Corneal Melting (Keratomalacia) in
Cavalier King Charles Spaniels
Corneal melting (keratomalacia) is a serious condition of the cornea believed to be due to microbial infections which cause inflammation, called infectious keratitis. Cavalier King Charles spaniels are included frequently in veterinary literature reporting on the diagnosis and treatment of canine corneal melting, although this disorder is more common in French bulldogs, pugs, and other excessively brachycephalic breeds, because they can be more susceptible to injuries causing corneal ulcers.
What It Is
The cornea consists of three layers, all of which are clear. The outward layer is the epithelium, comprised of several thin layers of cells. Behind the epithelium is the stroma, and the deepest layer is Descemet’s membrane. (See diagram below.)
Corneal melting (keratomalacia) may be initiated by an injury to the eye, causing a deep
corneal ulcer, but
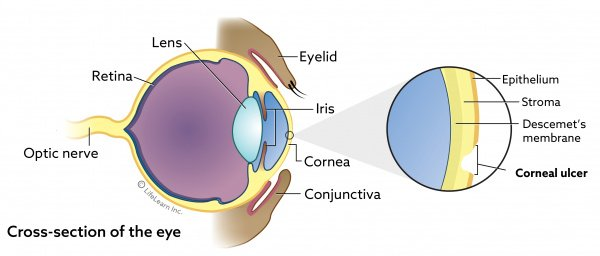 other causes include some other source of infection.
In the infectious process, enzymes are released, causing an imbalance
with proteinase inhibitors in the cornea, resulting in rapid rapid
gelatinization and liquefaction of the cornea stroma (see diagram at
right). Blindness and loss of the eye may occur if not
identified and treated as soon as possible.
other causes include some other source of infection.
In the infectious process, enzymes are released, causing an imbalance
with proteinase inhibitors in the cornea, resulting in rapid rapid
gelatinization and liquefaction of the cornea stroma (see diagram at
right). Blindness and loss of the eye may occur if not
identified and treated as soon as possible.
In an April 2021 article, a team of UK ophthalmogists reviewed the records of 110 melting corneal ulcers in 106 dogs over a period of 5 years, from 2014 to 2018. They found that the most common bacterial species associated with canine keratomalacia were Pseudomonas aeruginosa and β-hemolytic Streptococcus.
Contributing factors are brachycephalic conformation of the head, dry eye (keratoconjunctivitis sicca). treatment with topical corticosteroids, and chronic dermatologic diseaes.
RETURN TO TOP
Symptoms
A dog's cornea infected with keratomalacia literally appears to be melting, losing its normal roundness. Most cases are due to corneal ulcers. Corneal ulceration causes extreme pain, redness, light sensitivity, watering eyes, and twitching eyelids. The ulcer may also be visible to the naked eye when examined closely. See our webpage on Corneal Ulcers for more information on that disorder.
RETURN TO TOP
Diagnosis
 Corneal ulcers are detected by applying a stain, such as
fluorescein. Fluorescein is a
water-soluble stain applied to the cornea to detect corneal ulcers.
Either sterile fluorescein strips or sterile vials of fluorescein dye
are used to stain the cornea. An ulcer in the epithelial surface appears
bright green (see photo at right), especially under an ultraviolet or cobalt blue light. If the ulcer very deep, a
sample may be taken for a culture and cell study before applying the
stain or medication.
Corneal ulcers are detected by applying a stain, such as
fluorescein. Fluorescein is a
water-soluble stain applied to the cornea to detect corneal ulcers.
Either sterile fluorescein strips or sterile vials of fluorescein dye
are used to stain the cornea. An ulcer in the epithelial surface appears
bright green (see photo at right), especially under an ultraviolet or cobalt blue light. If the ulcer very deep, a
sample may be taken for a culture and cell study before applying the
stain or medication.
In addition to fluorescein staining and measurement of ulcer size, the dog also should receive a thorough ophthalmic examination, including evaluation of the menace response, dazzle reflex, pupillary light reflex, slit-lamp examination, Schirmer Tear Test I, and rebound tonometry.
In an April 2021 article, a team of UK ophthalmogists reviewed the records of 110 melting corneal ulcers in 106 dogs over a period of 5 years, from 2014 to 2018. They recommneded that because the bacteria Pseudomonas aeruginosa and β-hemolytic Streptococcus were common to corneal melting, bacterial culture and sensitivity testing should be performed in all dogs diagnosed with keratomalacia.
RETURN TO TOP
Treatment
Corneal melting is a vision-threatening disorder and requires a rapid response by an experienced ophthalmology specialist.
Medical treatment may successfully treat milder cases of keratomalacia. Treatments typically are the frequent application of topical antibiotics, topical and/or systemic collagenase inhibitors, and topical atropine and systemic non-steroidal anti-inflammatory treatment. Antimicrobial therapy ideally is selected based on bacterial culture and susceptibility testing, but, due ti the time lag between sampling and the availability of results, topical broad-spectrum antimicrobials may be used initially). Such medications include topical antibiotics, such as combinations of tobramycin/cefazolin, gentamicin/chloramphenicol, and ciprofloxacin/cefazolin, or monotherapy with a second-generation fluoroquinolone, topical serum or plasma, and oral doxycycline.
Photoactivated Chromophore for Keratitis-Corneal
Cross-linking (PACK-CXL) is a novel
 photodynamic therapy which
is being researched. PACK-CXL involves first applying riboflavin, a
chromophore solution, to the corneal surface of the dog, which is
lightly sedated. Then, the cornea is
exposed to ultraviolet A light irradiation (see image at right) that causes a photochemical formation
of the riboflavin which
cross-links within and on the surface of collagen fibers and between
collagen fibers and proteoglycans in the extracellular matrix. PACK-CXL
reportedly improves corneal resistance to enzymatic digestion, thereby
stopping the degradation of the corneal stromal tissue. PACK-CXL also
has been found to have antimicrobial properties which damage the
micro-organisms.
photodynamic therapy which
is being researched. PACK-CXL involves first applying riboflavin, a
chromophore solution, to the corneal surface of the dog, which is
lightly sedated. Then, the cornea is
exposed to ultraviolet A light irradiation (see image at right) that causes a photochemical formation
of the riboflavin which
cross-links within and on the surface of collagen fibers and between
collagen fibers and proteoglycans in the extracellular matrix. PACK-CXL
reportedly improves corneal resistance to enzymatic digestion, thereby
stopping the degradation of the corneal stromal tissue. PACK-CXL also
has been found to have antimicrobial properties which damage the
micro-organisms.
A minor surgical procedure is grid keratotomy, which involves pricking or scratching the eye down to the stroma to stimulate the epithelium to heal by making it easier to attach back to the stroma. General anesthesia is not required for this procedure, as a combination of sedation and local anesthesia is applied.
Surgical procedures are important options, especially for deep ulcers. In each, tissue from other parts of the patient's eyes or elsewhere is inserted into the void and then sutured to hold the repair in place. Conjunctival grafts involve taking tissue from the patient' conjunctiva, a pale membrane which covers the white of the eye and includes blood vessels. A piece of conjunctiva is moved and rotated so that it covers the ulcer and is then sutured into place. Corneal conjunctival transposition (CCT) includes both the conjunctiva and cornea. Healthy corneal tissue, with attached conjunctiva, adjacent to the ulcer is moved into the wound, with the conjunctiva providing a functioning blood supply. Other types of grafts include tissue from pig bladder, pig intestines, donor dog or pig cornea, and amnion (an innermost fetal membrane).
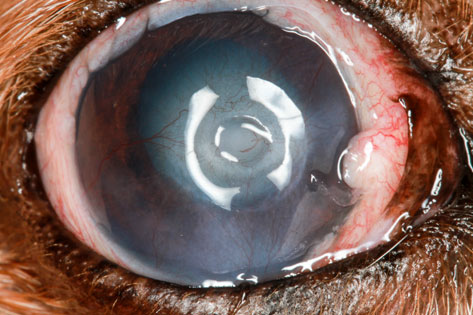
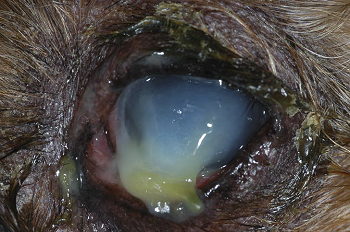
 In
a
September 2015 article, a
cavalier was among five dogs with keratomycosis, an infection in the
cornea caused by a fungus. The cavalier also had corneal
ulceration with surrounding keratomalacia. Due to the severity of the infection, a
keratectomy and conjunctival graft surgery were
successfully performed. See the before (left) and after (right)
photos of this cavalier's eye.
In
a
September 2015 article, a
cavalier was among five dogs with keratomycosis, an infection in the
cornea caused by a fungus. The cavalier also had corneal
ulceration with surrounding keratomalacia. Due to the severity of the infection, a
keratectomy and conjunctival graft surgery were
successfully performed. See the before (left) and after (right)
photos of this cavalier's eye.
In a June 2016 article, a cavalier was one of six dogs and two cats studied. The CKCS had infectious crystalline keratopathy (ICK) in its cornea. An anterior lamellar keratectomy and a corneoconjunctival transposition surgical procedure were successfully performed.
In a November 2016 article, French and UK ophthalmologists reported the 100% successful use of pig bladder grafts for corneal reconstruction in 27 dogs (and three cats), including two cavalier King Charles spaniels suffering from deep melting corneal ulcers. After 90 days following surgery, all eyes were sighted. They concluded that "Use of a porcine urinary bladder acellular matrix appears to be effective in the surgical management of deep corneal ulcers and feline corneal sequestra."
In an April 2021 article, a team of UK ophthalmogists reviewed the records of 110 melting corneal ulcers in 106 dogs over a period of 5 years, from 2014 to 2018. They found that melting corneal ulcers associated with pure Pseudomonas infection were significantly more likely to result in eye loss, despite medical and surgical treatments, than melting corneal ulcers associated with other cultures.
RETURN TO TOP
Research News
April 2021:
The most common bacteria causing melting corneal ulcers are
identified in a UK study.
 In an
April 2021 article, a team of UK ophthalmogists (Agata Tsvetanova
[right], Roger M. Powell, Kamen A. Tsvetanov, Kerry M. Smith,
David J. Gould) reviewed the records of 110 melting corneal ulcers in
106 dogs over a period of 5 years, from 2014 to 2018. They reported the
following findings:
In an
April 2021 article, a team of UK ophthalmogists (Agata Tsvetanova
[right], Roger M. Powell, Kamen A. Tsvetanov, Kerry M. Smith,
David J. Gould) reviewed the records of 110 melting corneal ulcers in
106 dogs over a period of 5 years, from 2014 to 2018. They reported the
following findings:
• 63 (57%) eyes were infected with bacterial growth
• 26 (24%) were infected with Pseudomonas aeruginosa
• 12 (11%) were infected with β-hemolytic Streptococci
• 9 (8%) had multiple bacterial cultures
• 47 (42%) were not infected with any bacteria
• 63 (57%) eyes received surgical grafting in addition to medical treatment
• 14 (13%) eyes had to be removed despite medical and surgical treatment
• 8 (57%) of the removed eyes were diagnosed with pure Pseudomonas aeruginosa isolatesAll eyes diagnosed with β-hemolytic Streptococci were healed
They concluded:
"The most common bacterial species associated with canine keratomalacia were Pseudomonas aeruginosa and β-hemolytic Streptococcus. Because of the variation in antibacterial sensitivity between these two species, bacterial culture and sensitivity testing should be performed in all dogs presenting with keratomalacia. Melting corneal ulcers associated with pure Pseudomonas infection were significantly more likely to result in globe loss than melting corneal ulcers associated with other cultures."
November 2016: Pig bladder grafts for deep melting corneal ulcers in two cavaliers are successful. In a November 2016 article, French and UK ophthalmologists (Olivier Balland, Anne-Sophie Poinsard, Frank Famose, Frédéric Goulle, Pierre-François Isard, Iona Mathieson, Thomas Dulaurent) reported the 100% successful use of pig bladder grafts for corneal reconstruction in 27 dogs (and three cats), including two cavalier King Charles spaniels suffering from deep melting corneal ulcers. After 90 days following surgery, all eyes were sighted. They concluded that "Use of a porcine urinary bladder acellular matrix appears to be effective in the surgical management of deep corneal ulcers and feline corneal sequestra."
September 2015: Australian
ophthalmologists successfully perform graft surgery on a cavalier with
keratomalacia.
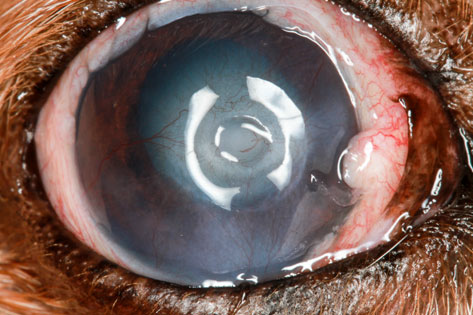
 In
a
September 2015 article, a team
of Australian ophthalmologists (Jessica C. Nevile, Simon D. Hurn, Andrew
G. Turner) treated a
cavalier diagnosed with keratomycosis, an infection in the
cornea caused by a fungus. The cavalier also had corneal ulceration with
surrounding keratomalacia. Due to the severity of the infection, a
keratectomy (corneal surgery) and conjunctival graft surgery were
successfully performed. See the before (left) and after (right)
photos of this cavalier's eye.
In
a
September 2015 article, a team
of Australian ophthalmologists (Jessica C. Nevile, Simon D. Hurn, Andrew
G. Turner) treated a
cavalier diagnosed with keratomycosis, an infection in the
cornea caused by a fungus. The cavalier also had corneal ulceration with
surrounding keratomalacia. Due to the severity of the infection, a
keratectomy (corneal surgery) and conjunctival graft surgery were
successfully performed. See the before (left) and after (right)
photos of this cavalier's eye.
RETURN TO TOP
RETURN TO TOP
Veterinary Resources
Surgical repair of deep melting ulcers with porcine small intestinal submucosa (SIS) graft in dogs and cats. Maria Vanore, Sabine Chahory, Guillaume Payen, Bernard Clerc. Vet. Ophtal. March 2007;10(2):93-99. Quote: Abstract Purpose: To evaluate the efficacy of using a porcine small intestinal submucosa (SIS) graft for the surgical repair of deep melting ulcers in dogs and cats. Methods: Two cats and five dogs [incluidng one cavalier King Charles spaniel, diagnosed with hypopion and melting ulcer] presented with deep and large melting ulcers of the cornea. In each case, the necrotic and collagenolytic tissue of the cornea was removed by keratectomy. A SIS graft, 1 mm greater than the corneal defect, was rehydrated in sterile saline and sutured to the edges of the ulcer with a simple interrupted pattern of 9/0 polyglactin 910. A nictitating membrane flap was utilized in two cats and four dogs for 2 weeks. All cases were treated postoperatively with topical and systemic antibiotics, a systemic anti‐inflammatory drug and topical atropine. All animals were re‐evaluated 15 days, 4 weeks, 35–45 days, 2–3 months and 6 months postsurgery. Results: At 15 days postsurgery, a superficial intense corneal neovascularization surrounded the SIS graft. No ocular discomfort was present and fluorescein staining was negative in all cases. At 4 weeks the SIS graft was thick and opaque in all cases, although in one cat the SIS graft had partially detached. Between 35 and 45 days, SIS graft integration was evident in all eyes, and corneal neovascularization had decreased progressively. All eyes healed without complications and retained corneal transparency. This occurred even in the presence of corneal perforation in two cases: one prior to and one during surgery. Conclusion: Results of our study suggest the SIS graft may be an effective alternative surgical treatment to the traditional conjunctival grafts commonly used to repair melting ulcers in dogs and cats. The advantages of using a SIS graft include good corneal transparency, preservation of corneal integrity and maintenance of vision.
Proteinases of the cornea and preocular tear film. F. J. Ollivier, B. C. Gilger, K. P. Barrie, M. E. Kallberg, C. E. Plummer, S. O’Reilly, K. N. Gelatt, D. E. Brooks. Vet. Ophthal. July 2007;10(4):199-206. Quote: Maintenance and repair of corneal stromal extracellular matrix (ECM) requires a tightly coordinated balance of ECM synthesis, degradation and remodeling in which proteolytic enzymes (proteinases) perform important functions. There are natural proteinase inhibitors present in preocular tear film (PTF) and cornea simultaneously with proteinases that prevent excessive degradation of normal healthy tissue. Disorders occur when there is an imbalance between proteinases and proteinase inhibitors in favor of the proteinases, causing pathologic degradation of stromal collagen and proteoglycans in the cornea. Two matrix metalloproteinases (MMPs), MMP‐2 and MMP‐9, are of major importance in terms of remodeling and degradation of the corneal stromal collagen. Immunohistochemical studies have shown different origins of MMP‐2 and ‐9. MMP‐2 is synthesized by corneal keratocytes and performs a surveillance function in the normal cornea, becoming locally activated to degrade collagen molecules that occasionally become damaged. Alternatively, MMP‐9 may be produced by epithelial cells and polymorphonuclear neutrophils following corneal wounding. Because the cornea is in close contact with the preocular tear film (PTF), proteinases have been evaluated in the PTF. In damaged corneas, total proteolytic activity in the tear fluid was found to be significantly increased compared to normal eyes and contralateral eyes. Studies analyzing the proteolytic activity in serial PTF samples during corneal healing led to the following conclusions: ulcerative keratitis in animals is associated with initially high levels of tear film proteolytic activity, which decrease as ulcers heal; proteinase levels in melting ulcers remain elevated leading to rapid progression of the ulcers. The success of medical and surgical treatment of the corneal ulcers is reflected by the proteolytic activity in tears. In animals, successful treatment leads to a rapid reduction in tear film proteolytic activity that corresponds with the improvement in the clinical signs of corneal ulceration. The in vitro effects of various compounds on proteolytic activity in the tear fluid of animals with ulcerative keratitis have been evaluated and their important inhibitory effects have been confirmed. Because these various compounds utilize different mechanisms to inhibit various families of proteinases, a combination of these proteinase inhibitors may be beneficial.
Evaluation of accelerated collagen cross-linking for the treatment of melting keratitis in eight dogs. Frank Famose. Vet. Opthal. September 2014;17(5):358-367. Quote: Objective: Melting keratitis is serious condition presenting a high risk of permanent blindness and is caused by infectious or noninfectious factors. In humans, the clinical efficacy of collagen cross‐linking (CXL) has been described in the treatment of refractory infectious keratitis by arresting keratomalacia. The aim of this study was to evaluate the efficacy of accelerated CXL for the treatment of melting keratitis in dogs. Animal studied and Procedure: Eight dogs were treated for unilateral melting keratitis by accelerated CXL [including two cavalier King Charles spaniels (25%)]. ... The two Cavalier King Charles Spaniels that presented [had] macropalpebral fissures [a film-like scar tissue forming on the corneas. Dogs with macropalpebral fissure syndrome cannot blink their eyelids effectively.] ... Corneas were irradiated by UVA (370 nm) at 30 mW/cm² irradiance for 3 min after soaking by 0.1% riboflavin in 20% dextran for 30 min. Follow‐up was conducted 3, 7, 14, and 30 days after treatment. Results: Pain improvement was observed for all cases within 3 days after treatment. Epithelial healing was observed within 15 days for all cases. Disappearance of cellular infiltration was observed for all cases at day 7. The corneal vascularization disappeared for 4 of 8 dogs and was reduced for 4 of 8 dogs within 1 month. At 1 month, all cases presented a variable degree of corneal scarring, but all eyes had visual function. No recurrent infection was observed. Conclusions: The main observation of this study is that all the cases have presented with the same clinical result regardless of the presence and the sensitivity of the infectious agents and regardless of the duration of the condition prior to CXL treatment. Accelerated CXL appears to be a valuable option for the treatment of melting keratitis.
Infectious crystalline keratopathy in dogs and cats: clinical, in vivo confocal microscopic, histopathologic, and microbiologic features of eight cases. Eric C. Ledbetter, Patrick L. McDonough, Kay Kim. Veterinary Ophthalmology. June 2016. Quote: Objective: To describe clinical, in vivo confocal microscopic, histopathologic, and microbiologic features of canine and feline cases of infectious crystalline keratopathy (ICK). Animals studied: Six dogs [including one cavalier King Charles spaniel] and two cats with naturally acquired ICK. Procedures: Medical records of dogs and cats with a clinical diagnosis of ICK were reviewed. Signalment, medical history, clinical findings, and diagnostic evaluations were retrieved, including corneal cytology, histopathology, in vivo confocal microscopy, and microbiology results. Results: All animals presented with fine, needle-like, and branching white crystalline anterior stromal opacities emanating from corneal facets or corneal epithelial defects. Mild conjunctival hyperemia and anterior uveitis were frequently present. Concurrent ocular and systemic diseases were common, including keratoconjunctivitis sicca, corneal sequestrum, diabetes mellitus, hyperadrenocorticism, and malignant neoplasia. Bacteria, with minimal or absent leukocytes, were identified by cytology and histopathology. Histopathologically, the crystalline corneal opacities corresponded with dense accumulations of bacteria present in the interlamellar stromal spaces and forming cord-like projections within the stroma. In vivo confocal microscopy demonstrated deposits of reflective crystalline or amorphous structures within the stroma with a paucity of associated inflammatory changes. The most frequently cultured bacteria were alpha-hemolytic Streptococcus and Staphylococcus species. Resolution of clinical lesions was achieved in most cases with long-term medical or surgical therapy; however, the initiation of medical treatment was associated with an acute, dramatic onset of severe keratitis and anterior uveitis in some animals. Conclusions: Infectious crystalline keratopathy in dogs and cats shares many features with this condition in human patients. Prolonged medical therapy, or surgical intervention, is required for resolution.
Keratomycosis in five dogs. Jessica C. Nevile, Simon D. Hurn, Andrew G. Turner. Vet. Ophthal. September 2016;19(5):432-438. Quote: Five cases of canine keratomycosis were diagnosed and treated at a private Veterinary Ophthalmology Practice in Melbourne, Australia. Clinical presentations varied between dogs. ... Case 1: A 10-year 7-month-old spayed female Cavalier King Charles Spaniel was referred for a corneal ulcer in the right eye (OD). The dog was systemically healthy, there was no known history of trauma, and the dog had not been treated with topical or systemic corticosteroids prior to presentation. ... There was an axial mid-stromal corneal ulceration with surrounding keratomalacia, corneal white cell infiltrate and mild hypopyon (Fig 1). ... Predisposing factors were identified in 4 of 5 cases. Diagnostic modalities utilized were corneal cytology and fungal culture. Corneal cytology confirmed the presence of fungal organisms in all five cases. Aspergillus, Scedosporium, and Candida were cultured from three cases, respectively. Specific antifungal treatment included 1% voriconazole solution or 1% itraconazole ointment. Keratectomy and conjunctival grafting surgery was performed in two patients. Resolution of infection and preservation of vision were achieved in 4 of 5 patients.
Use of a porcine urinary bladder acellular matrix for corneal reconstruction in dogs and cats. Olivier Balland, Anne-Sophie Poinsard, Frank Famose, Frédéric Goulle, Pierre-François Isard, Iona Mathieson, Thomas Dulaurent. Vet. Ophthal. November 2016;19(6):454-463. Quote: Objective: To describe the use of a porcine urinary bladder acellular matrix for surgical reconstruction of the cornea in cases of canine and feline deep corneal ulcers, and feline corneal sequestra. Materials and methods: Twenty‐seven dogs [including two cavalier King Charles spaniels, both with deep, melting corneal ulcers] and three cats with deep corneal ulcers and seven cats with corneal sequestra were included in the study with overall 38 eyes. For each patient, the necrotic material (ie corneal sequestrum or collagenolytic tissue) was removed by circular lamellar keratectomy. The collagen graft was then cut and prepared to match the stromal defect and then sutured into the lamellar keratectomy bed using interrupted and continuous patterns of absorbable polyglactin 9–0 sutures. Postoperative medical treatment consisted of topical and systemic administration of antibiotics, combined with topical administration of atropine sulfate. The animals were examined 18, 45, and 90 days after the surgery. Results: Postoperative examination revealed complete integration of the biomaterial in 93.5% of ulceration cases in both species and in 100% of feline corneal sequestrum cases. In two cases of ulceration (1 dog and 1 cat), progression of the collagenolytic process at the graft periphery required an additional conjunctival graft 7 days after the first surgery. At 90 days post‐op, 100% of the eyes were sighted. Conclusion: Use of a porcine urinary bladder acellular matrix appears to be effective in the surgical management of deep corneal ulcers and feline corneal sequestra.
Outcome of medical therapy for keratomalacia in dogs. A. Guyonnet, L. Desquilbet, J. Faure, A. Bourguet, E. Donzel, S. Chahory. J. Sm. Anim. Pract. April 2020;61(4):253-258. Quote: Objectives: To evaluate the clinical and visual outcomes following intensive medical therapy for keratomalacia in dogs. Materials and Methods: Medical records were screened to identify dogs with corneal ulcers and keratomalacia. All patients were given the same topical treatment protocol with frequent administrations of tobramycin in combination with equine serum. Surgical treatment during the first 15 days of follow‐up was considered as medical treatment failure. Results: We report on 57 ulcers with keratomalacia from 53 dogs [including one cavalier King Charles spaniel]. ... The most commonly represented breeds were French bulldog (n = 13), Yorkshire terrier (n = 9), shih-tzu (n = 7), pug (n = 5) ... Medical treatment was successful in 31 of 57 ulcers with a median healing time of 5 days (range 2 to 15 days). At 60 days after epithelialisation, 14/15 medically‐treated eyes were visual. In one case, corneal perforation was observed 1 month after healing and required surgical stabilisation. Clinical Significance: Intensive medical therapy has the potential to achieve healing of some ulcers with keratomalacia. Surgical stabilisation in response to progression of stromal loss was required in less than half of the cases.
Melting corneal ulcers (keratomalacia) in dogs: A 5-year clinical and microbiological study (2014–2018). Agata Tsvetanova, Roger M. Powell, Kamen A. Tsvetanov, Kerry M. Smith, David J. Gould. Vet. Ophthal. April 2021; doi: 10.1111/vop.12885. Quote: Objectives: To identify bacterial microorganisms associated with canine keratomalacia, review their antimicrobial sensitivity, and evaluate clinical outcomes compared to results of microbial culture. Methods: Retrospective analysis of clinical records of dogs diagnosed with a melting corneal ulcer presented to a referral hospital in Hertfordshire, UK between 2014 and 2018. Results: One hundred and ten melting corneal ulcers were sampled in 106 dogs. The most common pure bacterial isolate was Pseudomonas aeruginosa (n = 26) followed by β-hemolytic Streptococcus (n = 12). Melting corneal ulcers that cultured coagulase-positive Staphylococcus, coliform bacteria, Pasteurella multocida, Enterococcus, and Streptococcus viridans presented in smaller numbers and were analyzed together (n = 16). Multiple cultures were identified in nine cases (n = 9). Forty-seven cultures yielded no bacterial growth (n = 47). The susceptibility to fluoroquinolones remained high with the exception of β-hemolytic Streptococci. There was no significant difference in the ulcer severity at presentation in regard to the cultured bacteria. Overall, 63 eyes (57%) received surgical grafting in addition to medical treatment. In 14 cases (13%), the progression of corneal melting despite medical ± surgical treatment resulted in enucleation. Fifty-seven percent (8/14) of the enucleated eyes cultured pure Pseudomonas aeruginosa isolates. In contrast, all β-hemolytic Streptococcus‐associated ulcers healed. Conclusions: The most common bacterial species associated with canine keratomalacia were Pseudomonas aeruginosa and β-hemolytic Streptococcus. Because of the variation in antibacterial sensitivity between these two species, bacterial culture and sensitivity testing should be performed in all dogs presenting with keratomalacia. Melting corneal ulcers associated with pure Pseudomonas infection were significantly more likely to result in globe loss than melting corneal ulcers associated with other cultures.

CONNECT WITH US