory findings consisted of mild hyperglycemia and a mild leukocytosis due to a mature neutrophilia (Table 1). CSF analysis disclosed blood contamination and several small clumps of meningeal cells (Table 2). Based on clinical examination and magnetic resonance imaging, a diagnosis of genetic epilepsy was established, and euthanasia was elected. Dog No. 4 had swollen, vacuolated hepatocytes attributed to recent glucocorticoid and barbiturate therapy and a cystic craniopharyngeal duct considered an incidental finding. Individual small foci of gliosis were present throughout the white matter of the frontal cortex, the internal capsule, and the substantia nigra. The temporal cortex had several ectopic islands of gray matter. Immature myelocytic cells, ranging from myeloblasts to band neutrophils, and scattered rubricytes were present in the stroma of the choroid plexus of the fourth ventricle. The xtramedullary hematopoiesis was confined to the central nervous system and consisted of megakaryocytes, immature granulocytes, and rubricytes in two dogs and of one predominant cell population in each of the other three dogs. These findings are unique, and factors possibly contributing to the formation of a hematopoietic inductive microenvironment in the choroid plexus are cytokine neurokine homologies, locally altered vascular supply, and aberrant functioning of bone marrow-derived central nervous system macrophages.
Control of Canine Genetic Diseases. Padgett, G.A., Howell Book House 1998, pp. 198-199, 235.
A Simple,
Effective Technique for Arresting Canine Epileptic Seizures. H. C.
Gurney, Janice Gurney. J. Amer. Holistic Vet.
Med. Assn. Jan 2004; 22(4):17-18.
Quote: "Fifty-one epileptic canine patients were successfully treated during an
epileptic
 seizure with a technique involving the application of ice on the back
(T10 to L4). This technique was found to be effective in aborting or shortening
the duration of ictus. ... Ice is applied as soon as the seizure is observed. The application itself
is either a block of ice (i.e., water frozen in a metal ice tray, with the tray
applied directly to the seizing patient), or ice (cubes or crushed ice in a
plastic bag). The ice is held firmly to the dog’s back, on the area superior to
the spinal process from T10 (palpable at the 'low spot' on the canine spine) to
L4 (Figure at right). The size of a given ice application is sufficient to cover the
described area. Maintain firm pressure in that location until the patient
spontaneously recovers sternal recumbency and makes efforts to rise and walk. If
the patient is prone to 'chain' episodes or displays evidence of returning to
ictus after removal of the ice, the ice should once again be applied until the
patient regains sternal recumbence (when chain seizures occur, aggressive
medical intervention is necessary). Clients have used bags or boxes of frozen
vegetables, but such applications are reported to be less effective.
... The sooner ice was applied during an epileptic event, the more effective the
intervention was in stopping or abbreviating the seizure. Also of note was the
observation that the canines’ post-ictus recovery time was shorter, and recovery
appeared to be augmented."
seizure with a technique involving the application of ice on the back
(T10 to L4). This technique was found to be effective in aborting or shortening
the duration of ictus. ... Ice is applied as soon as the seizure is observed. The application itself
is either a block of ice (i.e., water frozen in a metal ice tray, with the tray
applied directly to the seizing patient), or ice (cubes or crushed ice in a
plastic bag). The ice is held firmly to the dog’s back, on the area superior to
the spinal process from T10 (palpable at the 'low spot' on the canine spine) to
L4 (Figure at right). The size of a given ice application is sufficient to cover the
described area. Maintain firm pressure in that location until the patient
spontaneously recovers sternal recumbency and makes efforts to rise and walk. If
the patient is prone to 'chain' episodes or displays evidence of returning to
ictus after removal of the ice, the ice should once again be applied until the
patient regains sternal recumbence (when chain seizures occur, aggressive
medical intervention is necessary). Clients have used bags or boxes of frozen
vegetables, but such applications are reported to be less effective.
... The sooner ice was applied during an epileptic event, the more effective the
intervention was in stopping or abbreviating the seizure. Also of note was the
observation that the canines’ post-ictus recovery time was shorter, and recovery
appeared to be augmented."
Inheritance of occipital bone hypoplasia (Chiari type I malformation) in Cavalier King Charles spaniels. Rusbridge C., Knowler S. P. J Vet Intern Med 2004;18:673–678. Quote: "Occipital bone hypoplasia with foramen magnum obstruction and secondary syringomyelia (SM) is a common condition in the Cavalier King Charles Spaniel (CKCS) that is similar to human Chiari type I malformation. A worldwide family tree of more than 5,500 CKCSs spanning a maximum of 24 generations was established by obtaining pedigree information from 120 dogs diagnosed with SM secondary to occipital bone hypoplasia. The ongoing study showed 6 of 8 great grandparents of all affected dogs could be traced back to 2 female ancestors so that all 8 were descended from one or the other or both. The disease appears to be more severe and have an earlier onset with increased inbreeding, especially when breeding from affected dogs. The family tree of idiopathic epilepsy (IE) appears to be a different subset of the CKCS population, although some overlap was observed. Idiopathic epilepsy is more frequent in lines originating from whole-color dogs. Selection for coat color is believed to have influenced the development of both occipital hypoplasia with secondary SM and IE. In addition, breeding guidelines to reduce the incidence of mitral valve disease have placed further pressures on the gene pool."
Seizures (Podell, M.) in: Manual of Small Animal Neurology, 3d ed. Editors Olby N., Platt S., British Small Animal Vety Assn (2004). pp 97-112.
Alternative anticonvulsant drugs for dogs with seizure disorders. Curtis W. Dewey, Georgina Barone, Kerry Smith, Gregg D. Kortz. DVM360.com. Sept. 2004.
Anticonvulsant efficacy of the low-affinity partial benzodiazepine receptor agonist ELB 138 in a dog seizure model and in epileptic dogs with spontaneously recurrent seizures. Loscher W, Potschka H, Rieck S, Tipold A, Rundfeldt C. Epilepsia. 2004 Oct;45(10):1228-39. Quote: "Results: ELB 138 was shown to increase potently the pentylenetetrazole (PTZ) seizure threshold in dogs. Prolonged oral administration with twice-daily dosing of ELB 138 with either 5 or 40 mg/kg over a 5-week period was not associated with loss of anticonvulsant efficacy in the PTZ dog model. To study whether physical dependence developed during long-term treatment, the BZD antagonist flumazenil was injected after 5 weeks of treatment with ELB 138. Compared with prolonged treatment with DZP, only relatively mild abstinence symptoms were precipitated in dogs treated with ELB 138, particularly at the lower dosage (5 mg/kg, b.i.d.). In a prospective trial in dogs with newly diagnosed epilepsy, ELB 138 markedly reduced seizure frequency and severity without significant difference to standard treatments (phenobarbital or primidone) but was much better tolerated than the standard drugs. In dogs with chronic epilepsy, most dogs exhibited a reduction in seizure frequency and severity during add-on treatment with ELB 138. Conclusions: The data demonstrate that the partial BZD receptor agonist ELB 138 exerts significant anticonvulsant efficacy without tolerance in a dog seizure model as well as in epileptic dogs with spontaneously recurrent seizures. These data thus substantiate that partial agonism at the BZD site of GABAA receptors offers advantages versus full agonism and constitutes a valuable approach for treatment of seizures."
Neurological diseases of the Cavalier King Charles spaniel. Rusbridge, C. J Small Animal Practice, June 2005, 46(6): 265-272(8). "Idiopathic epilepsy is a inheritable disease in the CKCS and is seen in all colour varieties but is more frequent in lines originating from whole-coloured ancestors from the late 1960s, especially where there were half-brother/sister matings (Rusbridge and Knowler 2004). Diagnosis is by ruling out other causes of seizures; for example, using haematology and biochemistry to rule out reactive causes such as hepatic encephalopathy, and MRI and CSF analysis to rule out structural and inflammatory disease such as GME. The author’s firstline therapy is phenobarbital or bromide monotherapy, progressing to a combination of both drugs if the seizures are not adequately controlled. Some cases of CKCS epilepsy are difficult to control and novel anticonvulsants such as levetiracetam (Keppra; UCB Pharma) or topiramate (Topamax; Janssen-Cilag) may be useful. For a more extensive review of the management of epilepsy see Podell (2004)."
Anticonvulsant activity and tolerance of ELB138 in dogs with epilepsy: A clinical pilot study. Rieck S, Rundfeldt C, Tipold A. Vet J. 2005 May 16.
From Gold Beads to Keppra: Update on Anticonvulsant Therapy. Gregg Kortz. 2d Ann. Vet. Neurology Symposium. Univ. Calif.-Davis. 2005.
Improving seizure control in dogs with refractory epilepsy using gabapentin as an adjunctive agent. M. Govendir, M. Perkins, R. Malik. Australian Vet. October 2005;83(10):602-608. Quote: "Objective: To assess whether there is a change in seizure activity in dogs with refractory epilepsy that are receiving appropriate doses of phenobarbitone and/or potassium bromide, when gabapentin is added to the therapeutic regimen. Design: A prospective study of 17 dogs with a refractory seizure disorder, 16 of which have idiopathic epilepsy. Procedure: Patients were stabilised using phenobarbitone and/or potassium bromide to produce tolerable therapeutic serum concentrations and dosed additionally with gabapentin at 35 to 50 mg/kg/d (divided twice or three times daily) for 4 months. Owners recorded seizure activity and side effects during this period in a standardised diary. Patients underwent monthly physical examinations and venepuncture to assess selected serum biochemical analytes, as well as phenobarbitone and bromide concentrations. Patients were further monitored for long-term response to adjunctive gabapentin therapy. Results: There was no significant decrease in the number of seizures over the studyperiod for the entire cohort, however three dogs stopped seizuring completely. There was a significant increase in the number of patients who showed an increase in the interictal period (P > 0.001). Serum alkaline phosphatase activity and triglyceride concentrations were elevated at baseline. There were no significant changes in biochemical analytes during the course of the study period. Side effects observed initially on addition of gabapentin included sedation and hind limb ataxia. The former resolved spontaneously after a few days; the latter after a slight reduction in bromide dose. Long-term, a further two patients became seizure free and ten patients remained on gabapentin indefinitely. No long-term side effects have become apparent. Conclusion: Addition of gabapentin to phenobarbitone and/or potassium bromide increased the interictal period and shortened the post-seizure recovery in some canine epileptics. In some dogs, seizures were prevented completely, while in others there was an increase in interictal period. The short-half life of gabapentin has advantages for seizure control, however its present high cost may prohibit therapy in large dogs."
A Retrospective Study on the Use of Acepromazine Maleate in Dogs With Seizures. Karen M. Tobias, Katia Marioni-Henry, and Rebecca Wagner. J. Am.An. Hosp. Assn. July 2006; 42:283-289; doi:10.5326/0420283 . Quote: Use of acepromazine (i.e., acetylpromazine) maleate in dogs with a history of seizures is reportedly contraindicated because of the risk of decreasing the seizure threshold in these animals. In this retrospective study, acepromazine was administered for tranquilization to 36 dogs with a prior history of seizures and to decrease seizure activity in 11 dogs. No seizures were seen within 16 hours of acepromazine administration in the 36 dogs that received the drug for tranquilization during hospitalization. After acepromazine administration, seizures abated for 1.5 to 8 hours (n=6) or did not recur (n=2) in eight of 10 dogs that were actively seizing. Excitement-induced seizure frequency was reduced for 2 months in one dog.
Treatment with gabapentin of 11 dogs with refractory idiopathic epilepsy. Platt, S. R.; Adams, V.; Garosi, L. S.; Abramson, C. J.; Penderis, J.; De Stefani, A.; Matiasek, L. Vet.Rec. December 2006;159(26):881-884. Quote: "Eleven dogs diagnosed with refractory idiopathic epilepsy were treated orally with gabapentin for a minimum of three months at an initial dose of 10 mg/kg every eight hours. They were all experiencing episodes of generalised tonic-clonic seizures and had been treated chronically with a combination of phenobarbital and potassium bromide at doses sufficient to reach acceptable therapeutic serum levels without causing significant side effects. In each dog, the number of seizures per week, the average duration of the seizures and the number of days on which seizures occurred were compared for the three months before and after they were treated with gabapentin. A minimum 50 per cent reduction in the number of seizures per week was interpreted as a positive response to gabapentin, and six of the dogs showed a positive response. After the addition of gabapentin, both the number of seizures per week (P = 0.005) and the number of days with any seizures in a one-week period (P = 0.03) were significantly reduced. Mild side effects of ataxia and sedation were observed in five of the dogs, but they were not severe enough to warrant the treatment being discontinued during the trial."
Clinical management of idiopathic epilepsy in dogs with homeopathic Belladonna 200C: a case series. JP Varshney. Homeopathy. January 2007;96:46-48. Quote: Epilepsy is an important neurological disorder in dogs. Belladonna 200C was evaluated in 10 dogs with idiopathic epilepsy. During the seizure phase, 3–4 drops of Belladonna 200C were administered orally at 15 min intervals until considerable reduction in seizure activity, then four times daily. Four dogs with head shaking syndrome in addition to seizures were given Cocculus 6C, 3–4 drops orally weekly for 3 months in addition. Numbers of fits reduced to 2–3 during first 2 weeks post-therapy and then became occasional in next 2 weeks. With continuation of Belladonna therapy, no fits were observed during 2–7 months follow-up. In two cases epileptic fits reappeared within 15–25 days of cessation of therapy. Belladonna therapy was resumed and seizure control was again achieved. Owners were advised to continue the therapy at least twice daily until there were no fits for 2–3 months. Liver specific enzymes were monitored, no abnormalities were observed.
Refractory seizures associated with an organic aciduria in a dog. Simon Platt, Yvonne L. McGrotty, Carley J. Abramson, Cornelis Jakobs. J Am Anim Hosp Assoc. May 2007; doi: 10.5326/0430163. Quote: A 6-month-old, female Cavalier King Charles spaniel exhibited seizures that were difficult to control with standard anticonvulsants over a 12-month period. The diagnosis of an organic aciduria with excessive excretion of hexanoylglycine was determined when the dog was 20 months old. Recurrent and cluster seizures were eventually controlled with the addition of levetiracetam to potassium bromide and phenobarbital.
Epil-K9's Canine Epilepsy Resources website.
The efficacy and tolerability of Levetiracetam in pharmacoresistant epileptic dogs. Holger A. Volk, Lara A. Matiasek, Alejandro Luján Feliu-Pascual, Simon R. Platt, Kate E. Chandler. Vet. J. June 2008;176(3):310-319. Quote: "Twenty-two dogs with idiopathic epilepsy which were pharmacoresistant to phenobarbitone and bromide were treated with levetiracetam as an add-on medication. Records of eight dogs were used retrospectively to determine a safe, efficient levetiracetam dosage. Fourteen dogs were entered into a prospective, open label, non-comparative study. After 2 months of levetiracetam oral treatment (10 mg/kg TID), 8/14 dogs responded significantly to the treatment and seizure frequency was reduced by ⩾50%. In dogs that remained refractory, the dosage was increased to 20 mg/kg TID for 2 months. One further dog responded to levetiracetam treatment. Levetiracetam responders had a significant decrease in seizure frequency of 77% (7.9 ± 5.2 to 1.8 ± 1.7 seizures/month) and a decrease in seizure days per month of 68% (3.8 ± 1.7 to 1.2 ± 1.1 seizure days/month). However, 6/9 responders experienced an increase in seizure frequency and seizure days after 4–8 months continuing with the levetiracetam treatment at the last effective dosage. Levetiracetam was well tolerated by all dogs and sedation was the only side-effect reported in just one of the 14 dogs."
Pregabalin as an adjunct to phenobarbital, potassium bromide, or a combination of phenobarbital and potassium bromide for treatment of dogs with suspected idiopathic epilepsy. Curtis W. Dewey, Sofia Cerda-Gonzalez, Jonathan M. Levine, Britton L. Badgley, Julie M. Ducoté, Gena M. Silver, Jocelyn J. Cooper, Rebecca A. Packer, and James A. Lavely. JAVMA, Dec 2009; 235(12):1442-1449, Quote: "Objective—To assess tolerability and short-term efficacy of oral administration of pregabalin as an adjunct to phenobarbital, potassium bromide, or a combination of phenobarbital and potassium bromide for treatment of dogs with poorly controlled suspected idiopathic epilepsy. ... Animals—11 client-owned dogs suspected of having idiopathic epilepsy that was inadequately controlled with phenobarbital, potassium bromide, or a combination of these 2 drugs. ... Results—Seizures were significantly reduced (mean, 57%; median, 50%) after pregabalin administration in the 9 dogs that completed the study; 7 were considered responders with mean and median seizure reductions of 64% and 58%, respectively. Adverse effects for pregabalin were reported in 10 dogs. Mean and median plasma pregabalin concentrations for all dogs were 6.4 and 7.3 μg/mL, respectively. Conclusions and Clinical Relevance—Pregabalin may hold promise as a safe and effective adjunct anticonvulsant drug for epileptic dogs poorly controlled with the standard drugs phenobarbital or potassium bromide. Adverse effects of pregabalin appeared to be mild. Additional studies with larger numbers of dogs and longer follow-up intervals are warranted."
Dietary supplementation with medium-chain TAG has long lasting cognition-enhancing effects in aged dogs. Pan Y, Larson B, Araujo JA. British J. Nutr. June 2010;103:1746–54. Quote: "The present study focused on the hypothesis that dietary supplementation with medium-chain TAG (MCT) will improve cognitive function in aged dogs by providing the brain with energy in the form of ketones. Aged Beagle dogs were subjected to a baseline battery of cognitive tests, which were used to establish cognitively equivalent control or treatment groups. The dogs in the treatment group were maintained on a diet supplemented with 5·5 % MCT. After an initial wash-in period, all the dogs were tested with a battery of cognitive test protocols, which assessed sequentially landmark discrimination learning ability, egocentric visuospatial function and attention. The groups were maintained on the diets for 8 months. The MCT-supplemented group showed significantly better performance in most of the test protocols than the control group. The group differences also varied as a function of task difficulty, with the more difficult task showing greater supplementation effects than the easier tasks. The group given the MCT supplement showed significantly elevated levels of β-hydroxybutyrate, a ketone body. These results indicate, first, that long-term supplementation with MCT can have cognition-improving effects, and second, that MCT supplementation increases circulating levels of ketones. The results support the hypothesis that brain function of aged dogs can be improved by MCT supplementation, which provides the brain with an alternative energy source."
Seizure Management in Dogs: Going Beyond Standard Therapy. C.W. Dewey. October 2010. Quote: "A common misconception concerning seizure management is that the achievement of no more than one seizure per month should be the goal of therapy. Such a goal would be of little benefit to the dog presenting with a history of monthly seizure activity. Alternatively, a dog that seizures daily prior to drug intervention and experiences two seizures per month afterwards would be incorrectly considered a treatment failure, using such arbitrary criteria. Concerns over potential side effects of drug therapy are based primarily on the use of phenobarbital and bromide. With the advent of the newer anticonvulsant drugs to be discussed in this presentation, improved seizure control is often possible without concurrent adverse side effects. There are a number of so-called “new” drugs for dogs with epilepsy, and they are discussed below in order of my perception of most to least effective. I will also briefly discuss a drug called pregabalin for which we recently reported the results of a clinical trial in refractory epileptics. My opinion is that pregabalin is often an effective drug. ... Gabapentin is a structural analog of GABA. Gabapentin is thought to exert its antiseizure effects via binding to the α2δ subunit of voltage-gated neuronal calcium channels. Long-term toxicity trials for gabapentin have not been reported in dogs. However, the drug seems to be very well tolerated by this species, usually with no side-effects. Sedation does not appear to be a common problem with gabapentin use in dogs, but occasionally occurs. There are two clinical reports of gabapentin use as an add-on drug for dogs with refractory epilepsy. Overall, the responder rate of these dogs was between 41% and 55%. In the author’s experience, gabapentin is moderately effective as an anticonvulsant drug in dogs. ... My colleagues and I have completed an oral pharmacokinetic study of pregabalin in both dogs and cats, and a clinical trial of pregabalin in refractory epileptic dogs. The median seizure reduction in the clinical study was approximately 50%."
Idiopathic Epilepsy in Dogs and Cats. William B. Thomas. Vet. Clin. Small. Anim. 2010;40:161–179. Quote: "Gabapentin binds to neuronal voltage-gated calcium channels, inhibiting calcium flow. A major advantage of this drug in people is that it is excreted unchanged by the kidneys, is not metabolized by the liver, and has little or no potential for drug interactions. In dogs, however, gabapentin is partially metabolized to N-methyl-gabapentin, with an elimination half life of 3 to 4 hours. Gabapentin improves seizure control when added to phenobarbital and/or bromide. A recommended starting dose is 10 mg/kg every 8 hours. Mild sedation and ataxia are the most common side effects."
Breed Predispositions to Disease in Dogs & Cats (2d Ed.). Alex Gough, Alison Thomas. 2010; Wiley-Blackwell Publ. 53.
The association between Chiari-like malformation, ventriculomegaly and seizures in cavalier King Charles spaniels. C.J. Driver, K. Chandler, G. Walmsley, N. Shihab, H.A. Volk. Vety.J. Feb. 2013;195(2):235-237. Quote: "Cavalier King Charles spaniels (CKCSs) with Chiari-like malformation (CM) and associated seizures are frequently diagnosed with idiopathic epilepsy. There could be an association between ventriculomegaly (V) or caudal fossa overcrowding (CCFP) and seizures. A retrospective case-control study was performed using MRI to investigate the possible association between these morphological abnormalities and seizures. Seizure semiology and, where possible, electroencephalographic (EEG) abnormalities were documented. Eighty-five CKCS with CM were included, 27 with seizures. There was no association between V or CCFP and seizures (P = 0.10 and 0.71, respectively). Seizures were classified as having partial onset [meaning that they occur in in one area of the brain, unlike generalized seizures which typically affect nerve cells throughout the brain] in 61% of individuals in the study population (95% CI 42.41–76.43%). Another cause of recurrent seizures in CKCS (such as familial epilepsy) is suspected, as previously reported."
Double-Masked, Placebo-Controlled Study of Intravenous Levetiracetam for the Treatment of Status Epilepticus and Acute Repetitive Seizures in Dogs. B.T. Hardy, E. E. Patterson, J.M. Cloyd, R.M. Hardy, I.E. Leppik. J.Vet.Inter.Med. March 2012;26(2):334-340. Quote: "Background: Status epilepticus (SE) and acute repetitive seizures (ARS) are common canine neurologic emergencies. No evidence-based studies are available to guide treatment in veterinary patients. Parenteral levetiracetam (LEV) has many favorable properties for the emergency treatment of seizures, but its safety and efficacy in dogs for SE and ARS are unknown. Hypothesis: Intravenous LEV is superior to placebo in controlling seizures in dogs with SE or ARS after treatment with IV diazepam. Animals: Nineteen client-owned dogs admitted for SE or ARS. Methods: Randomized, placebo-controlled, double-masked study. Dogs with SE or ARS were randomized to receive IV LEV (30 or 60 mg/kg using an adaptive dose-escalation approach) or placebo, in addition to standard of care treatment. They were monitored for at least 24 hours after admission for additional seizures. Results: The responder rate (defined as dogs with no additional seizures after administration of the study medication) after LEV was 56% compared with 10% for placebo (P = .06). Dogs in the placebo group required significantly more boluses of diazepam compared with the LEV group (P < .03). Seizure etiologies identified were idiopathic epilepsy (n = 10), inflammatory central nervous system disease (n = 4), intracranial neoplasia (n = 2), hepatic encephalopathy (n = 1), and 2 dogs had no cause determined. No serious adverse effects were attributable to LEV administration. Conclusions and Clinical Importance: LEV was safe and potentially effective for the treatment of SE and ARS in these client-owned dogs. Larger, controlled clinical trials are needed to confirm this preliminary observation."
Prevalence and risk factors for canine epilepsy of unknown origin in the UK. L. Kearsley-Fleet, D. G. O’Neill, H. A. Volk, D. B. Church, D. C. Brodbelt. Vet. Rec. January 2013;172(13):338. Quote: "Epidemiological evaluation of canine epilepsy is an under-researched area. The objectives of this study were to estimate prevalence and investigate risk factors for epilepsy of unknown origin (EUO) among dogs attending primary veterinary practices in the UK. The clinical data analysed spanned a two-year period and included all dogs attending 92 primary veterinary clinics participating in the VetCompass project. Five hundred and thirty-nine EUO cases were identified giving a prevalence of 0.62% (95% CI 0.57% to 0.67%). Males were over 1.5 times as likely to have EUO compared with females (95% CI 1.44 to 2.06; P < 0.001). Of purebred dogs, the border terrier had 2.70 (95% CI 1.57 to 4.62; P < 0.001) and the German shepherd dog had 1.90 (95% CI 1.28 to 2.80; P=0.001) times increased odds of EUO compared with crossbred dogs. [Cavalier King Charles spaniel had 0.88 times.] In addition, the West Highland white terrier had reduced odds (OR 0.23; 95% CI 0.08 to 0.62; P=0.004) of EUO compared with crossbred dogs (likelihood ratio test P < 0.0001). ... No association was found with neuter status, colour or weight. ... Idiopathic epilepsy (IE) has also been seen more frequently in solid coat-colour Cavalier King Charles spaniels indicating that the number of colours may have some association with the disease (Rusbridge 2005). ... The current study highlights the clinical importance of epilepsy as a canine disorder in the UK. Increased awareness of sex and breed predispositions may assist clinicians with diagnosis. Further research is merited to evaluate the specific breed associations identified."
Prevalence of Lateral Ventricle Asymmetry in Brain MRI Studies of Neurologically Normal Dogs and Dogs with Idiopathic Epilepsy. Mauro Pivetta, Luisa De Risio, Richard Newton, Ruth Dennis. Vet.Radiology&Ultrasound. Sept. 2013;54(5):516-521. Quote: "Asymmetry of the cerebral lateral ventricles is a common finding in cross-sectional imaging of otherwise normal canine brains and has been assumed to be incidental. The purpose of this retrospective study was to compare the prevalence of ventricular asymmetry in brain MRI studies of normal dogs and dogs with idiopathic epilepsy. Brain MRI archives were searched for 100 neurologically normal dogs (Group 1) and 100 dogs with idiopathic epilepsy (Group 2). For each dog, asymmetry of the lateral ventricles was subjectively classified as absent, mild, moderate, and severe based on a consensus of two observers who were unaware of group status. ... The prevalence of asymmetry was 38% in Group 1 dogs and 44% in Group 2 dogs. Asymmetry was scored as mild in the majority of Group 2 dogs. There was no significant association between presence/absence and degree of ventricular asymmetry vs. dog group, age, gender, or skull conformation. Findings from the current study supported previously published assumptions that asymmetry of the lateral cerebral ventricles is an incidental finding in MRI studies of the canine brain."
Pediatric Seizure Disorders in Dogs and Cats. James A. Lavely. Vet. Clinics of No. America: Small Animal Prac. Dec. 2013. Quote: "Seizure disorders in young animals pose different considerations as to cause and therapeutic decisions compared with adult animals. Infectious diseases of the nervous system are more likely in puppies and kittens compared with adults. The diagnosis of canine distemper is often based on clinical signs. Idiopathic epilepsy typically occurs in dogs between 1 and 5 years of age; however, inflammatory brain diseases such as necrotizing encephalitis and granulomatous meningoencephalomyelitis also commonly occur in young to middle-aged small-breed dogs. The choice of which anticonvulsant to administer for maintenance therapy is tailored to each individual patient. ... A 6-month-old Cavalier King Charles spaniel was reported to have seizures secondary to a hexanoylglycine aciduria."
Unusual manifestation of bromide toxicity (bromism) in an idiopathic epileptic dog already treated with phenobarbital. Fabio Stabile, Alberta de Stefani, and Luisa De Risio. Veterinary Record Case Report. April 2014;2(1). Quote: "A three-year seven-month-old female spayed Cavalier King Charles spaniel was diagnosed with idiopathic epilepsy. Because of poor seizure control, the dog was started on oral treatment with potassium bromide as adjunctive treatment to phenobarbital. The dog presented eight days following bromide loading, having developed sedation, general proprioceptive ataxia and generalised appendicular repetitive myoclonus [twitching of the limbs]. The serum bromide concentration was 15.9 mg/ml (target range 1 mg/ml to 2.5 mg/ml), which was suggestive of a bromide overdose. The dog improved after reduction of bromide dosing and no similar episodes were reported by the owners at a follow up of 26 months. To the authors’ knowledge this is the first report describing generalised repetitive myoclonus related to bromide toxicity."
Validation of the diagnosis canine epilepsy in a Swedish animal insurance database against practice records. Linda Heske, Mette Berendt, Karin Hultin Jäderlund, Agneta Egenvall, Ane Nødtvedt. Preventive Vet. Med. June 2014;114(3-4):145-150. Quote: "Canine epilepsy is one of the most common neurological conditions in dogs but the actual incidence of the disease remains unknown. A Swedish animal insurance database has previously been shown useful for the study of disease occurrence in companion animals. The dogs insured by this company represent a unique population for epidemiological studies, because they are representative of the general dog population in Sweden and are followed throughout their life allowing studies of disease incidence to be performed. The database covers 50% of all insured dogs (in the year 2012) which represents 40% of the national dog population. Most commonly, dogs are covered by both veterinary care insurance and life insurance. Previous studies have shown that the general data quality is good, but the validity of a specific diagnosis should be examined carefully before using the database for incidence calculations. The aim of the current study was therefore to validate the information contained in the insurance database regarding canine epilepsy. The validation focused on the positive predictive value and the data-transfer from the veterinary practice records to the insurance database. The positive predictive value was defined as the proportion of recorded cases that actually had the disease in question. The quality of the data-transfer was assessed by comparing the diagnostic codes in practice records to the codes in the insurance database. The positive predictive value of the diagnostic codes for canine epilepsy (combining “epileptic convulsions” and “idiopathic epilepsy”) in the insurance database was validated in a cross-sectional study where insurance claims for canine epilepsy were compared to diagnostic information in practice records. A random sample of dogs with a reimbursed insurance claim during 2006 was included in the study sample (n = 235). Practice records were requested by mail from attending veterinarians. Two independent examiners scrutinized all the records. All 235 dogs were coded correctly in the database as they really had suffered seizures with or without convulsions, and the quality of the data-transfer was therefore excellent. In total, 167 dogs (71%) were classified as cases of canine epilepsy according to pre-defined criteria, and the positive predictive value was therefore considered relatively high. The most common breeds were mongrel (n = 26), Labrador retriever (n = 26), Cavalier King Charles spaniel (n = 11), Golden retriever (n = 10) and and German shepherd (n = 10). Based on these results, it was concluded that the data regarding canine epilepsy in the insurance database can be used for further population studies."
Pharmacokinetics of levetiracetam in epileptic dogs when administered concurrently with phenobarbital, bromide, or phenobarbital and bromide in combination. K.R. Muñana, J.A. Nettifee-Osborne, M.G. Papich. J.Vet.Int.Med. July 2014;28(4):1358. Quote: "Levetiracetam (LEV) is a common add-on antiepileptic medication (AED) for dogs with refractory seizures. Concurrent phenobarbital administration alters the disposition of LEV in healthy dogs. The objective of this study was to evaluate the pharmacokinetics of LEV in epileptic dogs when administered concurrently with conventional AEDs. Eighteen client-owned dogs on maintenance therapy with LEV and phenobarbital (PB group, n = 6), LEV and bromide (BR group, n = 6) or LEV, phenobarbital and bromide (PB-BR group, n = 6) were enrolled. All AEDs had attained steady state concentrations. Blood samples were collected at 0, 1, 2, 4 and 6 hours after a morning dose of LEV. Plasma LEV concentrations were determined by high-pressure liquid chromatography. To account for dose differences among dogs, LEV concentrations were normalized to the mean study dose (26.4 mg/kg). Pharmacokinetic analysis was performed on adjusted concentrations using a noncompartmental method, and AUC calculated using the trapezoidal method. Compared to the PB and PB-BR groups, the BR group had significantly higher Cmax (70.6 ± 24.0 μg/mL, versus 35.5 ± 13.7 μg/mL and 25.3 ± 9.0 μg/mL, respectively) and AUC0-Cn (314.2 ± 114.3 h*μg/mL versus 127.0 ± 64.7 h*μg/mL and 91.0 ± 42.2 h*μg/mL, respectively), and significantly lower CL/F (68.9 ± 22.1 mL/h/kg versus 172.1 ± 81.9 mL/h/kg and 247.6 ± 126.9 mL/h/kg, respectively). Concurrent administration of phenobarbital alone or in combination with bromide significantly alters the disposition of LEV in epileptic dogs compared to concurrent administration of bromide alone. These findings warrant consideration when utilizing LEV for add-on therapy in dogs with epilepsy."
A cohort study of epilepsy among 665,000 insured dogs: Incidence, mortality and survival after diagnosis. L. Heske, A. Nødtvedt, K. Hultin Jäderlund, M. Berendt, A. Egenvall. Vet.J. October 2014. Quote: "The main objective of this study was to estimate the incidence and mortality rates of epilepsy in a large population of insured dogs and to evaluate the importance of a variety of risk factors. Survival time after a diagnosis of epilepsy was also investigated. The Swedish animal insurance database used in this study has previously been helpful in canine epidemiological investigations. More than 2,000,000 dog-years at-risk (DYAR) were available in the insurance database. In total, 5013 dogs had at least one veterinary care claim for epilepsy [including 173 cavalier King Charles spaniels], and 2327 dogs were euthanased or died because of epilepsy. Based on veterinary care claims the incidence rate of epilepsy (including both idiopathic and symptomatic cases) was estimated to be 18 per 10,000 DYAR. Dogs were followed up until they were 10 (for life insurance claims) or 12 years of age (veterinary care claims). Among the 35 most common breeds in Sweden, the Boxer was at the highest risk of epilepsy with 60.3 cases per 10,000 DYAR, and also had the highest mortality rate of 46.7 per 10,000 DYAR (based on life insurance claims). Overall, males were at a higher risk than females (1.4:1). Median survival time (including euthanasia and death) after diagnosis was 1.5 years. In general, breeds kept solely for companionship lived longer after diagnosis than those kept for dual-purposes, such as hunting and shepherd and working breeds. The study demonstrates marked breed differences in incidence and mortality rates, which are assumed to reflect genetic predisposition to epilepsy."
Treatment in canine epilepsy - a systematic review. Marios Charalambous, David Brodbelt, Holger A Volk. BMC Vet. Research. Oct. 2014;10:257. Quote: "Background: Various antiepileptic drugs (AEDs) are used for the management of canine idiopathic epilepsy (IE). Information on their clinical efficacy remains limited. A systematic review was designed to evaluate existing evidence for the effectiveness of AEDs for presumptive canine IE. Electronic searches of PubMed and CAB Direct were carried out without date or language restrictions. Conference proceedings were also searched. Peer-reviewed full-length studies describing objectively the efficacy of AEDs in dogs with IE were included. Studies were allocated in two groups, i.e. blinded randomized clinical trials (bRCTs), non-blinded randomized clinical trials (nbRCTs) and non-randomized clinical trials (NRCTs) (group A) and uncontrolled clinical trials (UCTs) and case series (group B). Individual studies were evaluated based on the quality of evidence (study design, study group sizes, subject enrolment quality and overall risk of bias) and the outcome measures reported (in particular the proportion of dogs with ≥50% reduction in seizure frequency). Results: Twenty-six studies, including two conference proceedings, reporting clinical outcomes of AEDs used for management of IE were identified. Heterogeneity of study designs and outcome measures made meta-analysis inappropriate. Only four bRCTs were identified in group A and were considered to offer higher quality of evidence mong the studies. A good level of evidence supported the efficacy of oral phenobarbital and imepitoin and fair level of evidence supported the efficacy of oral potassium bromide and levetiracetam. For the remaining AEDs, favorable results were reported regarding their efficacy, but there was insufficient evidence to support their use due to lack of bRCTs. Conclusions: Oral phenobarbital and imepitoin in particular, as well as potassium bromide and levetiracetam are likely to be effective for the treatment of IE. However, variations in baseline characteristics of the dogs involved, significant differences between study designs and several potential sources of bias preclude definitive recommendations. There is a need for greater numbers of adequately sized bRCTs evaluating the efficacy of AEDs for IE."
Clinical efficacy and safety of imepitoin in comparison with phenobarbital for the control of idiopathic epilepsy in dogs. Tipold, A., Keefe, T. J., Loscher, W., Rundfeldt, C., de Vries, F. Vet. Pharm. & Therapeutics. April 2015;38(2):160-168. Quote: "The anticonvulsant activity and safety of imepitoin, a novel antiepileptic drug licensed in the European Union, were evaluated in a multicentre field efficacy study as well as in a safety study under laboratory conditions. Efficacy of imepitoin was compared with phenobarbital in 226 client-owned dogs in a blinded parallel group design. The administration of imepitoin twice daily in incremental doses of 10, 20 or 30 mg/kg demonstrated comparable efficacy to phenobarbital in controlling seizures in dogs. The frequency of adverse events including somnolence/sedation, polydipsia and increased appetite was significantly higher in the phenobarbital group. In phenobarbital-treated dogs, significantly increased levels of alkaline phosphatase, gamma-glutamyl-transferase and other liver enzymes occurred, while no such effect was observed in the imepitoin group. In a safety study under laboratory conditions, healthy beagle dogs were administered 0, 30, 90 or 150 mg/kg imepitoin twice daily for 26 weeks. A complete safety evaluation including histopathology was included in the study. A no-observed-adverse-event level of 90 mg/kg twice daily was determined. These results indicate that imepitoin is a potent and safe antiepileptic drug for dogs."
Assessment into the usage of levetiracetam in a canine epilepsy clinic. Rowena MA Packer, George Nye, Sian Elizabeth Porter, holger A Volk. BMC Vet. Research. February 2015. Quote: "Background: The purpose of this retrospective study was to describe the use of LEV in a canine epilepsy clinic and determine the long-term efficacy and tolerability of LEV in veterinary clinical practice. The electronic database of a UK based referral hospital was searched for LEV usage in dogs with seizures. Information and data necessary for the evaluation were obtained from a combination of electronic and written hospital records, the referring veterinary surgeons? records and telephone interviews with dog owners. Only dogs that were reportedly diagnosed with idiopathic epilepsy were included in the study. Results: Fifty-two dogs [including one cavalier King Charles spaniel] were included in this retrospective study. Two treatment protocols were recognised; 29 dogs were treated continuously with LEV and 23 dogs received interval or pulse treatment for cluster seizures. LEV treatment resulted in 69% of dogs having a 50% or greater reduction of seizure frequency whilst 15% of all the dogs were completely free from seizures. Seizure frequency reduced significantly in the whole population. No dog was reported to experience life-threatening side effects. Mild side effects were experienced by 46% of dogs and a significantly higher number of these dogs were in the pulse treatment group. The most common side-effects reported were sedation and ataxia. Conclusions: LEV appears to be effective and well tolerated for reduction of seizures."
Effect of Chronic Administration of Phenobarbital, or Bromide, on Pharmacokinetics of Levetiracetam in Dogs with Epilepsy. K.R. Muñana, J.A. Nettifee-Osborne, M.G. Papich. J.Vet. Int. Med. February 2015. Quote: "Background: Levetiracetam (LEV) is a common add-on antiepileptic drug (AED) in dogs with refractory seizures. Concurrent phenobarbital administration alters the disposition of LEV in healthy dogs. Hypothesis/Objectives: To evaluate the pharmacokinetics of LEV in dogs with epilepsy when administered concurrently with conventional AEDs. Animals: Eighteen client-owned dogs on maintenance treatment with LEV and phenobarbital (PB group, n = 6), LEV and bromide (BR group, n = 6) or LEV, phenobarbital and bromide (PB–BR group, n = 6). Methods: Prospective pharmacokinetic study. Blood samples were collected at 0, 1, 2, 4, and 6 hours after LEV administration. Plasma LEV concentrations were determined by high-pressure liquid chromatography. To account for dose differences among dogs, LEV concentrations were normalized to the mean study dose (26.4 mg/kg). Pharmacokinetic analysis was performed on adjusted concentrations, using a noncompartmental method, and area-under-the-curve (AUC) calculated to the last measured time point. Results: Compared to the PB and PB–BR groups, the BR group had significantly higher peak concentration (Cmax) (73.4 ± 24.0 versus 37.5 ± 13.7 and 26.5 ± 8.96 μg/mL, respectively, P < .001) and AUC (329 ± 114 versus 140 ± 64.7 and 98.7 ± 42.2 h*μg/mL, respectively, P < .001), and significantly lower clearance (CL/F) (71.8 ± 22.1 versus 187 ± 81.9 and 269 ± 127 mL/h/kg, respectively, P = .028). Conclusions and Clinical Importance: Concurrent administration of PB alone or in combination with bromide increases LEV clearance in epileptic dogs compared to concurrent administration of bromide alone. Dosage increases might be indicated when utilizing LEV as add-on treatment with phenobarbital in dogs."
International Veterinary Epilepsy Task Force’s current understanding of idiopathic epilepsy of genetic or suspected genetic origin in purebred dogs. Velia-Isabel Hülsmeyer, Andrea Fischer, Paul J.J. Mandigers, Luisa DeRisio, Mette Berendt, Clare Rusbridge, Sofie F.M. Bhatti, Akos Pakozdy, Edward E. Patterson, Simon Platt, Rowena M.A. Packer, Holger A. Volk. BMC Vet. Res. September 2015;11:175. Quote: "Canine idiopathic epilepsy is a common neurological disease affecting both purebred and crossbred dogs. Various breed-specific cohort, epidemiological and genetic studies have been conducted to date, which all improved our knowledge and general understanding of canine idiopathic epilepsy, and in particular our knowledge of those breeds studied. However, these studies also frequently revealed differences between the investigated breeds with respect to clinical features, inheritance and prevalence rates. Awareness and observation of breed-specific differences is important for successful management of the dog with epilepsy in everyday clinical practice and furthermore may promote canine epilepsy research. The following manuscript reviews the evidence available for breeds which have been identified as being predisposed to idiopathic epilepsy with a proven or suspected genetic background, and highlights different breed specific clinical features (e.g. age at onset, sex, seizure type), treatment response, prevalence rates and proposed inheritance reported in the literature. In addition, certain breed-specific diseases that may act as potential differentials for idiopathic epilepsy are highlighted. --- Cavalier King Charles Spaniel: For several years it has been suggested that idiopathic epilepsy may occur as an independent disease in this breed and may not be the consequence of the frequently occurring Chiari-like malformation. This hypothesis was supported by a study from 2013 that did not find a significant association between the degree of the Chiari-like malformation, (such as degree of ventriculomegaly) and the occurrence of epileptic seizures. However, an overlapping of the two diseases cannot be entirely excluded. According to the findings of the study published in 2013 the seizure type was defined as (primary) generalised epileptic seizures in 39% of the dogs, as focal epileptic seizures in 36% and as focal epileptic seizures evolving into generalised seizures in 25% of dogs. No detailed data regarding potential modes of inheritance are available; however, epilepsy was found more frequently in lines originating from whole-colour dogs. Potential breed-specific diseases that may mimic idiopathic epilepsy: Cavalier King Charles Spaniels are also known to suffer from Episodic Falling (paroxysmal exercise-induced dyskinesia). Episodic falling is a movement disorder that typically manifests between the age of 4 months and four years. Falling episodes are induced by physical activity, stress and excitement and manifest with hypertonicity of the limbs resulting in inability to move or even complete collapse. In contrast to epileptic seizures, consciousness usually is not affected during these episodes. A gene test is available for episodic falling that is based on evidence of a BCAN (brevican) mutation. Older Cavalier King Charles spaniels (>5 years old) have a high prevalence of myoclonus [spasmodic jerky contraction of groups of muscles], which manifests most commonly as a brief jerking of the head and forelimbs when the dog is standing or sitting. Initially the syndrome is relatively benign but can be progressive with affected dogs suffering frequent jerks which may interfere with function, for example cause the dog to fall or stumble. The syndrome can be confused with focal epileptic seizures but generally does not respond to AEDs [antiepileptic drugs] licenced for dogs although may respond to levetiracetam (personal communication Clare Rusbridge February 2015). The pathogenesis of the myoclonus is as yet undetermined."
International veterinary epilepsy task force consensus proposal: diagnostic approach to epilepsy in dogs. Luisa De Risio, Sofie Bhatti, Karen Muñana, Jacques Penderis, Veronika Stein, Andrea Tipold, Mette Berendt, Robyn Farqhuar, Andrea Fischer, Sam Long, Paul JJ. Mandigers, Kaspar Matiasek, Rowena MA Packer, Akos Pakozdy, Ned Patterson, Simon Platt, Michael Podell, Heidrun Potschka, Martí Pumarola Batlle, Clare Rusbridge, Holger A. Volk. BMC Vet. Res. September 2015;11:148. Quote: "This article outlines the consensus proposal on diagnosis of epilepsy in dogs by the International Veterinary Epilepsy Task Force. The aim of this consensus proposal is to improve consistency in the diagnosis of epilepsy in the clinical and research settings. The diagnostic approach to the patient presenting with a history of suspected epileptic seizures incorporates two fundamental steps: to establish if the events the animal is demonstrating truly represent epileptic seizures and if so, to identify their underlying cause. Differentiation of epileptic seizures from other non-epileptic episodic paroxysmal events can be challenging. ... Certain movement disorders are breed-specific, generally occur in young dogs and their phenotype may be well characterised. To date the associated genetic defect (e.g., deletion in the gene BCAN) has been identified only in Cavalier King Charles spaniels with paroxysmal exercise-induced dyskinesia (also known as episodic falling). ... Criteria that can be used to make this differentiation are presented in detail and discussed. Criteria for the diagnosis of idiopathic epilepsy (IE) are described in a three-tier system. Tier I confidence level for the diagnosis of IE is based on a history of two or more unprovoked epileptic seizures occurring at least 24 h apart, age at epileptic seizure onset of between six months and six years, unremarkable inter-ictal physical and neurological examination, and no significant abnormalities on minimum data base blood tests and urinalysis. Tier II confidence level for the diagnosis of IE is based on the factors listed in tier I and unremarkable fasting and post-prandial bile acids, magnetic resonance imaging (MRI) of the brain (based on an epilepsy-specific brain MRI protocol) and cerebrospinal fluid (CSF) analysis. Tier III confidence level for the diagnosis of IE is based on the factors listed in tier I and II and identification of electroencephalographic abnormalities characteristic for seizure disorders. The authors recommend performing MRI of the brain and routine CSF analysis, after exclusion of reactive seizures, in dogs with age at epileptic seizure onset <6 months or >6 years, inter-ictal neurological abnormalities consistent with intracranial neurolocalisation, status epilepticus or cluster seizure at epileptic seizure onset, or a previous presumptive diagnosis of IE and drug-resistance with a single antiepileptic drug titrated to the highest tolerable dose. This consensus article represents the basis for a more standardised diagnostic approach to the seizure patient. These recommendations will evolve over time with advances in neuroimaging, electroencephalography, and molecular genetics of canine epilepsy."
International veterinary epilepsy task force consensus proposal: outcome of therapeutic interventions in canine and feline epilepsy. Heidrun Potschka, Andrea Fischer, Wolfgang Löscher, Ned Patterson, Sofie Bhatti, Mette Berendt, Luisa De Risio, Robyn Farquhar, Sam Long, Paul Mandigers, Kaspar Matiasek, Karen Muñana, Akos Pakozdy, Jacques Penderis, Simon Platt, Michael Podell, Clare Rusbridge, Veronika Stein, Andrea Tipold, Holger A Volk. BMC Vet. Res. September 2015;11:177. Quote: "Common criteria for the diagnosis of drug resistance and the assessment of outcome are needed urgently as a prerequisite for standardized evaluation and reporting of individual therapeutic responses in canine epilepsy. Thus, we provide a proposal for the definition of drug resistance and partial therapeutic success in canine patients with epilepsy. This consensus statement also suggests a list of factors and aspects of outcome, which should be considered in addition to the impact on seizures. Moreover, these expert recommendations discuss criteria which determine the validity and informative value of a therapeutic trial in an individual patient and also suggest the application of individual outcome criteria. Agreement on common guidelines does not only render a basis for future optimization of individual patient management, but is also a presupposition for the design and implementation of clinical studies with highly standardized inclusion and exclusion criteria. Respective standardization will improve the comparability of findings from different studies and renders an improved basis for multicenter studies. Therefore, this proposal provides an in-depth discussion of the implications of outcome criteria for clinical studies. In particular ethical aspects and the different options for study design and application of individual patient-centered outcome criteria are considered."
A randomised trial of a medium-chain TAG diet as treatment for dogs with idiopathic epilepsy. Tsz Hong Lawa1a, Emma S. S. Daviesa, Yuanlong Pana, Brian Zanghia, Elizabeth Wanta, Holger A. Volk. Brit. J. Nutrition. September 2015. Quote: "Despite appropriate antiepileptic drug treatment, approximately one-third of humans and dogs with epilepsy continue experiencing seizures, emphasising the importance for new treatment strategies to improve the quality of life of people or dogs with epilepsy. A 6-month prospective, randomised, double-blinded, placebo-controlled cross-over dietary trial was designed to compare a ketogenic medium-chain TAG diet (MCTD) with a standardised placebo diet in chronically antiepileptic drug-treated dogs with idiopathic epilepsy. Dogs were fed either MCTD or placebo diet for 3 months followed by a subsequent respective switch of diet for a further 3 months. Seizure frequency, clinical and laboratory data were collected and evaluated for twenty-one dogs completing the study. ... This study included twenty-one dogs of seventeen different breeds including the following: American bulldog, two Beagles, two Border Collies, Boxer, Cavalier King Charles Spaniel, English Bull Terrier, English Springer Spaniel, German Shepherd, Golden Retriever, Lhasa Apso, Mastiff, Rhodesian Ridgeback, Saint Bernard, Siberian Husky, Slovakian Rough Haired Pointer, Welsh Springer Spaniel, and three cross breeds. ... Seizure frequency was significantly lower when dogs were fed the MCTD (2·31/month, 0–9·89/month) in comparison with the placebo diet (2·67/month, 0·33–22·92/month, P=0·020); three dogs achieved seizure freedom, seven additional dogs had ≥50 % reduction in seizure frequency, five had an overall <50 % reduction in seizures (38·87 %, 35·68–43·27 %) and six showed no response. Seizure day frequency were also significantly lower when dogs were fed the MCTD (1·63/month, 0–7·58/month) in comparison with the placebo diet (1·69/month, 0·33–13·82/month, P=0·022). Consumption of the MCTD also resulted in significant elevation of blood β-hydroxybutyrate concentrations in comparison with placebo diet (0·041 (sd 0·004) v. 0·031 (sd 0·016) mmol/l, P=0·028). There were no significant changes in serum concentrations of glucose (P=0·903), phenobarbital (P=0·422), potassium bromide (P=0·404) and weight (P=0·300) between diet groups. In conclusion, the data show antiepileptic properties associated with ketogenic diets and provide evidence for the efficacy of the MCTD used in this study as a therapeutic option for epilepsy treatment."
A single-blinded phenobarbital-controlled trial of levetiracetam as mono-therapy in dogs with newly diagnosed epilepsy. N. Fredsø, A. Sabers, N. Toft, A. Møller, M. Berendt. Vet. J. November 2015. Quote: "Treatment of canine epilepsy is problematic. Few antiepileptic drugs have proven efficacy in dogs and undesirable adverse effects and pharmacoresistance are not uncommon. Consequently, the need for investigation of alternative treatment options is ongoing. The objective of this study was to investigate the efficacy and tolerability of levetiracetam as mono-therapy in dogs with idiopathic epilepsy. The study used a prospective single-blinded parallel group design. Twelve client-owned dogs were included and were randomised to treatment with levetiracetam (30 mg/kg/day or 60 mg/kg/day divided into three daily dosages) or phenobarbital (4 mg/kg/day divided twice daily). Control visits were at days 30, 60 and then every 3 months for up to 1 year. Two or more seizures within 3 months led to an increase in drug dosage (levetiracetam: 10 mg/kg/day, phenobarbital: 1 mg/kg/day). Five of six levetiracetam treated dogs and one of six phenobarbital treated dogs withdrew from the study within 2–5 months due to insufficient seizure control. In the levetiracetam treated dogs there was no significant difference in the monthly number of seizures before and after treatment, whereas in the phenobarbital treated dogs there were significantly (P=0.013) fewer seizures after treatment. Five phenobarbital treated dogs were classified as true responders (≥50% reduction in seizures/month) whereas none of the levetiracetam treated dogs fulfilled this criterion. Adverse effects were reported in both groups but were more frequent in the phenobarbital group. In this study levetiracetam was well tolerated but was not effective at the given doses as mono-therapy in dogs with idiopathic epilepsy."
Vagus Nerve
Stimulator Placement in Dogs: Surgical Implantation Technique,
Complications, Long-Term Follow-Up, and Practical Considerations.
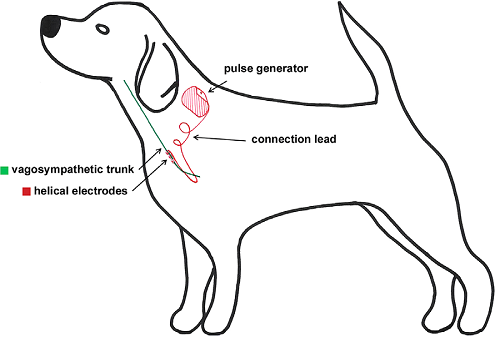 Valentine
Martle, Luc M. L. Van Ham, Paul Boon, Jacques Caemaert, Mulenda Tshamala,
Kristl Vonck, Robrecht Raedt, Ingeborgh Polis, Sofie Bhatti. Vet. Surg.
January 2016;45:71-78. Quote: Objective: To describe a modified implantation
procedure of a vagus nerve stimulation (VNS) device in dogs and to report
short- and long-term complications. Study Design: Descriptive, experimental
study. Animals: Healthy, adult Beagle dogs (n=10). Methods: A VNS
Therapy((R)) System was implanted in the left cervical region of
anesthetized dogs. During and within 48hours after surgery,
electrocardiography (ECG) and impedance testing of the system were
performed. Dogs were monitored daily and the impedance of the system was
determined regularly until VNS devices were surgically removed 3 years after
implantation. Results: The implantation procedure was successful in all dogs
without intraoperative complications. ECG monitoring and impedance tests
were within normal limits during and within 48 hours after surgery.
Post-operative seroma formation was common (70%). One dog developed an
irreversible Horner's syndrome leading to removal of the device 5 months
after implantation. Another dog developed trauma-induced damage of the lead
requiring surgical revision. The device could be safely removed in all dogs;
however, electrodes were left in place to avoid nerve damage. At removal,
the anchor tether was dislodged in 40% of dogs and the lead was twisted in
50% of dogs. Conclusion: Implantation of a VNS Therapy System is safe and
feasible in dogs; however, seroma formation, twisting of the lead, and
dislodgement of the anchor tether were common. Practical improvements in the
technique include stable device placement, use of a compression bandage, and
exercise restriction. Regular evaluation of lead impedance is important, as
altered values can indicate serious complications.
Valentine
Martle, Luc M. L. Van Ham, Paul Boon, Jacques Caemaert, Mulenda Tshamala,
Kristl Vonck, Robrecht Raedt, Ingeborgh Polis, Sofie Bhatti. Vet. Surg.
January 2016;45:71-78. Quote: Objective: To describe a modified implantation
procedure of a vagus nerve stimulation (VNS) device in dogs and to report
short- and long-term complications. Study Design: Descriptive, experimental
study. Animals: Healthy, adult Beagle dogs (n=10). Methods: A VNS
Therapy((R)) System was implanted in the left cervical region of
anesthetized dogs. During and within 48hours after surgery,
electrocardiography (ECG) and impedance testing of the system were
performed. Dogs were monitored daily and the impedance of the system was
determined regularly until VNS devices were surgically removed 3 years after
implantation. Results: The implantation procedure was successful in all dogs
without intraoperative complications. ECG monitoring and impedance tests
were within normal limits during and within 48 hours after surgery.
Post-operative seroma formation was common (70%). One dog developed an
irreversible Horner's syndrome leading to removal of the device 5 months
after implantation. Another dog developed trauma-induced damage of the lead
requiring surgical revision. The device could be safely removed in all dogs;
however, electrodes were left in place to avoid nerve damage. At removal,
the anchor tether was dislodged in 40% of dogs and the lead was twisted in
50% of dogs. Conclusion: Implantation of a VNS Therapy System is safe and
feasible in dogs; however, seroma formation, twisting of the lead, and
dislodgement of the anchor tether were common. Practical improvements in the
technique include stable device placement, use of a compression bandage, and
exercise restriction. Regular evaluation of lead impedance is important, as
altered values can indicate serious complications.
Effects of a ketogenic diet on ADHD-like behavior in dogs with idiopathic epilepsy. Rowena M.A. Packer, Tsz Hong Law, Emma Davies, Brian Zanghi, Yuanlong Pan, Holger A. Volk. Epilepsy & Behavior. February 2016;55:62-68. Quote: "Objectives: Epilepsy in humans and rodent models of epilepsy can be associated with behavioral comorbidities including an increased prevalence of attention-deficit/hyperactivity disorder (ADHD). Attention-deficit/hyperactivity disorder symptoms and seizure frequency have been successfully reduced in humans and rodents using a ketogenic diet (KD). The aims of this study were (i) to describe the behavioral profile of dogs with idiopathic epilepsy (IE) while on a standardized nonketogenic placebo diet, to determine whether ADHD-like behaviors [excitability, chasing, and trainability] are present, and (ii) to examine the effect of a ketogenic medium chain triglyceride diet (MCTD) on the behavioral profile of dogs with idiopathic epilepsy (IE) compared with the standardized placebo control diet, including ADHD-like behaviors. Methods: A 6-month prospective, randomized, double-blinded, placebo-controlled, crossover dietary trial comparing the effects of the MCTD with a standardized placebo diet on canine behavior was carried out. Dogs diagnosed with IE, with a seizure frequency of at least 3 seizures in the past 3 months (n=21), were fed the MCTD or placebo diet for 3 months andwere then switched to the alternative diet for 3 months. Owners completed a validated behavioral questionnaire to measure 11 defined behavioral factors at the end of each diet period to report their dogs' behavior, with three specific behaviors hypothesized to be related to ADHD: excitability, chasing, and trainability. Results: The highest scoring behavioral factors in the placebo and MCTD periods were excitability (mean ± SE: 1.910 ± 0.127) and chasing (mean ± SE: 1.824 ± 0.210). A markedly lower trainability score (mean ± SE: 0.437±0.125) than that of previously studied canine populations was observed. The MCTD resulted in a significant improvement in the ADHD-related behavioral factor chasing and a reduction in stranger-directed fear (p b 0.05) compared with the placebo diet. The latter effect may be attributed to previously described anxiolytic effects of a KD. Conclusions: These data support the supposition that dogs with IE may exhibit behaviors that resemble ADHD symptoms seen in humans and rodent models of epilepsy and that a MCTD may be able to improve some of these behaviors, along with potentially anxiolytic effects."
Risk factors for cluster seizures in canine idiopathic epilepsy. Rowena M.A. Packer, Nadia K. Shihaba, Bruno B.J. Torres, Holger A. Volk. Research in Vet. Sci. February 2016. Quote: "Cluster seizures (CS), two or more seizures within a 24-hour period, are reported in 38–77% of dogs with idiopathic epilepsy (IE). Negative outcomes associated with CS include a reduced likelihood of achieving seizure freedom, decreased survival time and increased likelihood of euthanasia. Previous studies have found factors including breed, sex and neuter status are associated with CS in dogs with IE; however, only one UK study in a multi-breed study of CS in IE patients exists to the author's knowledge, and thus further data is required to confirm these results. Data from 384 dogs treated at a multi-breed canine specific epilepsy clinic were retrospectively collected from electronic patient records. 384 dogs were included in the study, of which nearly half had a history of CS (49.1%). Dogs with a history of CS had a younger age at onset than those without (p = 0.033). In a multivariate model, three variables predicted risk of CS: a history of status epilepticus (p = 0.047), age at seizure onset (p = 0.066) and breed (German Shepherd Dog) (p < 0.001). Dogs with a history of status epilepticus and dogs with an older age at seizure onset were less likely to be affected by cluster seizures. German Shepherd Dogs (71% experiencing CS) were significantly more likely to suffer from CS compared to Labrador Retrievers (25%) (p < 0.001). ... The occurrence of CS [cluster seizures] in each individual breed was compared with the Labrador Retriever. GSDs (71% CS, p<0.001), Boxers (67%, p=0.001), Cavalier King Charles Spaniels (67%, p=0.002), Staffordshire Bull Terriers (62%, p=0.007) and Border Collies (62%, p=0.001) were significantly more likely to suffer from CS compared to Labrador Retrievers (25% CS) at the univariate level. No significant association was found between CS and size (48% large, 38% medium, 14% small; p>0.05). ... Although GSDs and Boxers were found to be more affected by CS than Labrador Retrievers in both studies, three further breeds, the Cavalier King Charles Spaniel, Staffordshire Bull Terriers and Border Collie were identified in this study at the univariate level. ... There was no association between sex, neuter status, body size and CS. Further studies into the pathophysiology and genetics of CS are required to further understand this phenomenon."
2015 ACVIM Small Animal Consensus Statement on Seizure Management in Dogs. M. Podell, H.A. Volk, M. Berendt, W. Löscher, K. Muñana, E.E. Patterson, S.R. Platt. J. Vet. Internal Med. February 2016. Quote: "This report represents a scientific and working clinical consensus statement on seizure management in dogs based on current literature and clinical expertise. The goal was to establish guidelines for a predetermined, concise, and logical sequential approach to chronic seizure management starting with seizure identification and diagnosis (not included in this report), reviewing decision-making, treatment strategies, focusing on issues related to chronic antiepileptic drug treatment response and monitoring, and guidelines to enhance patient response and quality of life. Ultimately, we hope to provide a foundation for ongoing and future clinical epilepsy research in veterinary medicine. ... When Should Treatment Be Started? ... The panel recommendations to initiate AED [antiepileptic drugs] treatment are summarized as follows: (i) Identifiable structural lesion present or prior history of brain disease or injury; (ii) Acute repetitive seizures or, status epilepticus (ictal event ≥5 minutes or ≥3 or more generalized seizures within a 24-hour period); (iii) ≥2 or more seizure events within a 6-month period; and (iv) Prolonged, severe, or unusual postictal periods. ... Which Drug Should Be Used First? ... Phenobarbital: High recommendation and likely be effective treatment. Potassium Bromide: Moderate recommendation and most likely to be effective treatment. Primidone: Not recommended for treatment and may be ineffective and/or dangerous to the patient. Imepitoin: High recommendation and likely be effective treatment. Levetiracetam: Low recommendation and may not be effective treatment. Zonisamide: Low recommendation and may not be effective treatment. ... How Should Monitoring Be Performed? ... What Are The Risks Of Treatment? ... When Should a Second AED Be Started and Which Should be Used? ... What Alternative Nonpharmacologic Treatments Are Available? ... ."
In vitro comparative evaluation and stability studies of different brands of pregabalin (75 mg) capsules marketed in Karachi, Pakistan: A case study. Muhammad Arif Asghar, Syed Baqir Shayum Naqvi. Sci.Int.(Lahore). May 2016;28(3):3091-3096. Quote: Pregabalin is a drug of choice for the treatment of epilepsy. Several brands are available in the market which makes it difficult to select the safe, effective and economic one. Therefore, the current study was designed to evaluate and compare the quality and physicochemical characteristics of six different pharmaceutical brands of Pregabalin (75 mg) capsules available in the pharmacies of Karachi, Pakistan. The comparison was based on different parameters such as, price, uniformity of dosage unit, disintegration time, dissolution assessment, chemical assay and stability of Pregabalin using standard methods. The result showed that almost all brands of Pregabalin are within the limits of manufacturers claim and meet USP/BP specifications. However, statistical calculations and similarity factor (f2) studies also revealed that all brands are pharmaceutically equivalent in their quality aspects. On the basis of achieved results, it was concluded that the cost-effective brands of Pregabalin should be utilized for the treatment of epilepsy.
Quality-of-life aspects in idiopathic epilepsy in dogs. A. Wessmann, H. A. Volk, R. M. A. Packer, M. Ortega, T. J. Anderson. Vet. Rec. September 2016;179(9):229-235. Quote: Quality of life (QoL) plays a significant role in the treatment of dogs with idiopathic epilepsy (IE), yet is so far understudied. This study describes the outcome evaluation of an online questionnaire based on the carer's perception focusing on 62 QoL questions in 159 dogs with IE. Results showed that seizure frequency, but not seizure severity or presence of cluster seizures, was significantly associated with carer-perceived dog's QoL. Dogs receiving third-line antiepileptic drugs had a significantly lower perceived QoL than those that did not. Generalised linear mixed model analysis demonstrated that severity of the side effects sleeping more and ataxia were significantly associated with carer-perceived dog's QoL, with higher severities predicting lower QoL scores. The degree of carer acceptability of seizure frequency and severity was significantly associated with the dog's reported seizure frequency and severity. Moreover, there was a significant association between IE-related QoL changes of the dog and the carer, with reductions in perceived canine QoL scores associated with reductions in carer QoL, and vice versa. In conclusion, aspects of canine IE can affect both the carer and their dog's QoL. This has implications for the management and requires consideration when treatment options and outcomes are discussed.
Retrospective epidemiological study of canine epilepsy in Japan using the International Veterinary Epilepsy Task Force classification 2015 (2003–2013): etiological distribution, risk factors, survival time, and lifespan. Yuji Hamamoto, Daisuke Hasegawa, Shunta Mizoguchi, Yoshihiko Yu, Masae Wada, Takayuki Kuwabara, Aki Fujiwara-Igarashi, Michio Fujita. BMC Vet. Res. November 2016;12:248. Quote: Background: Epilepsy is the most common neurological disease in veterinary practice. However, contrary to human medicine, epilepsy classification in veterinary medicine had not been clearly defined until recently. A number of reports on canine epilepsy have been published, reflecting in part updated proposals from the human epilepsy organization, the International League Against Epilepsy. In 2015, the International Veterinary Epilepsy Task Force (IVETF) published a consensus report on the classification and definition of canine epilepsy. The purpose of this retrospective study was to investigate the etiological distribution, survival time of dogs with idiopathic epilepsy (IdE) and structural epilepsy (StE), and risk factors for survival time, according to the recently published IVETF classification. We investigated canine cases with epilepsy that were referred to our teaching hospital in Japan during the past 10 years, and which encompassed a different breed population from Western countries. Results: A total of 358 dogs with epilepsy [12 cavalier King Charles spaniels] satisfied our etiological study criteria. Of these, 172 dogs (48 %) [one CKCS] were classified as IdE and 76 dogs (21 %) [one CKCS] as StE. Of these dogs, 100 dogs (consisting of 65 with IdE and 35 with StE) were included in our survival study. Median survival time from the initial epileptic seizure in dogs with IdE and StE was 10.4 and 4.5 years, respectively. Median lifespan of dogs with IdE and StE was 13.5 and 10.9 years, respectively. Multivariable analysis demonstrated that risk factors for survival time in IdE were high seizure frequency (≥0.3 seizures/month) and focal epileptic seizures. Conclusions: Focal epileptic seizures were identified as a risk factor for survival time in IdE. Clinicians should carefully differentiate seizure type as it is difficult to identify focal epileptic seizures. With good seizure control, dogs with IdE can survive for nearly the same lifespan as the general dog population. Our results using the IVETF classification are similar to previous studies, although some features were noted in our Japanese canine population (which was composed of mainly small-breed dogs), including a longer lifespan in dogs with epilepsy and a larger percentage of meningoencephalomyelitis of unknown origin in dogs with StE.
Clinical Features, Imaging Characteristics, and Long-term Outcome of Dogs with Cranial Meningocele or Meningoencephalocele. K. Lazzerini, R. Gutierrez-Quintana, R. José-López, F. McConnell, R. Gonçalves, J. McMurrough, S. De Decker, C. Muir, S.L. Priestnall, L. Mari, F. Stabile, L. De Risio, C. Loeffler, A. Tauro, C. Rusbridge, S. Rodenas, S. Añor, C. de la Fuente, A. Fischer, A. Bruehschwein, J. Penderis, J. Guevar. J. Vet. Internal Med. January 2017. Quote: Background: The term meningoencephalocele (MEC) describes a herniation of cerebral tissue and meninges through a defect in the cranium, whereas a meningocele (MC) is a herniation of the meninges alone. Hypothesis/Objectives: To describe the clinical features, magnetic resonance imaging (MRI) characteristics, and outcomes of dogs with cranial MC and MEC. Animals: Twenty-two client-owned dogs diagnosed with cranial MC or MEC [including one cavalier King Charles spaniel]. Methods: Multicentric retrospective descriptive study. Clinical records of 13 institutions were reviewed. Signalment, clinical history, neurologic findings and MRI characteristics as well as treatment and outcome were recorded and evaluated. Results: Most affected dogs were presented at a young age (median, 6.5 months; range, 1 month – 8 years). The most common presenting complaints were seizures and behavioral abnormalities. Intranasal MEC was more common than parietal MC. Magnetic resonance imaging identified meningeal enhancement of the protruded tissue in 77% of the cases. Porencephaly was seen in all cases with parietal MC. Cerebrospinal fluid (CSF) analysis identified mild abnormalities in 4 of 11 cases. Surgery was not performed in any affected dog. Seventeen patients were treated medically, and seizures were adequately controlled with anti-epileptic drugs in 10 dogs. Dogs with intranasal MEC and mild neurologic signs had a fair prognosis with medical treatment. Conclusion and clinical importance: Although uncommon, MC and MEC should be considered as a differential diagnosis in young dogs presenting with seizures or alterations in behavior. Medical treatment is a valid option with a fair prognosis when the neurologic signs are mild.
Phenobarbital or potassium bromide as an add-on antiepileptic drug for the management of canine idiopathic epilepsy refractory to imepitoin. E. Royaux, L. Van Ham, B.J.G. Broeckx, I. Van Soens, I. Gielen, D. Deforce, S.F.M. Bhatti. Vet. J. February 2017. Quote: Imepitoin has recently been approved in Europe for the management of dogs with idiopathic epilepsy. Currently, there is no evidence-based information available on the efficacy of antiepileptic drugs used as additions to the therapeutic regimen in dogs with idiopathic epilepsy that are not well controlled with imepitoin. The goal of this study was to evaluate the efficacy of phenobarbital or potassium bromide (KBr) as add-on antiepileptic drugs for controlling dogs refractory to a maximum dose of imepitoin (30 mg/kg twice daily). The study was performed as a prospective, randomised, controlled clinical trial. The efficacy of phenobarbital and KBr was evaluated by comparing monthly seizure frequency (MSF), monthly seizure day frequency (MSDF), the presence of cluster seizures during a retrospective 2-month period with a prospective follow-up of 6 months, and the overall responder rate. Twenty-seven dogs were included in the study, 14 dogs in the phenobarbital group and 13 dogs in the KBr group. Both median MSF and MSDF decreased in the phenobarbital group (both P=0.001) and in the KBr group (P=0.004 and P=0.003, respectively). Overall, the number of dogs with cluster seizures decreased (P=0.0005). The responder rate was 79% vs. 69% in the phenobarbital and KBr groups, respectively. We conclude that phenobarbital or KBr add-on treatment decreases median MSF and MSDF in epileptic dogs refractory to a maximum dose of imepitoin. Combination therapy was generally well tolerated and resulted in an improvement in seizure management in the majority of the dogs.
Epileptic Seizures Versus Syncope: Pathophysiology and Clinical Approach. Marios Charalambous, Sergio A. Gomes, Stella Papageorgiou, Massimo Orioles. Vet. Evid. February 2017;2(1). Quote: Generalised epileptic seizures and syncope are two syndromes with similar clinical manifestation and their differentiation can be quite challenging. The aim of this review is to use an evidence-based approach in differentiating these two syndromes through the comprehension of the pathophysiological mechanisms involved and their clinical signs. Both syndromes affect regions of the forebrain and consciousness level, although, different mechanisms are involved. Syncope is a paroxysmal event secondary to a short-term decrease in cerebral perfusion, oxygenation or essential nutrients delivery. Generalised epileptic seizure activity is defined as the clinical manifestation of transient paroxysmal disturbances in brain function secondary to an imbalance between excitatory and inhibitory neurotransmitters. Clinical criteria, including precipitating events, clinical signs preceding, during and following the episodes and event duration, can be used to differentiate the two syndromes. Although these criteria might be useful for the practitioner, definite conclusions should be precluded due to the lack of original research articles and weak evidence on this specific field.
Langford Vets perform cutting-edge canine epilepsy procedure. Thomas Harcourt-Brown. Langford Vets. February 2017. Quote: Vagus Nerve Stimulators (VNS) are pacemaker type devices that are commonly implanted in children with medically unresponsive seizures and when other epilepsy surgery procedures aren’t suitable. The Paediatric Epilepsy Surgery centre at BRHC implants around thirty of these devices into epileptic children every year. Research work has demonstrated that the technique is effective in other mammals including dogs, although this is the first procedure of its type to be undertaken in the UK. Epilepsy is a very common disorder in dogs and can be very difficult and very expensive to treat medically. For this reason many beloved family pets end up being put down when they fail to respond to drugs. Although VNS is rarely curative of epilepsy in humans or dogs, we are very hopeful that that surgery will be effective in helping control Jago’s fits. In recent months his seizures have become so frequent that he has had difficulty in walking and eating. His device will need regular programming over the next few months to get to optimum settings. If it proves effective, it may be possible to reduce the amount of anti-seizure medications he has to take. Its early days yet but this treatment might offer hope for other families with epileptic dogs.
Physiological reactivity to spontaneously occurring seizure activity in dogs with epilepsy and their carers. R.M.A. Packer, H.A. Volk, R.C. Fowkes. Physiology & Behavior. April 2017. Quote: Highlights: • Seizure activity is potentially stress-inducing for dogs with epilepsy and their carers. • This study examined HPA reactivity following spontaneous seizure activity in dogs. • Salivary cortisol levels increased in dogs and carers following seizure activity. • Carers with higher neuroticism scores exhibited higher cortisol levels. • No associations were found between cortisol reactivity and the dog-carer bond. There is a complex bidirectional relationship between stress and epilepsy. Stressful stimuli and subsequent cortisol release act as a trigger for seizure activity in some individuals with epilepsy, and seizure activity itself may act as a stressor to the affected individual. Epilepsy is the most common chronic neurological condition in domestic dogs and requires chronic management by their human carers, impacting upon the quality of life of both dog and carer. Seizures occur unpredictably and may be stressful for carers to witness and manage. In the present study we investigated the role of seizure activity as a stressor, measuring the effect of spontaneously occurring seizure activity in dogs with epilepsy upon their own cortisol levels and that of their carers. Furthermore, we tested whether individual differences in HPA reactivity were associated with owner personality characteristics and the quality of the dog–carer relationship. Saliva samples were obtained from sixteen dog-carer dyads in the home setting 20 and 40 minute post-seizure, and at time-matched points on the following (non-seizure) day. Significant differences in cortisol levels were found in dogs at 40 minute post-seizure (265.1% increase), and at 20 minute post-seizure in their carers (40.5% increase). No associations were found between cortisol reactivity and the strength of the dog-carer bond. Carers with higher neuroticism scores exhibited higher cortisol levels at both post-seizure sampling points. As there was a gender bias in the carer sample (15/16 were female), and there are known sex differences in cortisol reactivity in response to psychological stress, the conclusions of this study may be limited to female carers. These findings are the first to objectively demonstrate the acutely stressful effects of seizures in dogs with epilepsy and their carers.
Serum cardiac troponin I concentrations in dogs with generalised seizures. E. Dutton, N. Carmichael, U. Michal, P. J. Cripps, A. Boswood. J. Sm. Anim. Pract. October 2017. Quote: Objectives: To determine if serum cardiac troponin I concentrations – measured with both a first-generation assay and a high-sensitivity assay – were greater in dogs with generalised seizures than in controls and to identify clinical variables associated with cardiac troponin I concentration. Materials & Methods: Prospective study of 30 dogs with recent generalised seizures [including 2 cavalier King Charles spaniels] and 30 healthy controls [including 1 cavalier]. Serum cardiac troponin I concentration was measured using two commercially available assays, and the correlation of clinical factors with concentration was examined. Results: Serum concentrations of cardiac troponin I were higher in dogs that had recent seizures compared to controls when measured by both assays. The predictors most clearly associated with cardiac troponin I concentration were number of seizures and age. Both predictors were positively associated with increasing concentrations of troponin I. Clinical Significance: Serum cardiac troponin I concentration was significantly elevated in dogs that had recent generalised seizures when compared to controls, and concentrations were higher in dogs that experienced more seizures. This association may indicate that generalised seizures are associated with damage to the myocardium.
Cognitive dysfunction in naturally occurring canine idiopathic epilepsy. Rowena M. A. Packer, Paul D. McGreevy, Hannah E. Salvin, Michael J. Valenzuela, Chloe M. Chaplin, Holger A. Volk. PlosOne. February 2018;13(2):e0192182. Quote: Globally, epilepsy is a common serious brain disorder. In addition to seizure activity, epilepsy is associated with cognitive impairments including static cognitive impairments present at onset, progressive seizure-induced impairments and co-morbid dementia. Epilepsy occurs naturally in domestic dogs but its impact on canine cognition has yet to be studied, despite canine cognitive dysfunction (CCD) recognised as a spontaneous model of dementia. Here we use data from a psychometrically validated tool, the canine cognitive dysfunction rating (CCDR) scale, to compare cognitive dysfunction in dogs diagnosed with idiopathic epilepsy (IE) with controls while accounting for age. An online cross-sectional study resulted in a sample of 4051 dogs [... There were 173 different breeds represented, the top three being the Border Collie (9.2%, n = 371), Cavalier King Charles Spaniel (6.5%, n = 265) and Labrador Retriever (6.1%, n = 248). ...], of which n = 286 [6 CKCSs] had been diagnosed with IE. Four factors were significantly associated with a diagnosis of CCD (above the diagnostic cut-off of CCDR ≥50): (i) epilepsy diagnosis: dogs with epilepsy were at higher risk; (ii) age: older dogs were at higher risk; (iii) weight: lighter dogs (kg) were at higher risk; (iv) training history: dogs with more exposure to training activities were at lower risk. Impairments in memory were most common in dogs with IE, but progression of impairments was not observed compared to controls. A significant interaction between epilepsy and age was identified, with IE dogs exhibiting a higher risk of CCD at a young age, while control dogs followed the expected pattern of low-risk throughout middle age, with risk increasing exponentially in geriatric years. Within the IE sub-population, dogs with a history of cluster seizures and high seizure frequency had higher CCDR scores. The age of onset, nature and progression of cognitive impairment in the current IE dogs appear divergent from those classically seen in CCD. Longitudinal monitoring of cognitive function from seizure onset is required to further characterise these impairments.
Negative effects of epilepsy and antiepileptic drugs on the trainability of dogs with naturally occurring idiopathic epilepsy. Rowena M.A. Packer, Paul D. McGreevy, Amy Pergande, Holger A. Volk. Applied Animal Behaviour Science. March 2018. DOI: 10.1016/j.applanim.2017.11.008 Quote: Highlights: • Epilepsy and antiepileptic drugs (AEDs) induce cognitive deficits in humans. • We studied the impact of epilepsy on trainability in adult dogs. • Dogs with epilepsy exhibited significantly lower trainability than controls. • Trainability of dogs treated with polytherapy and specific AEDs showed the most impairment. • History of training and use of reward-based methods increased trainability. -- Epilepsy and anti-epileptic drug (AED) treatment have been found to induce or exacerbate underlying cognitive impairments in people, affecting learning ability, attention and memory. Idiopathic epilepsy (IE) is the most common chronic neurological condition in dogs. Whether IE impairs cognition, which may be reflected in affected dogs’ trainability, has not been explored. The aim of this study was to investigate whether IE and/or AED treatment compromise the trainability of dogs with IE compared to controls. An online cross-sectional study was conducted, resulting in a sample of 4051 dogs [There were 173 different breeds represented, the top three being the Border Collie (9.2%, n=371), Cavalier King Charles Spaniel (6.5%, n=265) and Labrador Retriever (6.1%, n=248).], of which 286 had been diagnosed with IE. Owners reported their dog’s trainability using a previously validated research questionnaire, along with their dogs’ training history (type of activities and training methods used) and clinical history. Four factors were significantly associated with trainability in a generalised linear mixed model: (i) epilepsy diagnosis: dogs with IE had significantly lower trainability than controls; (ii) age: dogs aged >12 years had significantly lower trainability than all other age groups; (iii) adult training history score: dogs with greater exposure to training activities were more trainable; and (iv) training method: dogs whose owners used a mix of both reward and punishment-based methods had lower trainability than those using solely reward-based methods. Within the sub-population of dogs with IE, those treated with (i) polytherapy (2–3 AEDs), (ii) zonisamide and/or (iii) potassium bromide exhibited lower trainability. This study provides initial evidence of cognitive impairment associated with IE and treatments for it, as measured by a metric of trainability. Further study is required to characterise these deficits. However, if these effects are confirmed, the merits of using the dog as a model of spontaneously occurring epilepsy will be strengthened, further consideration of the effects of AEDs will be required, and strategies to enhance cognition in affected dogs should be explored.
Preliminary assessment of cognitive impairments in canine idiopathic epilepsy. Joshua Winter, Rowena Mary Anne Packer, Holger Andreas Volk. Vet. Rec. April 2018. DOI:10.1136/vr.104603. Quote: In humans, epilepsy can induce or accelerate cognitive impairment (CI). There is emerging evidence of CI in dogs with idiopathic epilepsy (IE) from recent epidemiological studies. The aim of our study was to assess CI in dogs with IE using two tests of cognitive dysfunction designed for use in a clinical setting. Dogs with IE (n=17) were compared against controls (n=18) in their performance in two tasks; a spatial [meaning, related to space or area] working memory task and a problem-solving task. ... The food searching task aims to test the dog’s spatial working memory, assessing ability to search and find a food reward (ham), the location of which had previously been indicated to them through vocalisation and pointing to the reward. ... The problem-solving task aims to test the dog’s problem-solving ability to access a hidden food reward. To access the food, the dog must manipulate an object (a transparent plastic box) that acts as a barrier to the reward. ... In addition, owners completed the Canine Cognitive Dysfunction Rating (CCDR) scale for their dog. The groups did not differ statistically with respect to age and breed. Dogs with IE performed significantly worse than controls on the spatial working memory task (P=0.016), but not on the problem solving task (P=0.683). CCDR scores were significantly higher in the IE group (P=0.016); however, no dogs reach the recommended threshold score for CCD diagnosis. Our preliminary data suggest that dogs with IE exhibit impairments in a spatial working memory task. Further research is required to explore the effect of IE on other cognitive abilities in dogs with a larger sample, characterising the age of onset, nature and progression of any impairments and the impact of anti-epileptic drugs.
Efficiency of Levetiracetam and Gabapentin in the treatment of Epilepsy in a Cavalier King Charles Spaniel Dog with Myxomatous Mitral Valve Heart Disease, a Case Report. Sinan Kandır, Cengiz Yüce Kayabek, Bilge Kaan Tekelioğlu. 3d Int'l Mediterranean Sci. & Engr'g Conf. October 2018. Pgs. 1242-1245;paper ID456. Quote: Epilepsy and seizure have a complex physiopathological background and are most common idiopathic or primary neurologic disorders in dogs. Various anticonvulsant (ACDs) and antiepileptic drugs (AEDs) are used for the management of seizures and epilepsy. The use of levetiracetam is limited in the treatment of epilepsy and is used only with expert opinion because of its undesirable side effects and its low therapeutic effect, which are not chemically related to existing AEDs. The Cavalier King Charles Spaniels (CKCSs) are predisposed to numerous inherited neurologic and cardiologic problems due to their high predisposition to genetic pool originated consanguineous diseases. The dog was 3 years old, female, CKCSs breed stud and had been suffered from epileptic seizures almost 3 months. The dog was consulted at Veterinary Faulty Clinics and myxomatous mitral valve heart disease (MMVD) was diagnosed. Phenobarbital (2.5 mg/kg BID, PO) and enalapril (0.5 mg/kg BID, PO) were prescripted for the management of epileptic seizures and medication of the MMVD. However, the dog wasn’t reacted the treatment as expected and epileptic seizures were increased dramatically (~7 times per day) in addition with respiratory depression. The treatment protocol was changed to levetiracetam (15 mg/kg BID, PO). The dog was reacted well to levetiracetam treatment and epileptic seizures were disappeared with respiratory depression. Three months later a routine parasitic treatment was done with fipronil (0.067 ml/kg, spot-on). The epileptic attacks were dramatically increased and became more severe just after the fipronil treatment (~7 times per day). Thus, gabapentin (10 mg/kg, TID, PO) was decided to use together with levetiracetam (10 mg/kg BID, PO). Epileptic seizures disappeared with the use of gabapentin over again. In conclusion, the pharmacokinetics and antiepileptic effects of levetiracetam and gabapentin are not fully understood, but the combination of both drugs with a combined drug protocol may help to manage epileptic attacks without causing respiratory depression in CKCS. Fipronil, phenylpyrazole origin and other antiparasitic drugs should be used very carefully and under veterinary consultant supervision due to their side effects especially in epileptic dogs. Finally, gabapentin could be a good option for the alternative add-on therapy to control epileptic seizures in CKCSs.
Randomized blinded controlled clinical trial to assess the effect of oral cannabidiol administration in addition to conventional antiepileptic treatment on seizure frequency in dogs with intractable idiopathic epilepsy. Stephanie McGrath, Lisa R. Bartner, Sangeeta Rao, Rebecca A. Packer, Daniel L. Gustafson. J. Am. Vet. Med. Assn. June 2019; doi: 10.2460/javma.254.11.1301. Quote: Objective: To assess the effect of oral cannabidiol (CBD) administration in addition to conventional antiepileptic treatment on seizure frequency in dogs with idiopathic epilepsy. Design: Randomized blinded controlled clinical trial. Animals: 26 client-owned dogs with intractable idiopathic epilepsy [none being cavalier King Charles spaniels]. Procedures: Dogs were randomly assigned to a CBD (n = 12) or placebo (14) group. The CBD group received CBD-infused oil (2.5 mg/kg [1.1 mg/lb], PO) twice daily for 12 weeks in addition to existing antiepileptic treatments, and the placebo group received noninfused oil under the same conditions. Seizure activity, adverse effects, and plasma CBD concentrations were compared between groups. Results: 2 dogs in the CBD group developed ataxia and were withdrawn from the study. After other exclusions, 9 dogs in the CBD group and 7 in the placebo group were included in the analysis. Dogs in the CBD group had a significant (median change, 33%) reduction in seizure frequency, compared with the placebo group. However, the proportion of dogs considered responders to treatment (≥ 50% decrease in seizure activity) was similar between groups. Plasma CBD concentrations were correlated with reduction in seizure frequency. Dogs in the CBD group had a significant increase in serum alkaline phosphatase activity. ... Serum ALP activity increased significantly from weeks 0 to 12 in dogs in the CBD group, compared with activity in dogs in the placebo group. This increase, observed in all 9 dogs in the CBD group, was likely due to the induction of CYP isoenzymes in the liver. ... This inhibition may be linked to adverse effects from coadministration of common AEDs, such as potentiation of benzodiazepines and phenobarbital. Thus, although the clinical importance of the increase in serum ALP activity observed in the present study remains unknown, other considerations involving drug interactions are of importance. No measurement of serum bile acids concentrations was performed, which would have helped elucidate whether any functional changes to the liver had occurred after 12 weeks of CBD treatment. ... No adverse behavioral effects were reported by owners. ... A limitation of the study reported here was the small sample size, which made the clinical importance of the observed data difficult to interpret. Given the results, a larger randomized blinded controlled clinical trial involving a higher dose of CBD is warranted. Another limitation inherent to clinical trials involving dogs with epilepsy is the reliance on dog owners for recording outcomes such as seizure frequency. Some seizures could have been missed if they were nocturnal or the owner was absent; however, because owners were unaware of which treatment their dogs received, there was no reason to believe that any bias introduced by misclassification of seizure frequency would be different between treatment groups. ... Conclusions & Clinical Relevance: Although a significant reduction in seizure frequency was achieved for dogs in the CBD group, the proportion of responders was similar between groups. Given the correlation between plasma CBD concentration and seizure frequency, additional research is warranted to determine whether a higher dosage of CBD would be effective in reducing seizure activity by ≥ 50%.
Behavioural changes in dogs with idiopathic epilepsy. Fraje Watson, Rowena Mary Anne Packer, Clare Rusbridge, Holger Andreas Volk. Vet. Rec. January 2020; doi: 10.1136/vr.105222. Quote: Background: Breed-specific and broader cohort studies have shown behavioural changes in dogs following the onset of idiopathic epilepsy (IE). Methods: A cross-sectional, case–control questionnaire study was carried out to strengthen this body of evidence. Owners of eight breeds of dog completed an online questionnaire about their dogs’ behaviour; once for control dogs and twice for dogs with IE, for both pre-IE and post-IE onset behaviour. Results: Ninety-six (24.74 per cent) dogs with IE and 292 (75.26 per cent) age and breed-matched control dogs met the inclusion criteria. Control dogs had significantly higher ‘Trainability’ scores than dogs with IE (P=0.04). After IE, dogs had significantly higher ‘Dog-Directed Fear or Aggression’ (P=0.02), ‘Non-Social Fear’ (P=0.01), ‘Attachment/Attention-Seeking Behaviour’ (P=0.04), ‘Attention-Deficit’ (P=0.02) and significantly lower ‘Trainability’ (P=0.02) than prior to the onset of IE. Medication status did not significantly affect any behavioural factor, but drug-resistant dogs had significantly less ‘Trainability’ than drug-responsive (P=0.04) and partially drug-responsive dogs (P=0.03). Conclusion: Behavioural differences related to cognitive function are seen between dogs with IE and controls. Behavioural changes related to anxiety, attention and cognition are seen in dogs following the onset of IE. The ability to clinically define and diagnose behavioural comorbidities in dogs is much needed from both a clinical and research perspective.
Multiple subpial transection as epilepsy surgery in two dogs with long-term (7 years) follow-up. M. Saito1, K. Mori1, M. Yokomori1, J. Hirashima. J. Vet. Intern. Med. October 2020;34(6)[P93]:3043-3044. Quote: Surgical treatment of epilepsy is underdeveloped in veterinary medicine. Multiple subpial transection (MST) is a disconnective epilepsy surgery, stopping the seizure activity, while preserving the function of the eloquent cortex by sectioning the intracortical horizontal fiber of the epileptogenic zone. This preliminary study aimed to assess the feasibility and clinical benefits of MST in epileptic dogs using prospective long-term observation. Two laboratory dogs with idiopathic epilepsy (Tier III, 1.5 T magnetic resonance imaging [MRI] without cerebrospinal fluid analysis) with frontal lobe focus consistently identified by multiple scalp electroencephalograms (EEG) were included. Both dogs had been abandoned from other facilities because of unmanageable convulsive seizures. A transection hook was designed for each dog with the length of the tip paralleling the frontal lobe cortical thickness determined by MRI. After rostrotentorial craniotomy, electrocorticography (ECoG) was recorded in multiple points around the frontal lobe and MST was performed in the gyrus where epileptic discharges (ED) were recorded in ECoG. ECoG was repeated, and MST was performed until ED almost disappeared. Intermittent observations, and serial physical, neurological, and EEG examinations were performed postoperatively. The study was approved by the Institutional Research Committee. Both dogs were followed-up for 7 years and showed no neurological abnormalities, except that one dog had transient hind-limb ataxia for 2 postoperative weeks and one seizure episode on postoperative day 1. ED was observed less frequently and not in the area where MST was performed a 27 months postoperatively. This study suggested that MST may be a treatment option for epileptic dogs.
Repetitive transcranial magnetic stimulation in drug-resistant idiopathic epilepsy of dogs: A noninvasive neurostimulation technique. Marios Charalambous, Luc Van Ham, Bart J. G. Broeckx, om Roggeman, Sofie Carrette, Kristi Vonck, Roelof R. Kervel, Ine Cornelis, Sofie F. M. Bhatti. J. Vet. Intern. Med. October 2020; doi: 10.1111/jvim.15919. Quote: Background: Although repetitive transcranial magnetic stimulation (rTMS) has been assessed in epileptic humans, clinical trials in epileptic dogs can provide additional insight. Objectives: Evaluate the potential antiepileptic effect of rTMS in dogs. Animals: Twelve client-owned dogs with drug-resistant idiopathic epilepsy (IE). Methods: Single-blinded randomized sham-controlled clinical trial (dogs allocated to active or sham rTMS) (I) and open-labeled uncontrolled clinical trial (dogs received active rTMS after sham rTMS) (II). Monthly seizure frequency (MSF), monthly seizure day frequency (MSDF), and number of cluster seizures (CS) were evaluated for a 3-month pre-TMS and post-rTMS period and safety was assessed. The lasting effect period of rTMS was assessed in each dog treated by active stimulation using the MSF ratio (proportion of post-TMS to pre-rTMS MSF) and treatment was considered effective if the ratio was <1. Results: No adverse effects were reported. In trial I, MSF and MSDF decreased significantly in the active group (n = 7). In the sham group (n = 5), no significant changes were found. Cluster seizures did not change significantly in either group. No significant differences were detected between the groups. In trial II, previously sham-treated dogs (n = 5) received active rTMS and significant decreases in MSF and MSDF were noted. The overall effect of rTMS lasted for 4 months; thereafter, the MSF ratio was >1. Conclusions and Clinical Importance: Repetitive transcranial magnetic stimulation may be a safe adjunctive treatment option for dogs with drug-resistant IE, but large-scale studies are needed to establish firm conclusions.
Medium-chain triglycerides dietary supplement improves cognitive abilities in canine epilepsy. Benjamin Andreas Berk, Rowena Mary Anne Packer, Tsz Hong Law, Annette Wessmann, Andrea Bathen-Nöthen, Tarja Susanna Jokinen, Anna Knebel, Andrea Tipold, Ludovic Pelligand, Holger Andreas Volk. Epilepsy & Behav. November 2020; doi: 10.1016/j.yebeh.2020.107608. Quote: Highlights: • Consumption of MCT oil improves the cognitive abilities in canine epilepsy. • MCT oil as 9% of total caloric intake improved spatial-working memory and problem-solving skills. • Dietary consumption of MCT increases BHB serum concentration. • Postprandial BHB serum concentration correlates with improvement in the problem-solving task. Objective: Cognitive impairments (CI) have recently been identified in canine epilepsy patients. A medium-chain triglyceride (MCT) enriched diet has been demonstrated to improve cognition in aged dogs and seizure control in canine epilepsy. This study evaluates the short-term effects of MCT-oil consumption on cognitive abilities in dogs with epilepsy, a naturally occurring animal model. Methods: A 6-month multicenter, prospective, randomized, double-blinded, controlled cross-over diet trial was conducted comparing dietary supplementation (DS) of MCT oil to a control oil. Allocation to dietary oil supplements, consisting of 9% total caloric intake, was block-randomized and supplemented into each dogs’ diet for 3 months followed by a respective switch of DS-oil for a further 3 months. Noninvasive cognitive tests and a validated psychometric tool were utilized to evaluate cognitive function and perturbations associated with dietary intervention. Results: Twenty-nine dogs completed the trial, of which 18 completed noninvasive cognitive testing. Spatial-working memory, problem-solving ability, and owner-reported trainability were significantly improved during MCT-oil supplementation compared to control-DS. Significance: MCT-oil DS improves cognition in dogs with epilepsy when compared to a control-DS. MCT supplementation may represent a promising option to address CI associated with epilepsy.
Dietary medium chain triglycerides for management of epilepsy: New data from human, dog, and rodent studies. Felicity Y. Han, Lisa Conboy-Schmidt, Galena Rybachuk, Holger A. Volk, Brian Zanghi, Yuanlong Pan, Karin Borges. Epilepsia. June 2021; doi: 10.1111/epi.16972. Quote: Many studies show that glucose metabolism in epileptic brain areas can be impaired. Energy is crucial to maintain normal brain function, including ion and neurotransmitter balances. Energy deficits can lead to disruption of ion gradients, which can trigger neuronal depolarization and generation of seizures. Thus, perturbed metabolic processing of glucose in epileptogenic brain areas indicates a specific nutritional need for people and animals with epilepsy, as they are likely to benefit from auxiliary brain fuels other than glucose. Ketogenic diets provide the ketone bodies acetoacetate and β-hydroxybutyrate, which can be used as auxiliary fuel by the brain. ... In dogs, specific breeds in certain countries have shown very high prevalence of epilepsy. [Belgian shepherds, Irish wolfhounds, pugs, boxers, basset hounds, border terriers, border collies] ... The onset of epilepsy typically occurs in the first few years of life. In addition to epileptic seizures, dogs with epilepsy show behaviors similar to anxiety and attention-deficit/hyperactivity disorder in humans, as well as cognitive impairments. ... To date, several efficacy studies in dogs with idiopathic epilepsy fed with 5.5%–6.5% added MCT oil (wt/wt) or MCT oil providing 9% of daily metabolic energy requirement have been published. ... The magnitudes of the anticonvulsant effects in dogs associated with dietary MCT supplementation published are very similar to successful new ASDs in large human Phase III efficacy trials, where new drugs are tested in 200–600 patients with drug-resistant epilepsy as add-on treatment. In these trials, approximately 30%–50% of people experienced greater than 50% reduction in seizures when treatments were deemed efficacious, and the placebo showed efficacy in 10%–26% of people. On average, seizure frequencies were reduced by 26% with efficacious drugs and 13% with placebo. Taken together, these studies provide accumulating evidence of the efficacy of MCTs as an adjunct for the management of epilepsy in dogs. ... Based on the available studies, it is still unclear which MCT formulations are ideal to prevent seizure generation in people and in dogs. However, decanoic acid and MCTs containing this MCFA seem to play an important role and were more efficacious in in vitro and in vivo rodent models.
Case Report: Embedding “Digital Chronotherapy” Into Medical Devices—A Canine Validation for Controlling Status Epilepticus Through Multi-Scale Rhythmic Brain Stimulation. Mayela Zamora, Sebastian Meller, Filip Kajin, James J. Sermon, Robert Toth, Moaad Benjaber, Derk-Jan Dijk, Rafal Bogacz, Gregory A. Worrell, Antonio Valentin, Benoit Duchet, Holger A. Volk, Timothy Denison. Front. Neurosci. September 2021; doi: 10.3389/fnins.2021.734265. Quote: Circadian and other physiological rhythms play a key role in both normal homeostasis and disease processes. Such is the case of circadian and infradian seizure patterns observed in epilepsy. However, these rhythms are not fully exploited in the design of active implantable medical devices. In this paper we explore a new implantable stimulator that implements chronotherapy as a feedforward input to supplement both open-loop and closed-loop methods. This integrated algorithm allows for stimulation to be adjusted to the ultradian, circadian and infradian patterns observed in patients through slowly-varying temporal adjustments of stimulation and algorithm sub-components, while also enabling adaption of stimulation based on immediate physiological needs such as a breakthrough seizure or change of posture. Embedded physiological sensors in the stimulator can be used to refine the baseline stimulation circadian pattern as a “digital zeitgeber,” i.e., a source of stimulus that entrains or synchronizes the subject's natural rhythms. This algorithmic approach is tested on a canine with severe drug-resistant idiopathic generalized epilepsy exhibiting a characteristic diurnal pattern correlated with sleep-wake cycles. Prior to implantation, the canine's cluster seizures evolved to status epilepticus (SE) and required emergency pharmacological intervention. The cranially-mounted system was fully-implanted bilaterally into the centromedian nucleus of the thalamus. Using combinations of time-based modulation, thalamocortical rhythm-specific tuning of frequency parameters as well as fast-adaptive modes based on activity, the canine experienced no further SE events post-implant as of the time of writing (7 months). Importantly, no significant cluster seizures have been observed either, allowing the reduction of rescue medication. The use of digitally-enabled chronotherapy as a feedforward signal to augment adaptive neurostimulators could prove a useful algorithmic method in conditions where sensitivity to temporal patterns are characteristics of the disease state, providing a novel mechanism for tailoring a more patient-specific therapy approach.
Corpus Callosotomy in 3 Cavalier King Charles Spaniel Dogs with Drug-Resistant Epilepsy. Rikako Asada, Satoshi Mizuno, Yoshihiko Yu, Yuji Hamamoto, Tetsuya Anazawa, Daisuke Ito, Masato Kitagawa, Daisuke Hasegawa. Brain Sci. November 2021; doi: 10.3390/brainsci11111462. Quote: Corpus callosotomy (CC) is an established palliative surgery for human patients with drug-resistant epilepsy (DRE), especially those with generalized seizures and multiple or unknown epileptogenic focus. However, there are no reports to describe CC in canine patients with epilepsy. Three client-owned Cavalier King Charles Spaniels with DRE are included in this case series. In presurgical evaluations, an apparent epileptogenic zone was not detected in each dog and CC was conducted. Total CC was performed in one dog, whereas the other two received partial CC. One dog recovered from surgery without any complications, but died suddenly by an unknown cause at 10 h after surgery. For the other two dogs, postoperative evaluations including seizure outcomes, complications, and quality of life of the dogs and owners were assessed for at least 12 months. Both dogs showed a remarkable decrease in seizure frequency (averaged 80.3% reduction) and severity after surgery. The antiseizure medications were maintained, and not only the mentation and activity of the dogs, but also the quality of life of dogs and owners were improved postoperatively. Although technical improvement and more large-scale studies are needed, CC is a treatment option for dogs with DRE in veterinary medicine.
Mimicking focal epileptic seizures-episodic pain due to a facial foreign body in a puppy: Imaging characteristics and treatment. Andrea De Bonis, Oliver Marsh, Fabio Stabile.Vet Record. December 2021; doi: 10.1002/vrc2.255. Quote: A 4-month-old female entire Cavalier King Charles Spaniel was referred for investigation into a 3-week history of suspected focal onset seizures, characterised by head nodding and eyelid twitching. An inflammatory soft-tissue reaction surrounding a suspected foreign body (FB) in the subcutaneous tissue and muscles at the level of the left maxilla in the caudal aspect of the left maxillary second molar was detected using MRI. The presence of the FB was confirmed ultrasonographically. This was found to be a grass seed upon surgical removal. The previously reported clinical signs resolved immediately after the surgery. It was suspected that the FB and secondary inflammatory reaction incited a form of trigeminal neuralgia manifesting as paroxysmal head nodding and facial twitching. A form of trigeminal neuralgia should be included in the differential diagnosis of facial focal motor seizures and should be investigated accordingly before initiating any antiepileptic treatment.
Neurostimulation as a Method of Treatment and a Preventive Measure in Canine Drug-Resistant Epilepsy: Current State and Future Prospects. Marta Nowakowska, Muammer Üçal, Marios Charalambous, Sofie F. M. Bhatti, Timothy Denison, Sebastian Meller, Gregory A. Worrell, Heidrun Potschka, Holger A. Volk. Front. Vet. Sci. June 2022; doi: 10.3389/fvets.2022.889561. Quote: Modulation of neuronal activity for seizure control using various methods of neurostimulation is a rapidly developing field in epileptology, especially in treatment of refractory epilepsy. Promising results in human clinical practice, such as diminished seizure burden, reduced incidence of sudden unexplained death in epilepsy, and improved quality of life has brought neurostimulation into the focus of veterinary medicine as a therapeutic option. This article provides a comprehensive review of available neurostimulation methods for seizure management in drug-resistant epilepsy in canine patients. ... Canine patients with epilepsy have been included in clinical research involving three brain stimulation methods: VNS [vagus nerve stimulation], DBS [deep brain stimulation], and TMS [transcranial magnetic stimulation]. ... Neurostimulation exerts effects on nervous tissue at cellular, molecular and structural levels. Mathematical modeling of high frequency stimulation in neural networks revealed its stabilizing influence on cells. Neural circuits showed reduced susceptibility to sudden transitions into oscillations usually marking the onset of a seizure. Moreover, inhibitory cells were recruited more strongly than excitatory cells, putting the system in an “anti-seizure state”. This mechanism may be the basis for acute seizure termination after application of high frequency stimulation. Brain stimulation also led to changes in connectivity of the brain inside and outside of epileptic foci and different protocols led to promotion or suppression of circuit synchronicity. Stimulation of neural tissue alters not only its electrical properties but also its chemical microenvironment. ... Recent progress in non-invasive modalities, such as repetitive transcranial magnetic stimulation and transcutaneous vagus nerve stimulation is highlighted. We further discuss potential future advances and their plausible application as means for preventing epileptogenesis in dogs.
Neurosurgery in canine epilepsy. Daisuke Hasegawa, Miyoko Saito, Masato Kitagawa. Vet. J. July 2022; doi: 10.1016/j.tvjl.2022.105852. Quote: Epilepsy surgery is functional neurosurgery applied to drug-resistant epilepsy. Although epilepsy surgery has been established and achieves fair to good outcomes in human medicine, it is still an underdeveloped area in veterinary medicine. With the spread of advanced imaging and neurosurgical modalities, intracranial surgery has become commonplace in the veterinary field, and, therefore, it is natural that expectations for epilepsy surgery increase. This review summarizes current standards of intracranial epilepsy surgery in human medicine and describes its current status and expectation in veterinary medicine. Intracranial epilepsy surgery is classified generally into resection surgery, represented by cortical resection, lobectomy, and lesionectomy, and disconnection surgery, such as corpus callosotomy and multiple subpial transection. In dogs with drug-resistant epilepsy, corpus callosotomy is available as a disconnection surgery for generalized epilepsy. However, other types of disconnection and resection surgeries for focal epilepsy are limited to experimental studies in laboratory dogs and/or anecdotal case reports of lesionectomy, such as tumor or encephalocele removal, without epileptogenic evidence. Veterinary epilepsy surgery is a new and challenging neurosurgery field; with the development of presurgical evaluations such as advanced electroencephalography and neuroimaging, it may become more readily practiced. Highlights: Epilepsy surgery (ES) is established in humans, but not in dogs and cats. ES is divided into resection (RS), disconnection (DS), and neurostimulation. RS includes cortical resection, gyrectomy, lobectomy, and lesionectomy. DS includes corpus callosotomy and multiple subpial transection. Presurgical evaluations and strategy are important for successful ES in dogs. ... Conclusions: This review describes the current status of epilepsy surgery in veterinary medicine, especially in dogs. All techniques, including presurgical evaluations, surgical procedures, and evidence of efficacy are immature, as we are just at the starting point of veterinary epilepsy surgery. Whether idiopathic (non-lesional) or structural (lesional), looking from the perspective of epilepsy surgery (i.e., semiology, electrodiagnostic, imaging, and expected outcome) is most important for future development of epilepsy surgery procedures. In human medicine, epilepsy surgery is not currently considered the final resort and is also performed as one of the early treatment options for epidemiologically intractable epilepsy syndromes. To establish and universalize epilepsy surgery in veterinary medicine, further research and education on all aspects of canine epilepsy, as well as surgical techniques are essential. The authors hope that this review will be the catalyst for advancing this new era of veterinary epileptology and neurosurgery.
Case Report: Anti-GABAA Receptor Encephalitis in a Dog. Enrice I. Huenerfauth, Christian G. Bien, Corinna Bien, Holger A. Volk, Nina Meyerhoff. Front.Vet. Sci. June 2022; doi: 10.3389/fvets.2022.886711. Quote: Autoantibodies against neurotransmitter receptors detected in cerebrospinal fluid (CSF) and serum are increasingly recognized in people with human autoimmune encephalitis causing severe neurological deficits, such as seizures and behavioral abnormalities. This case report describes the first encephalitis associated with antibodies against the γ-aminobutyric acid-A receptor (GABAAR) in a dog. A young male intact Cavalier King Charles Spaniel was presented with recent onset of initial multiple generalized tonic-clonic seizures progressing into a status epilepticus. Interictally, he showed alternating stupor and hyperexcitability, ataxia, pleurothotonus and circling behavior to the left side. Magnetic resonance imaging (MRI) of the brain showed breed-specific anatomical abnormalities. Standard CSF analysis was unremarkable. Despite treatment with multiple antiseizure medications (ASMs) seizures and behavior abnormalities sustained. Immunotherapy with dexamethasone was started on the fifth day after disease manifestation. This led to rapid improvement of clinical signs. An extensive antibody search in CSF and serum demonstrated a neuropil staining pattern on a tissue-based assay compatible with GABAAR antibodies. The diagnosis was confirmed by binding of serum and CSF antibodies to GABAAR transfected Human Embryonic Kidney cells. The serum titer was 1:320, the CSF titer 1:2. At the control visit 4.5 weeks after start of immunotherapy, the dog was clinically normal. The GABAAR antibody titer in serum had strongly decreased. The antibodies were no longer detectable in CSF. Based on clinical presentation and testing for GABAAR binding antibodies, this describes the first veterinary patient with an anti-GABAAR encephalitis with a good outcome following ASM and corticosteroid treatment.
Safety and efficacy of cannabidiol-cannabidiolic acid rich hemp extract in the treatment of refractory epileptic seizures in dogs. Gabriel A. Garcia1, Stephanie Kube, Sheila Carrera-Justiz, David Tittle, Joseph J. Wakshlag. Front. Vet. Sci. July 2022; doi: 10.3389/fvets.2022.939966. Quote: The use of cannabidiol (CBD) in childhood refractory seizures has become a common therapeutic approach for specific seizure disorders in human medicine. Similarly, there is an interest in using CBD, cannabidiolic acid (CBDA) or cannabinoid-rich hemp products in the treatment of idiopathic epilepsy in dogs. We aimed to examine a small cohort in a pilot investigation using a CBD and CBDA-rich hemp product for the treatment of refractory epileptic seizures in dogs. Fourteen dogs were examined in a 24-week randomized cross-over study being provided placebo or CBD/CBDA-rich hemp extract treatment at 2 mg/kg orally every 12 h for each 12-week arm of the study. Serum chemistry, complete blood counts, serum anti-seizure medication (ASM) concentrations and epileptic seizure frequency were followed over both arms of the cross-over trial. Results demonstrated that besides a mild increase in alkaline phosphatase, there were no alterations observed on routine bloodwork at 2, 6, and 12 weeks during either arm of the study. Epileptic seizure frequency decreased across the population from a mean of 8.0 ± 4.8 during placebo treatment to 5.0 ± 3.6 with CBD/CBDA-rich hemp extract (P = 0.02). In addition, epileptic seizure event days over the 12 weeks of CBD/CBDA-rich hemp treatment were 4.1 ± 3.4, which was significantly different than during the 12 weeks of placebo treatment (5.8 ± 3.1; P =0.02). The number of dogs with a 50% reduction in epileptic activity while on treatment were 6/14, whereas 0/14 had reductions of 50% or greater while on the placebo (P = 0.02). No differences were observed in serum zonisamide, phenobarbital or bromide concentrations while on the treatment across groups. Adverse events were minimal, but included somnolence (3/14) and transient increases in ataxia (4/14) during CBD/CBDA-rich hemp extract treatment; this was not significantly different from placebo. This further indicates that providing CBD/CBDA-rich hemp extract during refractory epilepsy (only partially responsive to ASM), in conjunction with other ASM appears safe. Based on this information, the use of 2 mg/kg every 12 h of a CBD/CBDA-rich hemp extract can have benefits in reducing the incidence of epileptic seizures, when used concurrently with other ASMs.
Clinical course and MRI lesion progression over four years in a dog with final diagnosis of high-grade oligodendroglioma in the forebrain. F. Graciolli Tomazi, V. M. Stein, A. Oevermann, F. Meneses, A. Maiolini. 34th Symposium ESVN-SCVN; P84. J. Vet. Intern. Med. September 2022; doi: 10.1111/jvim.17218. Quote: A 9-month-old female intact Cavalier King Charles Spaniel was presented with a 3-month history of paroxysmal episodes of pain and cervical scratching. MRI revealed a large left frontal lobe intra-axial complex cystic lesion with faint incomplete rim enhancement, transtentorial and transforaminal brain herniation, and cervical syringomyelia. A primary brain tumor (glioblastoma or anaplastic astrocytoma), or less likely a parasitic cyst where suspected. Palliative treatment (dexamethasone, omeprazole, gabapentine) reduced the frequency of the paroxysmal episodes. On MRI recheck 30 months later, the lesion showed comparable size, evidence of hemorrhage or mineralization, and regressive signs of increased intracranial pressure and perilesional edema. Considering the clinical evolution and rather benign biological behavior, porencephaly, congenital cystic malformations or less likely a parasitic cyst where then considered as differentials for the lesion. The patient remained clinically stable for another 19 months until generalized, tonic-clonic, epileptic seizures acutely occurred. The neurological status subsequently deteriorated over 48 hours to stupor, cardiovascular arrest and eventually death. Post-mortem MRI showed lesion progression characterized by increased size, increased soft tissue component, invasion of the left lateral ventricle, transtentorial and transforaminal brain herniation. Neuropathology revealed an anaplastic oligodendroglioma (WHO grade III) with subarachnoidal and intraventricular drop metastasis. Although oligodendroglioma is a common primary intracranial tumor in dogs, survival data are scarce because of lack of systematic and prospective follow-up studies. This is the first report describing the long-term clinical course and MRI lesion progression under palliative treatment of a dog eventually diagnosed with high-grade oligodendroglioma.
ACADM Frameshift Variant in Cavalier King Charles Spaniels with Medium-Chain Acyl-CoA Dehydrogenase Deficiency. Matthias Christen, Jos Bongers, Déborah Mathis, Vidhya Jagannathan, Rodrigo Gutierrez Quintana, Tosso Leeb. Genes. October 2022; doi: 10.3390/genes13101847. Quote: A 3-year-old, male neutered Cavalier King Charles Spaniel (CKCS) presented with complex focal seizures and prolonged lethargy. The aim of the study was to investigate the clinical signs, metabolic changes and underlying genetic defect. Blood and urine organic acid analysis revealed increased medium-chain fatty acids and together with the clinical findings suggested a diagnosis of medium-chain acyl-CoA dehydrogenase (MCAD) deficiency. We sequenced the genome of the affected dog and compared the data to 923 control genomes of different dog breeds. The ACADM gene encoding MCAD was considered the top functional candidate gene. The genetic analysis revealed a single homozygous private protein-changing variant in ACADM in the affected dog. This variant, XM_038541645.1:c.444_445delinsGTTAATTCTCAATATTGTCTAAGAATTATG, introduces a premature stop codon and is predicted to result in truncation of ~63% of the wild type MCAD open reading frame, XP_038397573.1:p.(Thr150Ilefs*6). Targeted genotyping of the variant in 162 additional CKCS revealed a variant allele frequency of 23.5% and twelve additional homozygous mutant dogs. The acylcarnitine C8/C12 ratio was elevated ~43.3 fold in homozygous mutant dogs as compared to homozygous wild type dogs. ... The dog was prescribed 40 mg/kg levetiracetam three times a day, however this resulted in severe sedation. The levetiracetam dose was therefore lowered to 25 mg/kg three times a day and 3 m/kg phenobarbital twice a day was started, which resulted in a partial response as the seizures decreased in frequency and intensity. The patient remained stable for 3 months before the seizure interval increased again and particularly the lethargy remained present up to 24 h. The dog would return to normal the following morning. An increase in the phenobarbital dose was not accompanied by an improvment. Given the unusual presentation, urine was analyzed for organic acids and revealed significant excretion of hexanoylglycine and a peak of suberic acid, highly suggestive of a fatty acid β oxidation disorder. A follow up test consisted of blood spot acylcarnitine analysis and revealed an increase in C6, C8 and C10:1 acylcarnitines, as judged against human adult reference intervals and a clinically normal dog. Extrapolating from human patients, and in comparison with the control dog, the acylcarnitine profile was consistent with a diagnosis of medium chain acyl CoA dehydrogenase deficiency. In addition to 25 mg/kg levetiracetam three times a day and 3.75 mg/kg phenobarbital twice a day, the dog was prescribed a low fat diet and a midnight snack consisting of carbohydrates. Prolonged periods of fasting and formulas that contained medium chain triglycerides as primary source of fat were also advised to avoid. This management protocol correlated with a complete resolution of clinical signs for the following 6 months. The anticonvulsant medication was therefore reduced to subtherapeutic levels. However, this was reversed as the dose reduction resulted in an increase in seizure frequency. The blood spot acylcarnitines were repeated to test sufficient free carnitine levels and these were found within normal limits. At the time of writing, the dog has been stable for 9 months on 25 mg/kg levetiracetam three times a day, 3 mg/kg phenobarbital twice a day and a low fat diet, with no further major seizures and a repeated normal neurological examination. ... We genotyped the variant in a cohort of 162 CKCS that were not closely related to the index case and sampled during an independent study (Table 2). This experiment revealed 52 heterozygous carriers and 12 homozygous mutant dogs. The genotype distribution did not significantly deviate from Hardy–Weinberg equilibrium. The frequency of the putative disease allele was 23.5% in the investigated CKCS population. ... Based on available clinical and biochemical data together with current knowledge in humans, we propose the ACADM frameshift variant as causative variant for the MCAD deficiency with likely contribution to the neurological phenotype in the index case. Testing the CKCS breeding population for the identified ACADM variant is recommended to prevent the unintentional breeding of dogs with MCAD deficiency. Further prospective studies are warranted to assess the clinical consequences of this enzyme defect.
Malformation of Cortical Development (MCDs) in a Dog with Drug-resistant
Epilepsy. Laurent Garosi, Ines Carrera, Simon Platt. Vet Oracle
Teleradiology. July 2023. Quote: The MR study of the brain below was
submitted to us at Vet Oracle Teleradiology by Dr Kaloyan Voychev at MVC
hospital in Bulgaria. These images were from a 2yr old CKCS
with severe epileptic seizures since 4 month of age. Despite ending up on
three antiseizure medications at recommended dosages, the seizures continued
to get worse with 3 to 4 episodes of severe cluster seizures a months
lasting 24 to 48 hrs each.
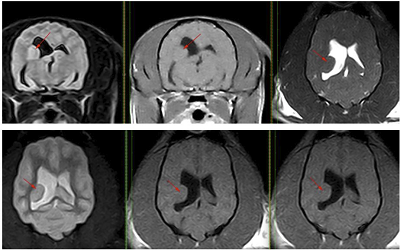 Relevant
MR images are below and showed a well-defined nodular lesion protruding
within the right lateral ventricle at the level of the parietal lobe. This
lesion was homogeneous with similar signal intensity as gray matter on all
sequences and it was well-demarcated from the adjacent white matter. There
was no associated contrast enhancement or perilesional edema. The MR images
were considered strongly suggestive of subependymal neuronal heterotopia.
Gray matter heterotopia is classified as a subgroup of MCDs and involves
clusters of normal neurons in abnormal locations, mainly due to abnormal
neuronal migration. Neurons start migrating from the ventricular and
subependymal zones after completing their final division and having
established their polarity. Migration occurs either radially or, less
commonly, tangentially. Too early or too late migration leads to disruption
of the normal neuronal migration and associated disorders. Although
histopathology would be required to confirm the diagnosis, subependymal
neuronal heterotopia was suspected. This type of malformation is very rare
in dogs and people affected with MCDs show high incidence of drug-resistant
epilepsy. It remains to be established in veterinary medicine if surgical
excision as sometime considered in people can help with seizure control.
Relevant
MR images are below and showed a well-defined nodular lesion protruding
within the right lateral ventricle at the level of the parietal lobe. This
lesion was homogeneous with similar signal intensity as gray matter on all
sequences and it was well-demarcated from the adjacent white matter. There
was no associated contrast enhancement or perilesional edema. The MR images
were considered strongly suggestive of subependymal neuronal heterotopia.
Gray matter heterotopia is classified as a subgroup of MCDs and involves
clusters of normal neurons in abnormal locations, mainly due to abnormal
neuronal migration. Neurons start migrating from the ventricular and
subependymal zones after completing their final division and having
established their polarity. Migration occurs either radially or, less
commonly, tangentially. Too early or too late migration leads to disruption
of the normal neuronal migration and associated disorders. Although
histopathology would be required to confirm the diagnosis, subependymal
neuronal heterotopia was suspected. This type of malformation is very rare
in dogs and people affected with MCDs show high incidence of drug-resistant
epilepsy. It remains to be established in veterinary medicine if surgical
excision as sometime considered in people can help with seizure control.
Faecal Microbial Transplantation in a Cavalier King Charles Spaniel with Drug-resistant Idiopathic Epilepsy. Fien Verdoodt, Myriam Hesta , Tijmen Willemse, Luc Van Ham, Sofie Bhatti. 8th BVNS Symposium Proceedings 'microbiome and the brain'. mARCH 2023. Quote: The management of dogs with idiopathic epilepsy (IE) remains challenging, because antiseizure drugs (ASDs) are still unsuccessful in one third of the cases. Therefore, interest in innovative therapeutic targets, like the microbiota-gut-brain axis (MGBA) is increasing. Based on growing literature, the MGBA shows high potential with low associated risks and adverse effects. Therefore, the MGBA was targeted in a canine IE patient with a severe, drug-resistant phenotype via faecal microbial transplantation (FMT). A 1.5 years old female entire Cavalier King Charles Spaniel, diagnosed with IE (Tier II) at the age of 1 year, was presented at the UGent Small Animal Clinic for optimization of antiseizure management. At first presentation the dog received levetiracetam 23 mg/kg TID with a high mean seizure frequency (MSF). ASD management was adapted and phenobarbital 4.6 mg/kg BID was started, while tapering down levetiracetam. Reaching an optimal serum concentration of phenobarbital, MSF remained high and potassium bromide was added at 20 mg/kg BID but lowered to 15 mg/kg BID after 3 weeks due to side effects. The MSF did not decrease. Therefore, additional management options were discussed with the owner. Firstly, the diet was changed to a medium chain triglycerides diet (MCTD, Purina Neurocare®). Six weeks later MSF remained high and consequently FMT was performed. Fresh faeces was collected on the day of FMT together with frozen faeces the day before (to achieve an adequate amount), after donor screening. The resulting faecal slurry was given via a naso- oesophagal tube at a dose of 5g/kg. The dog was hospitalized for the procedure and received omeprazole (1 mg/kg) and metoclopramide (0,3 mg/kg) before FMT. The FMT procedure was well tolerated without adverse effects. Follow-up management included enteric coated capsules with lyophilised faeces from the same donor at 207 mg/kg twice weekly. This follow up treatment started 3 weeks after FMT, for a period of 12 weeks. Faecal samples were collected before FMT and at multiple timepoints after FMT for future assessment of the engraftment of the donor microbiome via 16sDNA sequencing. Ten weeks after the FMT, MSF showed a very mild but clinically irrelevant decrease. In conclusion, this case reports confirms safety and feasibility of FMT in a clinical case of canine IE. In this dog however, the effect on MSF was negligible. The lack of effect could be due to three main aspects. Firstly, the current protocol might have caused inadequate donor engraftment. 16sDNA sequencing will reveal performance of the protocol. Secondly, variable effects on MSF might be seen in different dogs, similar to medical and nutritional management of canine IE. Thirdly, the MGBA might not be an ideal target in the management of canine IE.
Fecal microbial transplantation and microbiota analysis in a cavalier King Charles spaniel with drug-resistant idiopathic epilepsy. L. Ledeganck, F. Verdoodt, E. Goossens, M. Hesta, L. van Ham, S. F. M. Bhatti. Proceedings 35th Symposium ESVN-ECVN. September 2023. Quote: The management of dogs with idiopathic epilepsy (IE) remains challenging. Therefore, targeting the microbiota–gut–brain axis via a fecal microbial transplantation (FMT) in a canine IE patient with a severe and drug-resistant (DRE) phenotype was performed. A 1.5-year- old female entire Cavalier King Charles Spaniel was diagnosed with IE (Tier II) resistant to phenobarbital/potassium bromide and an MCT-included diet. The dog had a mean seizure frequency (SF) of 1.7 ± 1.1 seizures/week and was given FMT through naso-esophageal route. Follow-up management included oral administration of enteric coated capsules with lyophilized feces from the same donor, starting 3 weeks after the initial FMT, for a period of 12 weeks. Fecal samples from the receptor were collected before (R0), 3 weeks (R1), and 6 weeks after FMT (R2) for 16sDNA sequencing. From R0 till 25 weeks after FTM, the mean seizure frequency decreased to 1.3 ± 0.9 seizures/week (p = 0.0359). Alpha diversity, measured with Chao1 index, was higher in the donor sample (153) compared with the samples from the receptor at all timepoints (101–118). In our receptor dog, at the family level, the relative abundance of Bacteriodaceae and Lactobacillaceae decreased markedly, while Prevotellaceae, Ruminococcaceae, and Selenomonadaceae increased markedly at R1 and R2. Similar to the DRE dogs in a recent pilot study (Garcia-Belenguer, 2023) our receptor dog showed a higher relative abundance of the genera Bacteroides at R0 (32.67%), which markedly decreased at R1 (11.37%) and R2 (4.75%). In conclusion, this case report indicates that FMT may alter the baseline microbiota composition in dogs with DRE. Future directions include studies in a larger dog population and the measurement of bacterial metabolites in feces and/or serum as markers for the appropriate function of the microbiome.
The efficacy and safety of cannabidiol as adjunct treatment for drug-resistant idiopathic epilepsy in 51 dogs: A double-blinded crossover study. Aaron J. Rozental, Brooke G. Weisbeck, Isabella Corsato Alvarenga, Daniel L. Gustafson, Breonna R. Kusick, Sangeeta Rao, Lisa R. Bartner, Stephanie McGrath. J. Vet. Intern. Med. November 2023; doi: 10.1111/jvim.16912. Quote: Background: Approximately 30% of dogs with idiopathic epilepsy (IE) are drug-resistant. Recent studies have suggested cannabidiol (CBD) may be an effective anticonvulsant in dogs with IE. Objective: To evaluate the addition of CBD to antiseizure drugs (ASDs) on seizure frequency and to report adverse events in dogs with drug-resistant IE. Animals: Fifty-one dogs. Dogs having at least 2 seizures per month while receiving at least 1 ASD were included in the trial. Methods: Double-blinded placebo-controlled crossover study. The 5mg/kg/day dosage met futility requirements after 12 dogs, and a dosage of 9mg/kg/day was used in the next 39 dogs. Dogs were randomly assigned to receive CBD or placebo for 3 months, with a 1-month washout period between oils. Total numbers of seizures and seizure days were recorded. Diagnostic testing was performed periodically throughout the trial. Results: At the 9mg/kg/day dose, the decrease in total seizure frequency was significant compared with placebo. A 24.1% decrease in seizure days occurred in dogs receiving CBD and a 5.8% increase occurred in dogs receiving placebo (P≤.05). No significant difference was found in the number of responders (≥50% decrease in total seizures or seizure days). Liver enzyme activities increased at both dosages. Decreased appetite and vomiting were more common in the CBD phase (P ≤.05). Conclusions and Clinical Importance: Cannabidiol decreased total seizures and seizure days compared to placebo when administered to dogs PO at 9mg/kg/day. Liver enzymes should be monitored with administration of CBD in dogs.
Epilepsy is more than a simple seizure disorder: Parallels between human and canine cognitive and behavioural comorbidities. Saskia I. Peek, Sebastian Meller, Friederike Twele, Rowena M.A. Packer, Holger A. Volk. Vet. J. February 2024; doi: 10.1016/j.tvjl.2023.106060. Quote: Highlights: •Neurobehavioural and cognitive comorbidities affect human and canine epilepsy. •Comorbidities can substantially affect quality and quantity of life. •Common comorbidities are anxiety, cognitive impairment and ADHD-like behaviours. •Intrinsic and extrinsic factors influence the occurrence and course of comorbidities. ... Psychiatric and cognitive comorbidities have been known to play a major role in human epilepsy for a long time. People with epilepsy (PWE) frequently express signs of varying psychiatric and cognitive disorders affecting their quality and quantity of life (QoL/QaoL). Over the last few years, research on behavioural comorbidities and their effect on the underlying disease have been performed in canine epilepsy. The following article reviews manifestations of comorbidities in canine epilepsy with an emphasis on patterns of clinical signs and their effects on QoL and QaoL. Cognitive and behavioural alterations in epileptic dogs are mainly represented by fear-/anxiety related behaviour and cognitive impairment (CI). Reduced trainability and altered reactions to daily situations are common results of comorbid changes posing obstacles in everyday life of owners and their dog. In addition, clinical signs similar to attention deficit hyperactivity disorder (ADHD) in humans have been reported. Canine attention-deficit-hyperactivity-disorder-like (c-ADHD-like) behaviour should, however, be evaluated critically, as there are no official criteria for diagnosis of ADHD or ADHD-like behaviour in dogs, and some of the reported signs of c-ADHD-like behaviour could be confused with anxiety-associated behaviour. Many intrinsic and extrinsic factors could potentially influence the development of behavioural and cognitive comorbidities in canine epilepsy. In particular, seizure frequency/severity, signalment and factors concerning disease management, such as pharmacotherapy and nutrition, are closely linked with the presence of the aforementioned comorbid disorders. Further studies of behavioural alterations in epileptic dogs are needed to comprehend the complexity of clinical signs and their multifactorial origin.


CONNECT WITH US