
- How to spot an ignorant veterinary cardiologist -- Part One -- February 19, 2026
- CKCSC,USA out snobs the UK Kennel Club. -- February 8, 2026
- Why Social Media Veterinary Pill Merchants should be ignored. -- February 1, 2026
- Entresto (sacubitril/valsartan) for treating canine myxomatous mitral valve disease. -- December 7, 2025
- Artificial Intelligence (AI) is an oxymoron. It definitely is "artificial", but it definitely also IS NOT "intelligent". -- November 18, 2025
- Coughing is NOT a sign of onset of heart failure in dogs with mitral valve disease. -- November 17, 2025
- Toothless cavaliers are disabled dogs. -- October 29, 2025
- Health disorders you should assume your cavalier will develop ... -- August 9, 2025
- Why Social Media Veterinary Pill Merchants Should Be Ignored. -- June 6, 2025
- Cavaliers diagnosed with mitral valve disease need sodium in their diets. -- September 21, 2024
- How to find a well qualified holistic veterinarian to treat your cavalier King Charles spaniel. -- July 19, 2024
- Be wary of social media veterinarians who recommend products they sell. -- July 15, 2024
- Cardiologists' obsession with the LA/Ao clouds their analyses of multiple echocardiograms of cavalier patients. -- July 11, 2024
- Wild Hair Syndrome infects cavalier fanciers. -- May 20, 2024
- Nutrition needs of dogs with mitral valve disease. -- February 17, 2024
- Is the cavalier breed about to run out of healthy genes? -- January 29, 2024
- Eggs shells are a poor source of calcium in dogs' diets. -- January 25, 2024
- Not all PEA (palmitoylethanolamide) is alike. -- November 16, 2023
- MVD-affected cavaliers need sodium in their daily meals. -- October 17, 2023
- 'Prescription' dog foods which are hazardous to cavaliers' health. -- August 21, 2023
- Why some holistic canine nutritionists may be their own worst enemies. -- May 26, 2023
- Why do cavaliers' coat colors matter? -- May 14, 2023
- Are medium chain triglycerides (MCTs) hazardous to many cavalier King Charles spaniels? -- March 11, 2023
- When not to separate cavalier puppies from their mothers - before the 14th week. -- November 26, 2022
- Beware of Internet advice to stop treating MVD-affected dogs with prescription medications. -- September 15, 2022
- Giving your cavalier a bone will not prevent or treat dental disease and may fracture teeth. -- August 24, 2022
- Peer-reviewed breed-specific ranges of normal-sized left atria (LA/Ao) and left ventricles (LVIDDN) in cavalier King Charles spaniels. -- July 20, 2022
- Japanese mitral valve surgeons at JASMINE report their MVD surgery statistics. -- July 10, 2022
- Why are cardiologists obsessed with predicting when MVD-affected cavaliers will die? -- June 29, 2022
- Veterinarians' seat-of-the-pants diagnosis and treatment of mitral valve disease. -- February 22, 2022
- Don't be fooled by Purina's hype of its new "Pro Plan CardioCare" kibble dog food. -- November 18, 2021
- Your MVD-affected cavalier is losing weight. What to do? -- October 2, 2021
- The cavalier King Charles spaniel is pre-disposed to ... August 27, 2021
- Should MVD-Affected Dogs Start Furosemide Treatment Before Congestive Heart Failure? -- March 24, 2021
- Boehringer Academy spreads dangerously false information about when MVD-affected dogs should first be treated with Vetmedin. -- December 3, 2020
- Should arbitrary reference intervals in research studies also be used to diagnose individual MVD patients? -- October 5, 2020
- Cavaliers' coats are not meant to be cut, trimmed, or shaved. -- July 17, 2020
- Why do so many ACVIM cardiologists insist upon being Stuck On Stupid? -- May 12, 2020
- Cardiologist Dr. Gordon recommended VHS>10.5 but rejects >11.5 to define heart enlargement -- Oct. 7, 2019
- CavalierHealth.org's first aid kit for our traveling cavaliers -- July 30, 2019
- ACVIM's new definition of Stage B2 heart enlargement ignorantly assumes that one size fits all -- June 25, 2019
- ACVIM's new definition of Stage B2 mitral valve disease will include dogs with normal-sized hearts -- April 19, 2019
- EPIC Study lead investigator admits that its definition of heart enlargement is inaccurate -- Feb. 2, 2019
- What Cavalier Health news may we expect in 2019? -- January 1, 2019
- Many General Practice Vets are MVD-Quacks! -- October 16, 2018
- There is no better advocate for your dog, than YOU! -- Aug 26, 2018
- D-ribose can boost the energy in MVD-affected hearts -- May 7, 2018
- Did the EPIC Study investigators intentionally enroll Stage B1 cavaliers in their trial? -- Dec 22, 2017
- Why do researchers invent definitions of species-wide heart enlargement to test risky drugs? -- Nov 7, 2017
- The EPIC Study's parameters are arbitrary and unsupported -- October 21, 2017
- Telemedicine is the answer, when no cardiologist is nearby -- September 19, 2017
- CEG doubles down on prescribing Vetmedin to dogs without enlarged hearts -- September 14, 2017
- The Cardiac Education Group waters down the EPIC Trial recommendations -- July 10, 2017
- ACVIM forum Consensus Statement further deteriorates the flawed EPIC Study report -- July 3, 2017
- ACKCSC's charitable trust falls for the impossible promised dream -- June 17, 2017
- Ten Frequently Asked Questions About Cavaliers and Mitral Valve Disease -- June 15, 2017
- When should intact cavaliers have a preventative prostate ultrasound? -- June 14, 2017
- EPIC study's bluster about pimobendan unravels as critical analysis finally takes hold. -- May 28, 2017
- Will GP vets cut corners to prematurely prescribe pimobendan to cavaliers? -- March 16, 2017
- Does detecting heart failure in MVD-affected cavaliers matter anymore? -- February 3, 2017
- All that cavalier owners need to know about spironolactone -- January 20, 2017
- Why do vets prescribe useless drugs to MVD-affected cavaliers before heart failure? -- Dec. 20, 2016
- Pimobendan's EPIC Study: The BAD and the UGLY! -- October 3, 2016
- So your cavalier has a heart murmur. What do you do next? UPDATED! -- Sept. 30, 2016
- Is the Univ. of Washington's "Rapamycin Intervention Trial in Pet Dogs" Unethical? -- Aug. 18, 2016
- Whither the EPIC Trial's final report? -- August 3, 2016
- OFA finally recognizes what mitral valve disease is all about -- April 15, 2016
- Cavalier breeders boycott posting health test clearances on the OFA website -- April 14, 2016
- EPIC trial results are scheduled to be announced at ACVIM Forum in Denver in June -- Feb. 2, 2016
- Too many cavaliers are too fat! -- October 25, 2015
- Cardiologists focus on bionic fixes to the leaking mitral valve -- October 14, 2015
- Heart failure in the MVD-affected cavalier King Charles spaniel -- July 1, 2015
- The CKCSC,USA makes part of its ethics code optional -- April 30, 2015
- "Purebred breeding" is a euphemism for accelerated genetic entrophy -- April 19, 2015
- The EPIC trial ends on schedule, but could a whitewash be in the works? -- March 25, 2015
- Is it 'Back to the Future' for the American Kennel Club? -- March 19, 2015
- All that cavalier owners need to know about the "Reverse Sneeze" or "Cavalier Snort" -- Feb. 10, 2015
- Just Asking: What's up with Vetmedin's 'EPIC Trial'? -- October 20, 2014
- So your cavalier has a heart murmur. What do you do next? -- October 13, 2014
- Do MVD-affected cavalier King Charles spaniels really need taurine supplements? -- October 11, 2014
- When NOT to start giving your cavalier pimobendan (Vetmedin). -- July 12, 2014
- Do-it-yourself diagnosing of congestive heart failure in your cavalier. -- June 18, 2014
- Dog food companies may be turning a grain-free corner. -- March 10, 2014
- The accordion-muzzled cavalier King Charles spaniel. -- December 12, 2013
- All that cavalier owners need to know about primary secretory otitis media. -- September 23, 2013
- All that cavalier owners need to know about their dogs' blood platelets. -- August 26, 2013
- What if the American Kennel Club ceased to exist? -- August 10, 2013
- All that cavalier owners need to know about natriuretic peptides tests (ANP & BNP). -- July 9, 2013
- The cavalier King Charles spaniel is pre-disposed to ... -- July 7, 2013
- CKCSC,USA embarks on an offensive "charm offensive" -- March 26, 2013
- AVMA's House of Nannies aims at homeopathic vets -- December 18, 2012
- Dog food companies lie, and allergic dogs may die -- September 27, 2012
- Update on Hill's Science Diet junk food. -- September 26, 2012
- The US cavalier clubs contemptuously keep whistling past our breed's graveyard. -- August 3, 2012
- The insidious mind control over clueless veterinarians by Hill's Pet "Nutrition". -- June 14, 2012
- Congratulations to Her Majesty, lover of cavaliers! -- June 3, 2012
- When ignorance (stupidity?) guides cavalier PSOM research -- May 9, 2012
- AKC's CHIC program is a farce for cavaliers -- March 14, 2012
- Pedigree Dogs Exposed: The Sequel, or The End? -- March 1, 2012
- Will the next SM breeding protocol be BAD FOR THE BREED? -- December 24, 2011
- What do the two USA CKCS clubs have against breeding healthy cavaliers? -- October 14, 2011
- A neurologist answers our August 13 questions -- September 13, 2011
- Plucking the MVD genes: The first shoe has dropped! -- August 29, 2011
- Will the CSF-space gap predict future syringomyelia in cavaliers? -- August 18, 2011
- Okay, syringomyelia researchers: What now? Where do we go from here? -- August 13, 2011
- AKC Chairman Ron Menaker condemns "Pedigree Dogs Exposed" -- July 24, 2011
- How the SM breeding protocol could lead to the Popular Sire Syndrome -- June 13, 2011
- CKCSC,USA board admits its ignorance ... but not its stupidity! -- May 11, 2011
- Beware the pimobendan/Vetmedin "EPIC clinical trial": There is no upside -- April 23, 2011
- Chiari-like malformation HAS been re-defined! -- January 30, 2011
- Maybe cavaliers don't even have Chiari-like malformation (CM)! -- January 28, 2011
- CKCSC,USA's board reinstates a third of the REAL MVD breeding protocol -- December 28, 2010
- To CKCSC,USA's board: Reinstate the REAL MVD breeding protocol! -- October 7, 2010
- How self-absorbed can the CKCSC,USA board be? -- September 10, 2010
- CKCSC,USA dumps the MVD breeding protocol -- September 7, 2010
RETURN TO TOP
February 19, 2026:
How to spot an ignorant veterinary cardiologist -- Part One
Prescribing taurine to treat mitral valve disease
First of a series
 Board certified veterinary cardiologists, who are tested and certified by
either the American College of Veterinary Internal Medicine (ACVIM) or the
European College of Veterinary Internal Medicine (ECVIM-CA), are presumed to
know more about canine heart diseases than any other veterinarians, or
anybody else, for that matter. But not always.
Board certified veterinary cardiologists, who are tested and certified by
either the American College of Veterinary Internal Medicine (ACVIM) or the
European College of Veterinary Internal Medicine (ECVIM-CA), are presumed to
know more about canine heart diseases than any other veterinarians, or
anybody else, for that matter. But not always.
All too often we hear that board certified veterinary cardiologists have been prescribing synthetic, chemical versions of taurine to dogs diagnosed with myxomatous mitral valve disease (MVD). Why is that?
It is well established in peer-reviewed veterinary research literature that MVD-affected dogs do not need taurine supplementation unless their blood plasma shows a deficiency of taurine. (More about that research below.) And yet, these cardiologists do not even bother to have their MVD patients' blood or plasma tested for taurine. Instead, they just prescribe it in a knee-jerk fashion.
In its natural state, taurine is a non-essential amino-acid. "Non-essential" means that dogs make taurine themselves from other animo acids in their livers and therefore do not need it to be supplemented. All animals create taurine naturally in their own bodies, including mammals, fish, shellfish, and poultry, including eggs. It is found in their hearts, brains, retinae, and skeletal muscles. Natural taurine is found exclusively in animal proteins and is absent from plant-sourced proteins. If MVD-affected dogs consume fresh muscle meats from those sources in their diets, they will not need the artificial, chemical version of taurine sold as a supplement. Because commercial dry dog foods (kibble) destroy the building blocks of taurine in their meat ingredients during processing, synthetic taurine is added to those ingredients. Synthetic taurine is produced mostly in China, from the raw materials of ethylene oxide, sulfuric acid, and sodium bisulfite.
Excessive dosages of synthetic taurine supplementation have been found to be toxic in rodent studies, causing extreme low and high blood pressure. Thus far, its safety in humans and canines has not been determined. So, giving taurine supplements to un-tested dogs amounts to experimenting on those dogs without any fore-knowledge of the risks involved. In general, over-supplementing -- by adding synthetic supplements to diets of dogs which do not need supplementation -- can impose an unnecessary additional burden upon the liver, kidneys, and the immune system.
So why would any cardiologist prescribe taurine for MVD without testing
the blood plasma first? We think we
 know
why. We think it is due to intellectual
laziness on the part of these cardiologists. Over the past few years,
taurine supplementation has been given a lot of publicity in cases of
another heart disease,
dilated cardiomyopathy (DCM). The headlines in veterinary newsletters
have screamed that DCM dogs may need taurine supplementation. But DCM and
MVD are totally unrelated disorders, and all veterinary cardiologists really
ought to know the difference between the two. But if the cardiologist's
attention span is so short that he does not dig any deeper than those
newsletter headlines, he remains ignorant about the distinctions between the
two disorders, and he passes his ignorance on to his MVD patients and their
owners as "professional advice". He prescribes synthetic taurine to treat
MVD, a disease that has nothing to do with taurine deficiency. In cases like
this, it is best that the dogs' owners be prepared in advance and know more than these lazy-minded
cardiologists. That is a purpose of our website,
cavalierhealth.org.
know
why. We think it is due to intellectual
laziness on the part of these cardiologists. Over the past few years,
taurine supplementation has been given a lot of publicity in cases of
another heart disease,
dilated cardiomyopathy (DCM). The headlines in veterinary newsletters
have screamed that DCM dogs may need taurine supplementation. But DCM and
MVD are totally unrelated disorders, and all veterinary cardiologists really
ought to know the difference between the two. But if the cardiologist's
attention span is so short that he does not dig any deeper than those
newsletter headlines, he remains ignorant about the distinctions between the
two disorders, and he passes his ignorance on to his MVD patients and their
owners as "professional advice". He prescribes synthetic taurine to treat
MVD, a disease that has nothing to do with taurine deficiency. In cases like
this, it is best that the dogs' owners be prepared in advance and know more than these lazy-minded
cardiologists. That is a purpose of our website,
cavalierhealth.org.
So, as promised, here are the details about veterinary research into MVD and taurine:
Research studies have shown that MVD-affected dogs tend to have higher plasma taurine concentrations than unaffected dogs. In a 1995 study (by board certified veterinary cardiologists George A. Kramer, Mark D. Kittleson, Philip R. Fox, Julia Lewis, and Paul D. Pion), for example, "[P]lasma taurine concentrations were highest in dogs with AVD [acquired valvular disease, e.g, MVD] ... We conclude that plasma taurine concentrations may be increased in dogs with AVD."
In a 2002 presentation, board certified veterinary cardiologist Bruce Keene stated:
"Taurine supplementation is indicated whenever plasma or whole blood taurine concentrations are found to be low. ... [S]upplementation is generally only recommended after discovery of deficiency."
In a March 2022 article, USA veterinary nutritionists and cardiologists recommended that taurine supplementation be administered only to dogs with plasma or whole blood taurine concentrations which were low or borderline.
In a September 2022 article, Texas A&M veterinary school researchers examined the levels of taurine concentration in the blood of 200 cavalier King Charles spaniels in various stages of mitral valve disease (MVD). Twelve were in Stage A (meaning no MVD murmur); 150 were in Stage B1 (murmur but no enlargement); and 38 were in Stage B2 (murmur plus enlargement). None were in Stages C or D (heart failure). They report finding that taurine concentrations in both plasma and whole blood were "not significantly different", regardless of the stage of MVD and also regardless of the type of food being fed to the dogs. They devised reference intervals for whole blood taurine (152 to 373 µM) and plasma taurine (51 to 217 µM) concentrations in cavaliers.
In a July 2023 article, a team USA researchers tested 14 dogs, including 4 (29%) cavaliers, diagnosed with congestive heart failure (CHF) due to MVD for a two-week period to see if taurine supplementation would suppress their renin-angiotensin-aldosterone system (RAAS). None of the dogs were taurine-deficient. They report finding that oral taurine supplementation did not have a suppressive effect upon the RAAS in this group of dogs with naturally occurring CHF secondary to MVD.
The Bottom Line: Taurine is not an appropriate supplement for MVD-diagnosed dogs unless taurine concentrations in the dogs' blood plasma has been found to be too low.
Links to the above cited veterinary journal articles are linked here.
RETURN TO TOP
February 8, 2026:
CKCSC,USA out snobs the UK Kennel Club
The USA cavalier club ranks coat color over health
 News Item: February 8, 2026: The Cavalier King Charles
Spaniel Club, USA (CKCSC,USA) issued this open letter to its members:
News Item: February 8, 2026: The Cavalier King Charles
Spaniel Club, USA (CKCSC,USA) issued this open letter to its members:
"The United Kingdom's registry, The Royal Kennel Club (formerly known as The Kennel Club) announce their [sic] intent to register Cavalier King Charles Spaniels in non-breed standard (NBS) colors. We want to be absolutely clear about the position of the Cavalier King Charles Spaniel Club, USA. We are firmly committed to the preservation and protection of our breed as defined by our club's official Breed Standard. Non-standard colors are not acceptable under our Breed Standard, and we do not recognize them for registration. The CKCSC,USA will only accept registrations for the four recognized, breed-standard colors: Blenheim, Tricolor, Black and Tan, and Ruby. Our ethical Guidelines require all members to breed toward the official Standard, prioritizing type, health, and temperament above all else. Our commitment to the integrity of the Cavalier King Charles Spaniel remains unwavering. Thank you for your continued dedication to our breed."
What apparently prompted the CKCSC,USA's letter to its members is a letter sent by the Royal Kennel Club (RKC) of the United Kingdom to the secretary to the Cavalier King Charles Spaniel Club of the UK earlier in February that the RKC intends to add 2 additional colors of cavaliers for registration purposes. The colors are Chocolate-&-Tan and Chocolate Tricolour. The club credits the fact that the chocolate (brown) color "has been widely known in the breed for a very long time", and that the American Kennel Club has been registering CKCSs of those colors for the past 25-30 years. The letter points out:
"There are no known health issues with the chocolate colour, and no indication that these colours are as a result of indiscriminate crossbreeding, and therefore there is no negative impact from a health perspective fore the breed as a whole."
CKCSC,USA combines snobbery and willful ignorance
Of course, all of this pretentious vanity displayed by the CKCSC,USA is pure genetic nonsense. The CKCSC,USA is prioritizing color above all else, at the expense of "type, health, and temperament". To this club, the most important things about a cavalier are what its color is and what its color is not. Ethics and integrity have nothing to do with it. Snobbery and willful ignorance best describe it.
We have seen this head-in-the-sand attitude displayed by the "leadership"
of the CKCSC,USA so many times in
 the
past when it comes to hereditary health issues of the breed, and now we see
it again. Rarely in the past has the CKCSC,USA shown any sense of
responsibility when it comes to dealing with severe medical problems. The
presidency of Anne Eckersley Robins is, of course, a shining exception, when
she led the efforts in 1998 to instate the Mitral
Valve Disease Breeding Protocol, albeit voluntary. The
only positive thing to say about the CKCSC,USA since then, when it comes to health
issues in general, is that the cavalier parent club of the American Kennel
Club -- the American Cavalier King Charles Spaniel Club -- and the AKC itself, have
been consistently far worse. The AKC and its ilk have no redeeming value
when it comes to health issues of the cavalier King Charles spaniel.
the
past when it comes to hereditary health issues of the breed, and now we see
it again. Rarely in the past has the CKCSC,USA shown any sense of
responsibility when it comes to dealing with severe medical problems. The
presidency of Anne Eckersley Robins is, of course, a shining exception, when
she led the efforts in 1998 to instate the Mitral
Valve Disease Breeding Protocol, albeit voluntary. The
only positive thing to say about the CKCSC,USA since then, when it comes to health
issues in general, is that the cavalier parent club of the American Kennel
Club -- the American Cavalier King Charles Spaniel Club -- and the AKC itself, have
been consistently far worse. The AKC and its ilk have no redeeming value
when it comes to health issues of the cavalier King Charles spaniel.
Historically, there have been more than just four colors
What are the other colors of cavaliers which the CKCSC,USA ostracizes? Here is a list of some, if not all, "off-colors":
• Brown-and-White (Chocolate and White)
• Black-and-White
• Brown (Chocolate)
• Brown-and-Tan (Chocolate and Tan)
• Black
• Black-and-Brown
 The documented history of this breed harks back at least to the toy
spaniels of the 1500s, before even the birth of King Charles I of England in 1600. In
that era in Great Britain, they were referred to simply as Toy Spaniels, and at
that time, they mainly came in two color combinations: Brown-and-White and
Black-and-White. By the time of King Charles II, the colors expanded by
adding the Tricolour, a combination of black, white, and reddish brown, and
what later would be called the Blenheim, reddish brown and white, as well as
a pure Black version. Later came the Black-and-Tan and the reddish Ruby and
the Brown and the Brown-and-Tan. This 1651 painting at the right is of King
Charles II of England, for whom the cavalier King Charles spaniel is named.
He is holding one of his brown-and-white toy spaniels, a color combination
banned by the CKCSC,USA as being "not acceptable".
The documented history of this breed harks back at least to the toy
spaniels of the 1500s, before even the birth of King Charles I of England in 1600. In
that era in Great Britain, they were referred to simply as Toy Spaniels, and at
that time, they mainly came in two color combinations: Brown-and-White and
Black-and-White. By the time of King Charles II, the colors expanded by
adding the Tricolour, a combination of black, white, and reddish brown, and
what later would be called the Blenheim, reddish brown and white, as well as
a pure Black version. Later came the Black-and-Tan and the reddish Ruby and
the Brown and the Brown-and-Tan. This 1651 painting at the right is of King
Charles II of England, for whom the cavalier King Charles spaniel is named.
He is holding one of his brown-and-white toy spaniels, a color combination
banned by the CKCSC,USA as being "not acceptable".
The blood and the genes of these off-colors are part of the foundation of the modern cavalier King Charles spaniel. Indeed, the off-colors preceded all 4 of the now "recognized" colors. When the breed known as the cavalier King Charles spaniel first was recognized in the United Kingdom in 1928, its original breed standard drawn up by the Committee of the Cavalier King Charles Spaniel Club stated: "Colour: All recognized".
Among the 18 cavaliers registered with the UK's club in May 1945 (following an hiatus during World War II), 2 were brown-&-whites and 1 was a black-&-white, comprising 17% of the registrations. And, these off-color cavaliers even were registered and shown in UK conformation shows as late as the 1970s. In 1971, Mrs. Amice Pitt of the UK club wrote of her preference for the now-recognized four color combinations, and since 1973 all CKCS breed standards have adhered to her choices. This decision appears to have been based solely upon a lady's personal preference without any thought of breed health consequences.
Off-color cavaliers have no unique health issues
Limiting the official, recognized coat colors to just those 4 in 1973 did not affect the genetic potential of the breed to continue to produce the off-color coats that had been in the breed for over 400 years. Since 1971, purebred cavaliers have been bred to other purebred cavaliers and have produced offspring of black-and-whites, brown-and-whites, brown-and-tans, and all blacks. Since these varieties are not eligible to compete in CKCS conformation events, most all breeders have tried to eliminate such genes from their breeding stock. In most all cases, they have been successful, so the production of off-color cavaliers today is quite rare. But such offspring are not inconceivable, and a few breeders still find off-colors among their litters.
Since our concern at CavalierHealth.org primarily is with the health of cavaliers, we have looked into whether any purebred off-colors are more or less vulnerable to the disorders known to affect the CKCS, or even if the off-colors tend to develop other diseases to which the recognized colors seem immune. We have found no such evidence. The only genetic differences between cavaliers of the recognized colored coats and the formerly recognized off-color coats are the colors of the coats. The recognized colors were chosen based solely upon the personal preference of Mrs. Pitt, and not due to any health issues whatsoever.
Eliminating coat colors may have spread CM and SM
Unfortunately, from a genetic health standpoint, the elimination of the off-colors has served as one more step in reducing the CKCS gene pool, which is very undesirable, as a general rule. In a September 2004 article, the investigators presented evidence that selection for coat color has not only narrowed the CKCS gene pool, but also has influenced the spread of Chiari-like malformation (CM) and syringomyelia (SM) throughout the breed.
It may be too late to rescue the CKCS breed from the deleterious health effects resulting from the clubs' efforts to eliminate the off-colors, but it is not too late to add them again. Considering that the only alternative approach to refreshing the gene pool has been to crossbreed with other breeds and then backcross, the insertion of off-color purebred cavaliers certainly is a less risky method of refreshing the gene pool. Wisely, at least the Royal Kennel Club (RKC) of the United Kingdom now has reversed that policy, in order to widen the CKCS's gene pool.
RETURN TO TOP
February 1, 2026:
Why Social Media Veterinary Pill
Merchants should be ignored
They don't examine, diagnose, or treat.
They just want to sell you stuff.
 Social Media Veterinary Pill Merchants are veterinarians who have
followings on social media platforms but who do not actually examine dogs as
patients. They should be ignored when they try to sell you something. Why?
Because unless they have examined your dog as their patient, they have no
valid basis for recommending any treatments which they want you to buy from
them. As board certified veterinary
neurologist and holistic vet Dr. Curtis Dewey wrote recently:
Social Media Veterinary Pill Merchants are veterinarians who have
followings on social media platforms but who do not actually examine dogs as
patients. They should be ignored when they try to sell you something. Why?
Because unless they have examined your dog as their patient, they have no
valid basis for recommending any treatments which they want you to buy from
them. As board certified veterinary
neurologist and holistic vet Dr. Curtis Dewey wrote recently:
"I won't give specific advice for any dog that I have not physically examined. No veterinarian should."
To do otherwise is an abuse of veterinary ethics, if not brazen hypocrisy. As an example, one of these Social Media Veterinary Mavens advertises on her social media platforms, to any and all dog owners, a wide variety of dog foods and recipes which she says she has formulated. And yet, she piously claims in one of her own YouTube videos that:
"I will not formulate a diet for somebody unless I've seen all the veterinary records and I've gone through them and I know what it is that we're dealing with."
So, which version of her should we believe? When Social Media Veterinary Mavens blatantly contradict themselves like that, their underlying reason usually is a conflict of interest between obvious good advice and wanting to sell the products on their warehouse shelves.
A worse example is that this same Social Media Veterinary Maven self-published a book of 60
dog food
 recipes, of which all but one of them, she finally confessed 8
years later, "is not 100% complete and balanced"
because their ingredients lists do not include any calcium, a vital supplement to
any dog food recipe. Mind you, this is a lady who claims to be a certified
food therapist. Dietary calcium insufficiency is a common and dangerous
consequence of not adding appropriate quantities of digestible calcium to
each meal.
Dogs die from it. While she finally has admitted, after years and
years of vigorously promoting her book, that 59 of its 60 recipes
do
not include any calcium at all among their listed ingredients, she persists in
offering the book for sale on her website and on
Amazon. Read the
details of why calcium supplementation is essential in all dog foods,
at this link.
recipes, of which all but one of them, she finally confessed 8
years later, "is not 100% complete and balanced"
because their ingredients lists do not include any calcium, a vital supplement to
any dog food recipe. Mind you, this is a lady who claims to be a certified
food therapist. Dietary calcium insufficiency is a common and dangerous
consequence of not adding appropriate quantities of digestible calcium to
each meal.
Dogs die from it. While she finally has admitted, after years and
years of vigorously promoting her book, that 59 of its 60 recipes
do
not include any calcium at all among their listed ingredients, she persists in
offering the book for sale on her website and on
Amazon. Read the
details of why calcium supplementation is essential in all dog foods,
at this link.
Interestingly, she
also claims to be the "top holistic veterinarian of the decade", and yet she has
not practiced clinical
 veterinary medicine for over 5 years, and even back then her
holistic certifications (only the basics: "acupuncturist, chiropractitioner, and food
therapist") were very limited. A "top holistic veterinarian" should at least
also be certified in herbal medicine, homeopathy, and homotoxicology.
veterinary medicine for over 5 years, and even back then her
holistic certifications (only the basics: "acupuncturist, chiropractitioner, and food
therapist") were very limited. A "top holistic veterinarian" should at least
also be certified in herbal medicine, homeopathy, and homotoxicology.
So, she does not examine, diagnose, or treat patients, holistically or otherwise. And, again, she warns that every dog must be treated individually by its hands-on veterinarian. She said recently:
"VERY, VERY CRITICAL! TREAT THE PET IN FRONT OF YOU!" If your pet is having a problem or an illness, it is so important that your individual pet is being treated as an individual. ... It is really important that your pet is treated as an individual, and that you are treating the animal in front of you! Your pet may not have the exact same symptoms as every pet with this problem. Your pet may have multiple comorbidities. We want to make sure that the pet is being treated for exactly what they [sic] are presenting with, not what the general population presents with. Very, very critical! Treat the pet in front of you! If they're acting sick, let's get to the bottom of it." (Emphasis in original.)
 Nevertheless,
she peddles a warehouse full of "holistic" treatments -- regardless of
whether there is any published veterinary research supporting their
effectiveness -- to unsuspecting dog owners, but she has not examined any of those
customers' dogs.
Nevertheless,
she peddles a warehouse full of "holistic" treatments -- regardless of
whether there is any published veterinary research supporting their
effectiveness -- to unsuspecting dog owners, but she has not examined any of those
customers' dogs.
At times, she even touts her personal experience with a supplement as being superior evidence to contradictory peer-reviewed published research. For example, here is the only authority she cites when advertising "Dr. Judy's PEA" (palmitoylethanolamide):
"I started using it with my own cavaliers and I was so impressed by the results that I decided to make human grade, high quality PEA available for other pets."
See this link for the low-down on PEA and how veterinary research has found it essential for PEA to be ultramicronized to be effectively utilized in the dog's body at all. Is her PEA product ultramicronized? Here is what she has to concede:
"If you are looking at the research, you often are going to see that ultramicronized PEA is used and recommended, and we are often asked if Dr. Judy's PEA, the product we have on our website, is ultramicronized. The answer is no."
 So, not only does she
not cite veterinary research to support her version of
PEA, but she ranks her anecdotal opinion over and above the scientific veterinary research that
contradicts her. Again, which version of her should we believe?
So, not only does she
not cite veterinary research to support her version of
PEA, but she ranks her anecdotal opinion over and above the scientific veterinary research that
contradicts her. Again, which version of her should we believe?
So, keep in mind the adage, "BUYER BEWARE!"
RETURN TO TOP
December 7, 2025:
Entresto (sacubitril/valsartan) for treating
canine myxomatous mitral
valve disease
What we know thus far. What may be coming next.
 Entresto
is a prescription oral tablet which the U.S. Food & Drug Administration
(FDA) approved for treating humans in 2015 to reduce the risk of cardiac
death in patients with chronic heart failure and reduced ejection
fraction. The drug has been found to reverse heart enlargement, reduce
inflammation of the heart, and enable lower diuretic doses in humans.
Entresto's primary medical purpose is to suppress the
kidneys' rein-angiotensin-aldosterone sytem
(RAAS), which in turn, has these beneficial effects.
Entresto
is a prescription oral tablet which the U.S. Food & Drug Administration
(FDA) approved for treating humans in 2015 to reduce the risk of cardiac
death in patients with chronic heart failure and reduced ejection
fraction. The drug has been found to reverse heart enlargement, reduce
inflammation of the heart, and enable lower diuretic doses in humans.
Entresto's primary medical purpose is to suppress the
kidneys' rein-angiotensin-aldosterone sytem
(RAAS), which in turn, has these beneficial effects.
Beginning in 2014, Entresto has been studied as a possible medication for treating dogs diagnosed with myxomatous mitral valve disease (MVD) in its late stages -- Stages C and D -- along with other MVD medications, pimobendan (Vetmedin) and diuretics.
Entresto is a combination of sacubitril and valsartan, and its generic name, appropriately, is sacubitril/valsartan (S/V)*. Sacubitril blocks the enzyme neprilysin, which otherwise interferes with beneficial natriuretic peptides which relax blood vessels and allow fluids and sodium to be excreted in the urine. Valsartan blocks the hormone angiotensin II, which otherwise would cause the narrowing of blood vessels and higher blood pressure. Combined, S/V significantly reduces aldosterone (ALD), a hormone that is involved in regulating blood pressure and levels of sodium and potassium in the blood. Aldosterone also is one of the major players in the RAAS, which when activated narrows the blood vessels and causes the kidneys to retain water and sodium, thereby increasing the amount of fluid in the dog's body and raising its blood pressure, when the best interests of the MVD-affected dog is to remove water and sodium from the body. Read more about the RAAS here.
* Many generic versions of S/V are available. Other brand names for S/V include Sacufox V, Vymada, Azmarda, Sacuvia, Scabutor, and its original code name, LCZ696.
Studies conclude S/V benefits the kidneys
Early canine studies of S/V focused upon its effect on the kidneys of MVD-affected dogs, since the components of S/V are blockers of the enzymes and hormones comprising the RAAS. Overall, they have found that S/V benefited the kidneys and did not cause damage to them. The downside of all of these studies is the few numbers of dogs tested, making them "pilot studies", meaning, hopefully leading the way to future follow-up studies with many more dogs participating. Thus far, none have been reported.
The earliest canine study of S/V was an April 2014 poster presentation before the American College of Cardiology by Dr. Jonathan Mochel and others. They reported on their comparison cross-over study of LCZ696 (the original code name of S/V), and valsartan alone, and the ACE-inhibitor benazepril, and a placebo on 18 RAAS-affected beagles for 10 days. The dosages of LCZ696 were 15 and 45 mg/kg. The aim was to determine reduction in aldosterone (ALD) exposure. They found that, compared to placebo, benazepril modestly reduced ALD, and valsartan and LCZ696 decreased ALD levels to a significant extent. The greatest reductions were observed in the LCZ696 groups, with LCZ696 at 2 hours reducing ALD 2-fold lower than valsartan.
In an August 2018 article, a team of Auburn University veterinary researchers examined the effectiveness of S/V in 7 dogs diagnosed with MVD, compared to 6 MVD-affected dogs in the placebo group. They reported finding that S/V is effective at lowering the urine concentration of aldosterone and that it was safe, with no deleterious effects on BUN, creatinine, and electrolyte concentrations, or systolic arterial pressure.
In a February 2019 article, the investigators compared the effects of S/V versus just valsartan, and versus benazepril, on the dynamics of the renin-angiotensin-aldosterone system (RAAS) and the natriuretic peptides (NP) system in 18 laboratory beagles after activating their RAAS with a low-salt diet over 15 days. They reported:
"In conclusion, the ARNI sacubitril/valsartan reduced ALD [aldosterone], a known risk factor of CV [cardiovascular] mortality, and enhanced the NP [natriuretic peptides] system via cGMP-mediated pathways in a low-sodium diet model of RAAS activation. The results presented herein provide further evidence that the effects on the renin cascade extend to reduced ALD levels beyond that achieved with RAAS blockade alone. These positive findings in dogs also suggest that sacubitril/valsartan is a promising pharmacological candidate for increased survival in canine cardiovascular diseases." (Emphasis added.)
In a November 2020 article, 7 dogs in which cardiorenal syndrome (CRS) was induced, resulting in heart failure and renal dysfunction, were treated with S/V for 3 months and compared to 7 other dogs in a control group. The investigators reported that the S/V improved left ventricle systolic function and mitochondrial function and decreased biomakers of heart and kidney injury.
In a June 2024 article, Japanese resaerchers studied the effects of S/V on the kidneys of 5 healthy laboratory dogs. They were given oral doses of 20 mg/kg. twice a day for 4 weeks. Kidney blood flow (renal hemocynamics) was assessed before the first dose and then on days 7 and 28. They report finding that S/V "may enhance renal haemodynamics in healthy dogs." Translated, this means S/V may improve the blood flow through the kidneys.
S/V has reversed MVD progression in Stage C dogs
The S/V research that has focused upon MVD in dogs has been more limited and mainly comparing S/V's effectiveness to that of ACE-inhibitors (e.g., benazepril, enalapril, ramipril). ACE stands for angiotensin-converting enzyme, and its activation causes the MVD-dog's blood vessels to tighten, thereby reducing the flow of blood and oxygen to the heart. An ACE-inhibitor is intended to prevent ACE from narrowing the blood vessels and reducing blood flow. However, for cavalier King Charles spaniels in particular, ACE-inhibitors have been found to be ineffective in dealing with MVD because they have a mutation of an ACE gene. Read more about ACE-inhibitors here. Again, these studies and the number of dogs in them have been very limited.
In a July 2021 article, Thai investigators compared S/V with the ACE-inhibitor ramipril in treating dogs diagnosed with Stage C (heart failure) due to MVD, along with both pimobendan and the diuretic furosemide. Twenty-one dogs -- none being cavaliers -- were divided into the S/V group (11 dogs) and the ramipril group (10 dogs) for four weeks. The investigators report that short-term administration of SV in dogs with MVD stage C resulted in a greater extent of reverse myocardial remodeling of both the left atrium and the left ventricle than in the ramipril group, as indicated by several echocardiographic parameters. They concluded:
"The current study suggested that the short-term effects of SV can reverse myocardial remodeling, as inferred from several echocardiographic indices (i.e., the reduction in LA/Ao, LVIDDN, EDVI and ESVI) in dogs with MMVD stage C. These findings would support the use of SV in clinically symptomatic heart failure in dogs." (Emphasis added.)
However, they warn of a few limitations: (a) a very small sample size, with a much larger sample size needed to confirm the findings; (b) the study was for a very short term -- four weeks -- and a longer term study should be conducted; (c) the results thus far "do not suggest that ACEi should be replaced with S/V in dogs with MMVD stage C."
 At
the June 2025 ACVIM Forum, board certified veterinary cardiologist Dr. Justin Carlson
(right) presented
a lecture, "Beyond the Guidelines: Sacubitril/Valsartan (ARNi)
(Entresto)", in which he reported on 49 case studies of
MVD-affected dogs in late Stage C or Stage D ("pretty bad cases that I thought were not
going to do very well"), 7 of which were cavalier King Charles spaniels
(and 7 Maltese and 6 Yorkies). Among those 49 patients in which he
substituted S/V for an ACE-inhibitor
(such as benazepril or enalapril) and spironolactone, their mean
survival time was 474 days, with a median of 381 days, and an
overall survival range from 152 to 1,989 days. He compared those results
to those of the
VALVE Study trial and the
QUEST Study. In the VALVE Study of Stage C dogs (in which the
ACE-inhibitor ramipril was added to the combination of furosemide and
pimobendan), the median survival time was only 214 days.
In the QUEST Study (in which Stage C dogs received either pimobendan or
benazepril), the median survival time was only 267 days
for pimobendan alone. He emphasized that the patients in his group of 49
dogs being treated with Entresto were late Stage C or Stage D dogs,
meaning that they were in far worse shape than the Stage C dogs just
developing heart failure which were the subjects of the VALVE and QUEST
studies.
At
the June 2025 ACVIM Forum, board certified veterinary cardiologist Dr. Justin Carlson
(right) presented
a lecture, "Beyond the Guidelines: Sacubitril/Valsartan (ARNi)
(Entresto)", in which he reported on 49 case studies of
MVD-affected dogs in late Stage C or Stage D ("pretty bad cases that I thought were not
going to do very well"), 7 of which were cavalier King Charles spaniels
(and 7 Maltese and 6 Yorkies). Among those 49 patients in which he
substituted S/V for an ACE-inhibitor
(such as benazepril or enalapril) and spironolactone, their mean
survival time was 474 days, with a median of 381 days, and an
overall survival range from 152 to 1,989 days. He compared those results
to those of the
VALVE Study trial and the
QUEST Study. In the VALVE Study of Stage C dogs (in which the
ACE-inhibitor ramipril was added to the combination of furosemide and
pimobendan), the median survival time was only 214 days.
In the QUEST Study (in which Stage C dogs received either pimobendan or
benazepril), the median survival time was only 267 days
for pimobendan alone. He emphasized that the patients in his group of 49
dogs being treated with Entresto were late Stage C or Stage D dogs,
meaning that they were in far worse shape than the Stage C dogs just
developing heart failure which were the subjects of the VALVE and QUEST
studies.
Dr. Carlson said that the owners of 39 of his 49 patients (80%) reported their dogs had noticeably improved energy levels. The owners of 28 of the dogs (57%) reported that their dogs were coughing less. He found that "in a lot of these dogs", the S/V allowed for the safe reduction of diuretics, and in "a handful of these dogs", he has since stopped any diuretic medications, and "they are doing great." He reported that, over time, there was "a statistically significant difference" in the sizes of the left ventricle and left atrial ratio. He found in some dogs that over time their left atriums were back to normal in size.
As for adverse effects, he had only 2 of the 49 dogs with gastrointestinal distress. As for renal values, only one patient had significant worsening renal values, with 3 having increased azotemia in 4 months and 5 having significantly decreased renal values after 4 months. Regarding survival times, the mean survival time was 474 days, with a median of 381 days , and a range from 152 to 1,989 days. He pointed out that in the VALVE Study trial, in which an ACE-inhibitor (ramipril) was added to the combination of furosemide and pimobendan, the median survival time was only 214 days, and in the QUEST Study (in which the Stage C dogs received either pimobendan or benazepril), the median survival time was only 267 days for pimobendan. He emphasized that the patients in his group of dogs being treated with Entresto were Stage D dogs.
Dr. Carlson recommends "up-titration" of dosages of S/V, meaning
starting at a low dosage and then increasing
 it, over 2 to
6 weeks,
depending upon the dog's response and the blood test results. He stops
both ACE-inhibitors and spironolactone when he starts the S/V, waiting
36 hours. His recommended dosage range is 15-30 mg/kg twice a day.
it, over 2 to
6 weeks,
depending upon the dog's response and the blood test results. He stops
both ACE-inhibitors and spironolactone when he starts the S/V, waiting
36 hours. His recommended dosage range is 15-30 mg/kg twice a day.
In a paper presented at the 2025 ACVIM Forum, cardiologists Ryan Fries, Elizabeth Malcolm, Sonya Gordon, and Justin Carlson wrote:
"When utilizing Entresto in a group of canine patients (n=49) with congestive heart failure secondary to myxomatous mitral valvular disease or dilated cardiomyopathy, Entresto was well tolerated, with fewer than 5% of patients having undesirable side effects when titrated appropriately. While a FETCH questionnaire was not completed on patients, there was an overwhelming owner-noted improvement to the patients' quality of life when optimal dosing of Entresto was achieved based on owner report history during follow-up. Up-titration of the medication was done over the span of 1-6 weeks in most patients, with some patients requiring an extended up-titration over multiple months. Survival, echocardiographic, and dose-response data will be presented in a future manuscript. Based on the encouraging data from this cohort of patients, the optimal dosing, timing of up-titration, and ideal start time in patient disease stage warrant further study in a prospective manner."
As noted above, the FDA approved S/V for humans in 2015 to reduce the risk of cardiac death in patients with chronic heart failure. Valsartan (Diovan) alone had been approved by the FDA in 2002 for treating humans of heart failure. FDA approval of S/V for humans was based upon a study (PARADIGM-HF) comparing it to enalapril in 8,442 patients with symptomatic chronic heart failure and systolic dysfunction. Studies of humans recommend up-titration from the lowest dose to the highest tolerable dose over periods of 2 to 4 weeks. It is for these reasons that veterinary cardiologists in general prefer to wait until the MVD-affected dog is well into heart failure (Stage C) or even in Stage D before starting S/V, and for up-titrating the dosages.
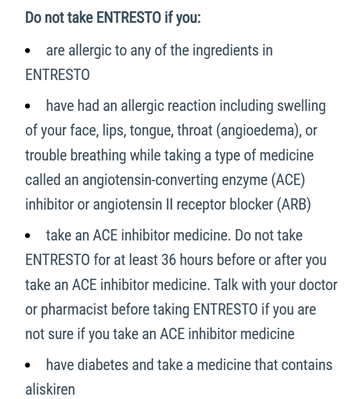 The maker of Entresto warns humans that
ACE-inhibitors (e.g.,
enalapril, benazepril, etc.) should not be taken in
addition to S/V. (See excerpt at right.) ACE-inhibitors
should be discontinued at least 36 hours before starting S/V, and
some veterinary cardiologists recommend a "wash out period" of as long
as 72 hours before starting S/V.
The maker of Entresto warns humans that
ACE-inhibitors (e.g.,
enalapril, benazepril, etc.) should not be taken in
addition to S/V. (See excerpt at right.) ACE-inhibitors
should be discontinued at least 36 hours before starting S/V, and
some veterinary cardiologists recommend a "wash out period" of as long
as 72 hours before starting S/V.
Reported side effects of S/V in humans include:
• Diarrhea
• Vomiting
• Drop in blood pressure
• Weakness
• Difficulty standing
Despite the lack of any published studies of S/V beyond the pilot level of very few dogs, some veterinary cardiologists have begun to prescribe S/V to MVD-affected dogs in late Stage C and Stage D. They typically call for blood tests within 10 to 14 days following commencement of the treatment, due mainly to concerns about the kidney levels, even though the above referenced studies have found no significant renal problems caused by the drug.
Rarely do veterinary cardiologists reportedly begin treating MVD with S/V prior to the patients reaching congestive heart failure, Stage C, and in most cases not before late in Stage C or even Stage D, refractory heart failure. There are at least 4 reasons for not rushing to prescribe S/V earlier in the progression of MVD:
(1) While in its earlier stages, MVD can activate the RAAS, the RAAS becomes most active and hazardous once the MVD reaches Stage C;
(2) In humans, the studies have been of patients already in heart failure;
(3) The only published study of MVD-affected dogs in Stage B2 (heart enlargement but no heart failure) thus far has been the 2018 Auburn Univ. study of 7 dogs, which focused upon the effect of S/V upon the dogs' RAAS; and
(4) Early administration of another MVD drug, pimobendan, have been found in some cases to accelerate the progression of MVD, even to the point of death. As a pointed example, during the 2016 EPIC Study of treating MVD dogs in Stage B, 8.4% of those dogs in the pimobendan group died of cardiac-related deaths prior to reaching Stage C.
 Nevertheless,
Dr. Fries (right) explained during a Zoom presentation in February
2026 that he also prescribes Entresto for dogs in Stage B2 if their heart
chambers are enlarging rapidly and appear close to the onset of Stage C. He
said:
Nevertheless,
Dr. Fries (right) explained during a Zoom presentation in February
2026 that he also prescribes Entresto for dogs in Stage B2 if their heart
chambers are enlarging rapidly and appear close to the onset of Stage C. He
said:
"In our practice, we use it under two conditions most commonly. The first one is, a dog has gone into heart failure, and we believe there is going to be benefit from this drug. So the combination of sacubitril and valsartan, the RNI combination, we're going to inhibit neprilysin and help the body produce its own natriuretic peptides to combat heart failure. And then combat the RAAS system with an angiotensin receptor blocker. So, we believe that there is good evidence to say it's going to be helpful in heart failure. And now that it is generic, and with GoodRx, you can find it for very reasonable prices now. So, I think we prescribe it pretty regularly. The other time that we prescribe it is for dogs who are showing clear, obvious progression, so their hearts are getting larger every month or two or six months, even on something like pimobendan, or they have really severe cardiomegaly already. Even though they are not in heart failure, we think it's imminent, then we would also recommend it at that point. I don't have any strong beliefs about starting it early, like early B2; definitely not B1 at this point. So I think all of those questions will be answered in time, but right now, there's really strong evidence to say heart failure, yes, lots of dogs benefit from it, with very few, almost no side effects that we've seen clinically. You know, azotemia, things like that, we haven't really appreciated that at all."
Anecdotal reports from the owners of MVD-affected dogs being given S/V almost uniformly are positive. They observe that their dogs' energy levels immediately are much higher, that their respiratory rates have dropped from the high 20s and 30s per minute down to the mid-teens, and that their cardiac coughs have diminished -- a sign that the dogs' left atriums may had shrunk. Post-treatment radiographs and echocardiograms confirm reduced heart chamber sizes.
We look forward to the soon-to-be-published article by Drs. Fries,
Malcolm, Gordon, and Carlson. While their
 report may be limited to their
patients' case studies, it is not reasonable to expect the owners of
severely affected MVD-dogs to wait any longer for this apparently very effective drug
to become more widely prescribed. Cardiologists all over are feeling that
pressure from their clients. For a drug like S/V, it is asking way too
much for cardiologists to insist upon awaiting publication of some
not-yet-scheduled future, randomised, double-blinded,
placebo-controlled, long term, cross-over, peer-reviewed study with hundreds of dogs in each cohort,
before being able to prolong the lives of our MVD-affected dogs.
report may be limited to their
patients' case studies, it is not reasonable to expect the owners of
severely affected MVD-dogs to wait any longer for this apparently very effective drug
to become more widely prescribed. Cardiologists all over are feeling that
pressure from their clients. For a drug like S/V, it is asking way too
much for cardiologists to insist upon awaiting publication of some
not-yet-scheduled future, randomised, double-blinded,
placebo-controlled, long term, cross-over, peer-reviewed study with hundreds of dogs in each cohort,
before being able to prolong the lives of our MVD-affected dogs.
What benefits may we expect from S/V?
S/V does not affect the underlying cause of MVD in dogs. It does not prevent the deterioration of the mitral valve leaflets and chordae, and it does not prevent the backflow of blood through that valve -- mitral regurgitation. So, S/V is not a preventative of or a cure for MVD.
S/V does, however, enable the heart and the kidneys to better compensate for the damaging effects of MVD. At its most effective, we may expect S/V to keep more blood and oxygen flowing from the left ventricle through the blood vessels to the rest of the body, and also reverse the enlargement of the heart. Thereby, less blood may backflow through the mitral valve into the left atrium, and less to no fluid from the left atrium into the lungs. This could mean that the MVD-dog in heart failure (Stages C and D) may need lower or even no doses of diuretics, thus avoiding the harmful effects upon the kidneys that those diuretics cause. The MVD-dog still will need pimobendan, as long as the dog tolerates it. In short, if S/V does these things, it could significantly prolong the life of the MVD-affected dog and provide a far higher quality of that life. However, despite the benefits that S/V may provide, it will not prevent the continued deterioration of the mitral valve, and for dogs with severe MVD, the disease ultimately will kill the patient.
There is a Facebook group, Entresto for dogs with CHF/MVD - sharing stories and what we have learned, which consists of hundreds of members who discuss their dogs' experiences with S/V.
RETURN TO TOP
November 18, 2025:
Artificial Intelligence (AI) is an oxymoron. It definitely is "artificial", but it definitely also IS NOT "intelligent".
AI does not filter out Internet falsehoods from facts
 BEWARE
OF ARTIFICIAL INTELLIGENCE when seeking information on the Internet about the health of your
cavalier King Charles spaniels! Artificial Intelligence (AI) is an oxymoron.
It definitely is "artificial", but it definitely also IS NOT "intelligent".
BEWARE
OF ARTIFICIAL INTELLIGENCE when seeking information on the Internet about the health of your
cavalier King Charles spaniels! Artificial Intelligence (AI) is an oxymoron.
It definitely is "artificial", but it definitely also IS NOT "intelligent".
AI only knows what it picks up from the Internet. It sucks up trillions of bits of data on-line, but it does not filter out falsehoods from facts. And, when AI does not know the answer to your question, it makes up a phony answer. Because, AI never wants to admit it doesn't have an answer. It never wants to say "I don't know." Its fear is that if it tells you it does not know the answer to your question, you will go search elsewhere among all of the AI sources and never return again.
So, when using AI to get answers about the health issues of cavalier King Charles spaniels, there is a very good chance it will lie to you. AI even has a name for its lies -- HALLUCINATIONS!

RETURN TO TOP
November 17, 2025:
Coughing is NOT a sign of heart failure
in dogs with mitral valve
disease
 Most dogs
diagnosed with mitral valve disease (MVD) which develop a cough are not yet in heart
failure. Unfortunately, far too many veterinarians ignorantly
assume that a dry, hacking cough necessarily means that the dog has
reached the stage of congestive heart failure (CHF -- Stage C). They call it a "cardiac
cough" and attribute it to fluid build-up in the lungs due to CHF
(pulmonary edema).
Most dogs
diagnosed with mitral valve disease (MVD) which develop a cough are not yet in heart
failure. Unfortunately, far too many veterinarians ignorantly
assume that a dry, hacking cough necessarily means that the dog has
reached the stage of congestive heart failure (CHF -- Stage C). They call it a "cardiac
cough" and attribute it to fluid build-up in the lungs due to CHF
(pulmonary edema).
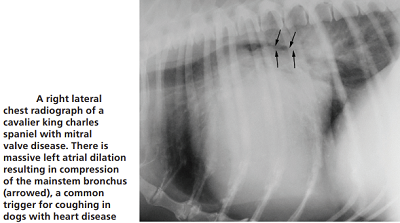
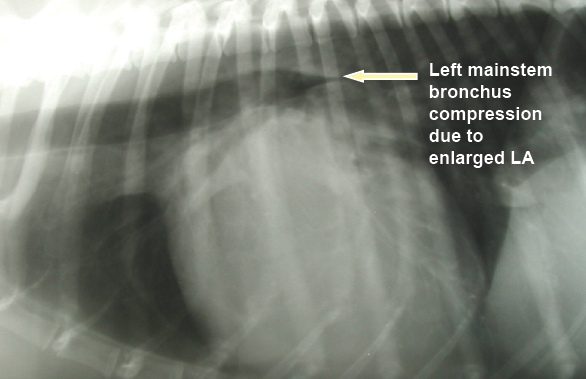
In most cases (roughly 70%), however, the term cardiac cough is a misnomer because the true cause of the cough probably is respiratory related and completely independent of any heart disorder. If the cough is related to the dog's MVD at all, it is due to the enlarged left atrium of the heart compressing against the dog's airway -- its bronchus or its trachea (see x-ray images above and below).
One of the most common -- and potentially dangerous -- misjudgments some veterinarians tend to make is to assume that such a cough indicates the onset of CHF and the need for immediate treatment with a diuretic. Cardiologist Dr. Michele Borgarelli has warned:
"It should be stressed that cough is a general clinical sign of respiratory disease and its presence in a dog with a murmur is not an indicator for starting treatment for CHF."
In a July 2025 article, authors Drs. Melanie J. Hezzell and Adrian Boswood concur, stating: "Stage B2 dogs may show signs of coughing, which appears to be more likely in dogs with cardiac enlargement." (See the x-ray image below, in which the enlarged left atrium, outlined in red, is pressing against the dog's airway, the black tube.)
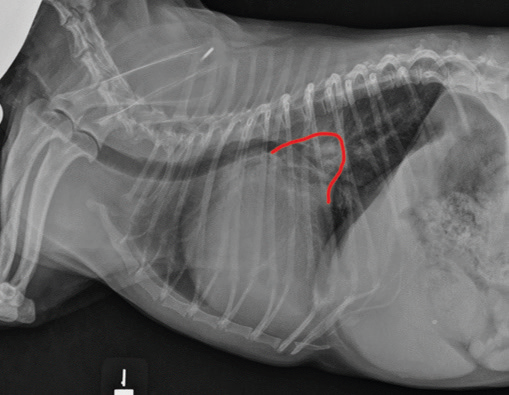 The cough could be due to a combination of factors, which include the
enlarged left atrium of the heart pressing against and compressing the
left mainstem bronchus or trachea, but more likely to airway disorders independent
of any relationship with the heart, such as bronchomalacia and airway
inflammation (possibly with the large left atrium merely highlighting
the bronchial narrowing). It may even cause the trachea to
collapse. However, if the dog coughs up a
pink-tinged fluid, it would indicate that may have very severe pulmonary
edema which is filling the airways. This would occur very late in the
Stage C of MVD, and not at the onset of fluid from the heart entering
the lungs.
The cough could be due to a combination of factors, which include the
enlarged left atrium of the heart pressing against and compressing the
left mainstem bronchus or trachea, but more likely to airway disorders independent
of any relationship with the heart, such as bronchomalacia and airway
inflammation (possibly with the large left atrium merely highlighting
the bronchial narrowing). It may even cause the trachea to
collapse. However, if the dog coughs up a
pink-tinged fluid, it would indicate that may have very severe pulmonary
edema which is filling the airways. This would occur very late in the
Stage C of MVD, and not at the onset of fluid from the heart entering
the lungs.
In a January 2019 article, Drs. Luca Ferasin and Chris Linney concluded that a cough in the absence of rapid and labored breathing would indicate that it is due mainly to a respiratory disease rather than a cardiac disease. They explain that coughing is a hallmark sign of bronchitis. They stated, dogs with severe pulmonary edema can cough but coughing is much more common with primary lung disease. By severe pulmonary edema, they said they mean that the fluid has completely filled the lungs and also has started to fill the upper airway passages, as well. (The x-ray below shows the heart's enlarged left atrium impinging upon the left main bronchus.). Dr. Ferasin concluded:
"The obsolete concept of cough caused by pulmonary oedema has been handed down for decades without any solid scientific evidence but merely based on the observation that dogs with cardiac disease often cough."
Most recently, in an October 2025 article, veterinary cardiologists Drs. Mark Rishniw, Michele Borgarelli, Luca Ferasin (again), and Giulio Menciotti examined the effect of left atrial (LA) size and presence or absence of CHF in small-breed dogs with MVD on the probability of coughing. They hypothesized that coughing probability would increase with increasing left atrial enlargement but not with CHF. They examined the records of 352 dogs with varying degrees of LA enlargement, up to severe enlargement. They report finding that only severe LA enlargement resulted in an increased probability of coughing in MVD-affected dogs. They further found that CHF was not an independent predictor of coughing. They concluded that they found no evidence that CHF contributes to or increases the probability of coughing in dogs with MVD and that severe LA enlargement does increase this probability. They urged that clinicians should not include coughing (or its absence) when considering whether dogs with MVD have CHF or not. Specifically, they stated:
"Our study should dispel the idea that pulmonary edema causes coughing in dogs with mitral valve disease -- indeed, clinicians should ignore the presence of coughing when making a diagnosis of CHF in dogs with mitral valve disease. Specifically, clinicians cannot make the assumption that a coughing dog with a murmur has CHF -- a diagnostic error that clinicians in first-opinion practice often make."
So if a dog has had a cough for months and unchanged and the dog is not being treated with a diuretic, the cough is very unlikely due to heart failure.
For more detailed information about this topic, see our MVD webpage at "coughing is not a symptom of CHF".
RETURN TO TOP
October 29, 2025:
Toothless cavalier King Charles spaniels are disabled dogs
Eating, drinking, and medicating
can be more complicated
 Cavalier
King Charles spaniels are more susceptible to a dental and gum and bone-loss
disorder called periodontal disease (PD) than most
any other dog breeds. While PD is the most commonly diagnosed disease in
dogs, the CKCS suffers from an earlier-onset version in which the the gums
recede and the tooth roots become exposed as early as two years of age. PD
is more prevalent in the CKCS than in any other breed. Read more about PD in
the cavalier at this webpage.
Cavalier
King Charles spaniels are more susceptible to a dental and gum and bone-loss
disorder called periodontal disease (PD) than most
any other dog breeds. While PD is the most commonly diagnosed disease in
dogs, the CKCS suffers from an earlier-onset version in which the the gums
recede and the tooth roots become exposed as early as two years of age. PD
is more prevalent in the CKCS than in any other breed. Read more about PD in
the cavalier at this webpage.
Apart from the cavalier's breed-specific causes of the onset of tooth and gum disease, studies have attributed causes to include feeding dry dog foods (kibble), bone chewing, and the lack of daily brushing of the dog's teeth. In a February 2024 article, for example, the author reported finding "a trend among dogs being fed dry foods to develop periodontal disease." She also stated that "Regular dental brushing has been found to support significant treatment in patients who are still in the early stages of the disease."
Nevertheless, despite how much daily care many cavaliers' teeth may receive, most all of them will lose some of their teeth to PD over time, and a high percentage of those will become totally toothless. Periodic veterinary teeth and gum cleaning procedures not only clean the teeth, but they end up also having to remove decaying teeth. When you see a cavalier with its tongue hanging out of the side of its mouth, that usually means the dog no longer has any teeth.
Toothless dogs are disabled dogs. There are several things that a
toothless dog no longer can do, at least very
 well.
Obviously, the toothless dog cannot chew its food. This means that its diet
must accommodate its lack of teeth. Ideally, the toothless dog's food should
be well ground and wet. Dry foods (kibble) and chunks of raw meats, or even
cooked chunks of meats, can cause swallowing problems for toothless
dogs. Kibble can cause lesions in the toothless dog's mouth that must be treated with
antibiotics. The meats and vegetables should be fresh and moist, and well ground. So, canned
or frozen wet foods, well ground, are the safest types of food to feed these
dogs. If the food is homemade, all of the ingredients should be fairly
finely ground.
well.
Obviously, the toothless dog cannot chew its food. This means that its diet
must accommodate its lack of teeth. Ideally, the toothless dog's food should
be well ground and wet. Dry foods (kibble) and chunks of raw meats, or even
cooked chunks of meats, can cause swallowing problems for toothless
dogs. Kibble can cause lesions in the toothless dog's mouth that must be treated with
antibiotics. The meats and vegetables should be fresh and moist, and well ground. So, canned
or frozen wet foods, well ground, are the safest types of food to feed these
dogs. If the food is homemade, all of the ingredients should be fairly
finely ground.
 Toothless dogs become sloppy eaters. A fair amount of food in the bowl
will end up on the floor. Eventually the dog with get back to that food, but
placing the bowl on a small tray (see image at right) will prevent the food from
getting on the floor and avoid contamination.
Toothless dogs become sloppy eaters. A fair amount of food in the bowl
will end up on the floor. Eventually the dog with get back to that food, but
placing the bowl on a small tray (see image at right) will prevent the food from
getting on the floor and avoid contamination.
Toothless dogs take longer to finish eating their meals. The owner needs to be patient with the toothless dog at mealtime. The dog is trying its best, but not every lick of its tongue successfully picks up the food it is aiming for.
Toothless dogs have problems taking medications, especially pills. Often
the pill placed in the dog's mouth will
pop
out again. So care must be taken to assure that when the toothless dog is
given its medications, it indeed has
 swallowed them and they are not
lingering in the mouth between the gums and the lip. If you customarily
place pills and capsules in the dog's food, make sure that they have been
consumed. Slick and shiny pills, like gel caps, often slip back out of the
mouths of toothless dogs and end up on the floor (or tray) instead of down
the throat. Once the dog has finished its meal, check the bowl and the area
beneath it to be sure all medications have been consumed.
swallowed them and they are not
lingering in the mouth between the gums and the lip. If you customarily
place pills and capsules in the dog's food, make sure that they have been
consumed. Slick and shiny pills, like gel caps, often slip back out of the
mouths of toothless dogs and end up on the floor (or tray) instead of down
the throat. Once the dog has finished its meal, check the bowl and the area
beneath it to be sure all medications have been consumed.
Toothless dogs are sloppy drinkers. When they lap up water from a bowl, they tend to splash and drip the water onto the floor. So, they should have some absorbent cloth or mat underneath the bowl to avoid leaving a puddle on the floor.
In general, toothless dogs require a lot of patience. Their condition is not their fault, so don't blame the dog for not being able to eat, drink, and take medications like it did before its last dental procedure.
RETURN TO TOP
August 9, 2025:
Health disorders you should assume
your cavalier will develop ...
... and for which you should be prepared in advance.
 Cavalier King Charles spaniels are more likely to
develop a few specific health disorders (listed below) than are average dogs
or other breeds. Veterinary researchers conclude that our breed is
"pre-disposed" to these diseases and some others (listed farther below).
Cavalier King Charles spaniels are more likely to
develop a few specific health disorders (listed below) than are average dogs
or other breeds. Veterinary researchers conclude that our breed is
"pre-disposed" to these diseases and some others (listed farther below).
Cavalier owners should be prepared in advance for these disorders. Preparation includes: (a) knowing how to recognize their signs and symptoms; (b) periodic testing for them; (c) being able to accept that they probably will happen; and (d) having a savings plan and/or insurance to be able to afford the veterinary care and medication bills that will result.
Here is the short list, with the most likely disorders at the top. Each is hyperlinked to a webpage that discusses them in detail.
Mitral valve disease (MVD)
Periodontal disease
Low blood platelets (idiopathic asymptomatic thrombocytopenia)
Dry eye syndrome
Deafness - progressive hereditary hearing loss
Intervertebral disk disease (IVDD)
Chiari-like malformation (CM)
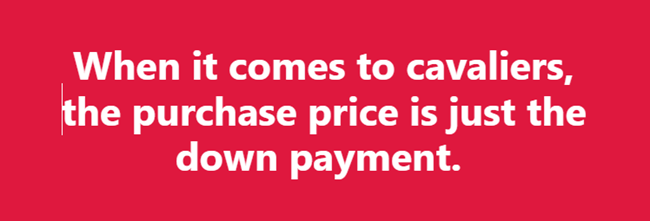
Far too often we read, particularly on Facebook pages, comments by cavalier owners about how shocked they are that their dogs' veterinarians have diagnosed heart murmurs or tooth decay or low blood platelets or back problems in their cavaliers. None of these should come as a surprise. In fact, they should be assumed to happen, and the owners should have plans in place to deal with them, particularly financial plans (for all but low platelets). When it comes to cavaliers, the purchase price is just the down payment.
Here is a complete list of health disorders for which cavaliers are "pre-disposed", according to published veterinary journal articles:
Mitral valve disease (MVD)
Chiari-like malformation (CM)
Syringomyelia (SM)
Low blood platelets (idiopathic asymptomatic thrombocytopenia)
Periodontal disease
Cerebellar infarcts - strokes
Anal sac disorders
Chronic pancreatitis
Brachycephalic airway obstruction syndrome (BAOS)
Curly coat syndrome
Deafness - progressive hereditary hearing loss
Intervertebral disk disease (IVDD)
Diabetes mellitus
Dry eye syndrome
Eosinophilic stomatitis
Facial nerve paralysis
Hip dysplasia (HD)
Idiopathic epilepsy
Episodic falling syndrome
Exocrine pancreatic insufficiency (EPI)
Fly catchers syndrome
Primary secretory otitis media (PSOM) - glue ear
Chronic kidney disesase
Masticatory muscle myositis (MMM)
Hydrocephalus
Muscular dystrophy
Myoclonus
Obesity
Patellar luxation
Pneumocystis pneumonia
Temporomandibular joint dysplasia
Aortic thrombosis
Aortic thromboembolism
RETURN TO TOP
June 6, 2025:
Why Social Media Veterinary Pill
Merchants Should Be Ignored
They Don't Diagnose or Treat.
They Just Want to Sell You Stuff.
Here's Another Example.
 Social Media Veterinary Pill Merchants are veterinarians who have
followings on social media platforms but who do not actually examine dogs as
patients. They should be ignored when they try to sell you something. Why?
Because unless they have examined the dogs as their patients, they have no
valid basis for recommending any treatments which they want you to buy from
them. As board certified veterinary
neurologist Dr. Curtis Dewey wrote recently:
Social Media Veterinary Pill Merchants are veterinarians who have
followings on social media platforms but who do not actually examine dogs as
patients. They should be ignored when they try to sell you something. Why?
Because unless they have examined the dogs as their patients, they have no
valid basis for recommending any treatments which they want you to buy from
them. As board certified veterinary
neurologist Dr. Curtis Dewey wrote recently:
"I won't give specific advice for any dog that I have not physically examined. No veterinarian should."
One of these Social Media Veterinary Mavens advertises a wide variety of dog foods which she has formulated, on her social media platforms to any and all dog owners. And yet, she piously claims in one of her own YouTube videos that:
"I will not formulate a diet for somebody unless I've seen all the veterinary records and I've gone through them and I know what it is that we're dealing with."
Which version of her should we believe? She published a book of 60 dog food recipes, of which all but one of them, she finally confessed, "is not 100% complete and balanced" because their ingredients do not include any essential calcium supplementation. She claims to be the "top holistic veterinarian of the decade", and yet she has not practiced veterinary medicine for over 5 years, and even back then her holistic certifications ("acupuncturist, chiropractitioner, and food therapist") were very limited. A "top holistic veterinarian" should at least also be certified in herbal medicine, homeopathy, and homotoxicology.
 Here
is another example. This same maven is urging her dog owner media fans to buy
from her a product called Legacy Biome FMT (fecal microbiota
transplantation) capsules - 30 of them for $199.99 - to treat dogs "suffering
from chronic allergies".
Here
is another example. This same maven is urging her dog owner media fans to buy
from her a product called Legacy Biome FMT (fecal microbiota
transplantation) capsules - 30 of them for $199.99 - to treat dogs "suffering
from chronic allergies".
In reality, FMT is a process of stool transplanting, whereby fecal material from a donor dog is inserted into the colon of the patient, usually directly into the rectum by a well-trained veterinarian who personally has examined the patient and has diagnosed a disorder for which FMT is an appropriate treatment. Read more about FMT here.
But this Legacy Biome FMT product is to be given orally in a capsule, and as far as this Social Media Vet is concerned, it "may" resolve "chronic itching, scratching, and recurring skin or ear infections". In a video advertisement about the product, she more boldly claims: "These capsules can be beneficial for animals with allergies, inflammatory bowel disease, chronic colitis, clostridium difficile infection, or mood disorders".
Contrary to her representations, this disclaimer is clearly stated on the container of the product itself: "This product is not intended to treat, cure, or prevent disease."
The advertisement on the Social Media Vet's webpage does not give any details about how the fecal material in these capsules was processed or in what form it is. The product's container states only that its ingredients are "Canine fecal material in saline". In fact, the collecting and processing of fecal material for FMT is quite specific and complex.
 The
Companion Animal FMT Consortium in its 2024 "Clinical
Guidelines for Fecal Microbiota Transplantation in Companion Animals"
warns that FMT fecal material should be processed immediately and administered to the patient
immediately or if not, then refrigerated or frozen
in an air-tight container. (See excerpt from report, at left.)
However, the container of the product the Social Media Vet is selling states
only, "Store bottle in a cool dry environment."
The
Companion Animal FMT Consortium in its 2024 "Clinical
Guidelines for Fecal Microbiota Transplantation in Companion Animals"
warns that FMT fecal material should be processed immediately and administered to the patient
immediately or if not, then refrigerated or frozen
in an air-tight container. (See excerpt from report, at left.)
However, the container of the product the Social Media Vet is selling states
only, "Store bottle in a cool dry environment."
What, if anything, does this product have to do with "chronic itching, scratching, and recurring skin or ear infections"? The closest that FMT may come to treating any skin disease, chronic atopic dermatitis (cAD), is in a May 2023 pilot study in which a single dose of freshly obtained fecal material was inserted orally by syringe into 12 dogs, all of which had been diagnosed with chronic atopic dermatitis. The investigators reported:
"In conclusion, the present study revealed that a single oral FMT significantly decreased skin lesions and pruritus scores and changed the gut microbiota in dogs with AD. Since this study was designed as a pilot trial with a short observation period (56 days), further studies are needed to clarify the long-term effect of a single or repeated oral FMT on cAD using a large population of dogs with mild to severe AD and appropriate controls. Nevertheless, this study provides evidence for a crucial role of the gut microbiota in the pathogenesis and a therapeutic target of cAD."
So, the use of FMT to treat "chronic itching, scratching, and recurring skin or ear infections in pets" still is in its fetus stage - 12 dogs in a pilot study about atopic dermatitis barely is even that. And, in that study, the fecal material was fresh and inserted down the throat using a syringe and not a capsule from a bottle that has not even been refrigerated.
And as for the effectiveness of FMT treatments using oral capsules, in a
January 2024 article, in which 54 dogs were studied, fresh fecal
material was orally given by capsule for 25 days. On average, only 18%
of the stool donor's bacterial amplicon sequence variants (ASVs)
engrafted in the FMT recipient. That is fresh feces,
not
 capsules sitting on a cool dry shelf for however long.
Since most capsules are designed to dissolve once they reach the stomach,
and yet the goal of their FMT content is to not disperse until it reaches
the intestines, there necessarily is a loss of effectiveness of the fecal
material that is released before arriving at the intestines.
capsules sitting on a cool dry shelf for however long.
Since most capsules are designed to dissolve once they reach the stomach,
and yet the goal of their FMT content is to not disperse until it reaches
the intestines, there necessarily is a loss of effectiveness of the fecal
material that is released before arriving at the intestines.
RETURN TO TOP
September 21, 2024:
Cavaliers diagnosed with mitral valve disease
need sodium in their diets
 Unlike humans with heart conditions, who are on strict low or no sodium
diets, cavalier King Charles spaniels and other dogs diagnosed with
mitral valve disease (MVD) need
sodium (table salt -- sodium chloride) in their food to offset the effects which both MVD and its
medications, especially diuretics like furosemide (Lasix) and
torsemide, have upon both the heart and the kidneys.
Unlike humans with heart conditions, who are on strict low or no sodium
diets, cavalier King Charles spaniels and other dogs diagnosed with
mitral valve disease (MVD) need
sodium (table salt -- sodium chloride) in their food to offset the effects which both MVD and its
medications, especially diuretics like furosemide (Lasix) and
torsemide, have upon both the heart and the kidneys.
These diuretics drain water from the body, and so they are a main medication for drawing fluids from the lungs of MVD-affected dogs in Stages C and D (congestive heart failure). While that process is good for the heart and lungs, it unfortunately irritates the kidneys to no end. Also, an excessively low sodium level is an electrolyte disorder in dogs, called hyponatremia.
Dogs' kidneys operate most effectively with normal amounts of water and sodium flowing through the blood stream. When the kidneys detect dehydration and/or low levels of sodium in the blood, they release renin, a combination of amino acid residues which form a peptide, into the bloodstream. This renin triggers a cascade of peptides ("angiotensin I and II"), followed by the "angiotensin converting enzyme (ACE)", and then the hormone "aldosterone", which when combined is called the "renin-angiotensin-aldosterone system" (RAAS). This RAAS acts to narrow the blood vessels, increase blood pressure, and conserve sodium. The RAAS also acts upon the brain, causing the dog a sense of increased thirst and an appetite for salt.
Narrowing of blood vessels and high blood pressure are the last two things any MVD-affected dog needs to have happen. Indeed, heart medications such as pimobendan (Vetmedin) and sildenafil (Viagra) are among the MVD drugs designed to widen the blood vessels and lower the blood pressure. Benazepril and enalapril are angiotensin converting enzyme inhibitors (ACE-I), having the main purpose of offsetting the effects of the activated RAAS.
Activation of the RAAS also has been identified as either causing or aggravating chronic kidney disease (CKD), excessively high blood pressure, and proteinuria (excess of proteins in the blood).
In the ACVIM's 2019 Consensus Statement, that panel of cardiologists recommends only "modestly" restricting sodium intake. Specifically, they state:
"Modestly restrict sodium intake, taking into consideration sodium from all dietary sources (including dog food, treats, table food, and foods used to administer medications) and avoid any processed or other salted foods." (Emphasis added.)
In a January 2017 article, Dr. Anton C. Beynen reviewed sodium restricted diets for MVD-affected dogs and concluded:
"There is no evidence that sodium restriction improves clinical signs in canine cardiac disease. Worse still, there are good reasons for contraindication."
Researchers intentionally feed dogs low sodium kibble to cause the kidneys to react badly
Veterinary cardiology researchers feed low sodium dog foods to healthy dogs to intentionally activate their RAAS in order to test the effectiveness of ACE-inhibitor medications. For example, in a July 2022 article, Iowa State Univ. researchers fed nine healthy dogs a low-sodium diet of Hill's Prescription Diet h/d Heart Care dry food for five days. Their levels of sodium reached such low levels that it resulted in steady, dangerous activiation of the dogs' renin-angiotensin-aldosterone system (RAAS). The researchers intentionally wanted to activate the RAAS in order to conduct a study of dosages of the ACE-inhibitor benazepril. In a November 2024 article, researchers testing Cardalis (benazepril/spironolactone) on the renin-angiotensin-aldosterone system in healthy dogs intentionally activated their RAAS system by feeding them the low-sodium diet of Hill's Prescription h/d Heart Care.
MVD-affected cavaliers should avoid low sodium diets, such as Hill's Prescription Diet h/d dry food (with only 17 mg sodium per 100 kcal, 0.12%). To avoid activation of the RAAS, the minimum amount of sodium should never be below the range of from 22.5 to 62 mg per 100 kcal. A solution to the question of what to feed the MVD-affected cavalier, is to choose a high-quality canned or frozen food with fresh, identifiable meats (for example, beef, turkey, chicken -- not "poultry" or "meat") as the main sources of protein and with a moderate amount of sodium (but not a low level), and avoid high sodium dry foods and treats.
The International Small Animal Cardiac Health Council (ISACHC) recommends these minimum amounts of sodium in the diets of MVD-affected dogs:
• Stage B1 or B2: no less than 100 mg/100 kcal.
• Stage C: no less than 80 mg/100 kcal
• Stage D: no less than 50 mg/100 kcal
RETURN TO TOP
July 19, 2024:
How to find a well qualified holistic veterinarian
to treat your
cavalier King Charles spaniel
Holistic vets are vet school graduates dissatisfied
with mediocre
results of conventional care
 We
at CavalierHealth.org have been having our cavalier King Charles spaniels
(among the editors, we've had a total of 13 of them) treated
by holistic veterinarians in addition to conventional (some may say
allopathic) veterinarians. We rely upon the holistic vets for two main
purposes: (1) complementary care, which adds to and
supports the treatments by conventional vets, and does not conflict with
them; and (2) alternative care, which provides treatments
when the conventional vets cannot solve the underlying health problems of
the patient. Combined, these two forms of care are called
integrative veterinary medicine. We usually refer to them as
holistic.
We
at CavalierHealth.org have been having our cavalier King Charles spaniels
(among the editors, we've had a total of 13 of them) treated
by holistic veterinarians in addition to conventional (some may say
allopathic) veterinarians. We rely upon the holistic vets for two main
purposes: (1) complementary care, which adds to and
supports the treatments by conventional vets, and does not conflict with
them; and (2) alternative care, which provides treatments
when the conventional vets cannot solve the underlying health problems of
the patient. Combined, these two forms of care are called
integrative veterinary medicine. We usually refer to them as
holistic.
Holistic vets have more veterinary education and training
The main difference between the two classes of veterinarians is that holistic veterinarians are far more educated and trained than are most conventional vets. Holistic vets hold the same diplomas as do the conventional ones - either a D.V.M. or a V.M.D. - and the same state veterinary licenses. But the holistic vets continue their veterinary education far beyond that degree. Holistic vets are veterinary school graduates who ultimately became dissatisfied with mediocre results from conventional veterinary care. A well trained holistic vet also will have certifications in any of the several treatment modalities listed below.
The level of diagnosis of the patient is a primary distinction between conventional and holistic care. Conventional veterinary diagnostic methods are pretty limited - stethoscope, x-rays, thermometer readings, bloodwork, ultrasound, and a few others. Holistic vets are much more inventive in their ways of diagnosing their patient, in addition to the conventional methods:
• They take pulses at various points on the body. In holistic medicine, there are over two dozen different types of pulses, each one describing a different health condition.
• They examine the tongue, for color, degree of dampness, texture, coating, cracks, shape, tremblingness.
• They look at the dog's coat of hair. Coat condition often indicates degree of nutrition.
• They smell the dog's paws.
• They interview the dog's owner, asking pointed questions about the dog's daily behaviors, life style, sleeping and awake periods, relationships with other dogs and humans, personality traits, and on and on.
• They touch almost every surface of the dog, feeling through the skin to the internal organs, feeling excess heat in muscles and certain organs.
Holistic vets have more treatment options
Conventional veterinary care consists mainly of drugs and surgery. There are several "modalities" of treatment offered in holistic medicine. They include:
• acupuncture
• herbal medicine (traditional Chinese, western, and other herbs and plants)
• homeopathy
• homotoxicology
• nutritional therapy
• chiropractic
• osteopathy
• laser therapy
• stem cell therapy
• flower essences (like Bach's)
• muscle testing
• applied kinesiology
among others. Holistic veterinarians are educated, trained, and certified in any or all of these modalities. Every one of these modalities is extremely complicated to learn and practice. Some holistic vets specialize in only the more complicated modalities, such as muscle testing, applied kinesiology, touch techniques, etc.
Examples of holistic care for mitral valve disease
An example of complementary care provided by holistic vets is for cavaliers diagnosed with mitral valve disease (MVD), particularly those which have reached Stage C, congestive heart failure. The primary conventional medications for treating advanced MVD are pimobendan (Vetmedin) and diuretics, such as furosemide. Holistic vets can complement that treatment by adding supplements to support the heart muscle - keep it strong. They can support the kidneys, which typically are severely damaged by MVD and its medications, with herbs, other supplements, and nutritional therapy, to offset that potential damage.
An example of alternative care for cavaliers with MVD is the experience of one of our dogs. He had MVD and in had enlarged left-side heart chambers. The cardiologist prescribed pimobendan, but the dog could not tolerate that drug. No matter how low the dosage, his reactions made his life unbearable. Our dog's holistic vet provided alternative care in the form of Chinese herbs, homeopathy, homeotoxicology, and acupuncture, and the dog survived for nearly 2 more years without any conventional heart medications except furosemide.
Another example of alternative care was for another of our MVD-affected cavaliers. He was diagnosed by a cardiologist using echocardiography to have enlarged left chambers of his heart. The cardiologist prescribed pimobendan. Instead, our holistic vet recommended d-Ribose, a natural sugar produced by all dogs in their systems to provide energy for the heart. MVD tends to over-tax the dog's production of enough d-Ribose to maintain that energy. We supplemented the dog's meals with d-Ribose for nine months. Then, the same cardiologist, using the same ultrasound echo equipment, re-examined the dog's heart and concluded that his left heart chambers no longer were enlarged.
How to find holistic vets
Now, not every holistic vet is equally educated, trained, and certified.
So, when looking for one for your dogs,
 the search may not be simple. In the
USA and Canada, the American Holistic Veterinary Medical Association (AHVMA)
provides
this search engine for finding their members. When you find an
holistic vet near you, click on his name, and the next page will list the
type of practice modalities he provides. The more modalities the better. As
an example, this page screen capture (below) from that website
lists an holistic vet in New York state with a lengthy list of practice
modalities. As we stated, the more modalities, the better the choices the
vet has to make to treat the patient.
the search may not be simple. In the
USA and Canada, the American Holistic Veterinary Medical Association (AHVMA)
provides
this search engine for finding their members. When you find an
holistic vet near you, click on his name, and the next page will list the
type of practice modalities he provides. The more modalities the better. As
an example, this page screen capture (below) from that website
lists an holistic vet in New York state with a lengthy list of practice
modalities. As we stated, the more modalities, the better the choices the
vet has to make to treat the patient.
In the UK, the British Association of Homeopathic Veterinary Surgeons offers a similar search engine here.
RETURN TO TOP
July 15, 2024:
Be wary of social media veterinarians who recommend products they sell
 THE PROBLEM: A retired veterinarian with a following on social media
sites (Facebook, Instagram, etc.) tells an anecdotal story on YouTube about
how she stopped treating her own syringomyelia-affected cavalier King
Charles spaniel with the syringomyelia (SM) medication
gabapentin,
presumably prescribed by a neurologist, and instead treated her dog only
with an over-the-counter supplement, which she also just happens to be
selling on her website, and at a discount.
THE PROBLEM: A retired veterinarian with a following on social media
sites (Facebook, Instagram, etc.) tells an anecdotal story on YouTube about
how she stopped treating her own syringomyelia-affected cavalier King
Charles spaniel with the syringomyelia (SM) medication
gabapentin,
presumably prescribed by a neurologist, and instead treated her dog only
with an over-the-counter supplement, which she also just happens to be
selling on her website, and at a discount.
She provides no information from any published veterinary journals to support her advice. She just tells a story about how she stopped treating her SM-affected dog with the primary drug prescribed by nearly all veterinary neurologists to their SM patients and switched to the product she is trying to sell on-line. She claims: "For my spaniels, they need this supplement in order to remain off the pain medication, the Gabapentin, with all of the side effects." And, "PEA has worked wonders for our own dogs with syringomyelia, allowing us to discontinue the use of the drug Gabapentin."
The fact is that there is no published clinical research supporting this supplement, palmitoylethanolamide (PEA), to treat syringomyelia. Indeed, veterinary neurologist Dr. Clare Rusbridge spoke recently about the lack of any published studies regarding treating dogs for pain or neuro-degenerative diseases with PEA. She said:
"There are no clinical studies published as scientific articles. And yet, you can find an awful lot of YouTube articles and stuff on the Internet. And it bothers me that is often being pushed by people actually selling the drug. And they are using very unscientific parameters for assessing whether something is effective."
It is important for pet owners to be able to spot clear conflicts of interest, such as social media mavens touting supplements which they are selling. This especially is true when the vendor also is a veterinarian, and the vendor is encouraging using the supplement instead of the medications prescribed by the patients' veterinary specialists.
Not all PEA is alike. Learn important facts HERE about PEA that social media vendors won't tell you.
RETURN TO TOP
July 11, 2024:
Cardiologists' obsession with the Left Atrium-to-Aortic Root Ratio (LA/Ao) clouds their analyses of multiple echocardiograms of cavalier patients
 Picture
it: A cavalier diagnosed with mitral valve disease (MVD) has an
initial echocardiogram in 2023 showing the left atrium (LA) dimension of 26 mm and
the aortic root (Ao) dimension of 15 mm, resulting in a
left atrium-to-aortic
root ratio (LA/Ao)
of 1.73.
Picture
it: A cavalier diagnosed with mitral valve disease (MVD) has an
initial echocardiogram in 2023 showing the left atrium (LA) dimension of 26 mm and
the aortic root (Ao) dimension of 15 mm, resulting in a
left atrium-to-aortic
root ratio (LA/Ao)
of 1.73.
An LA/Ao of that size in most cavaliers would indicate that the left atrium was somewhat enlarged, since normal sized left atriums of cavaliers have a LA/Ao range from 0.47 to 1.36.
So, the cardiologist probably correctly decides that the left atrium is enlarged, due to the MVD. On a scale of "mild/moderate/severe", he categorizes the enlargement as "mild", since he follows the ACVIM's 2019 Consensus Statement's species-wide definition of left atrium enlargement as having a LA/Ao of at least 1.6. He prescribes a starting dosage of pimobendan. He recommends a follow-up echo in 9 to 12 months. The dog's owner also gives her cavalier a few heart supplements with its daily meals.
Nine months later, the same cardiologist, using the same ultrasound equipment, performs a second echocardiogram on the cavalier, finding that the LA/Ao now is 1.83. The cardiologist notes that this second LA/Ao, being higher than the first one nine months previously, indicates that the left artrium has continued to enlarge, and that the degree of enlargement now is "moderate". He increases the dosage of pimobendan.
But what this cardiologist overlooks is that, in the second echo, the left atrium dimension is 22 mm, which is 4 mm smaller than it was in the first echo. And, the aortic root dimension in the second echo is 12 mm, which is 3 mm smaller than it was in the first echo.
So, in reality, this cavalier's left atrium is significantly smaller at the time of the second echo nine months after the first one. It was the variance in the size of the aortic root which resulted in the higher LA/Ao ratio in the second echo scan. The aortic root may vary in size with each beat of the heart, but it is unaffected by MVD. But the cardiologist ignored the 2023 measurement of just the left atrium and focused only upon the differences in the LA/Ao ratios in 2023 and 2024.
Why would he do that? Why ignore a direct comparison between the 2023 dimension of the left atrium and its 2024 dimension? Why, instead, would the cardiologist only compare the 2023 LA/Ao ratio with the 2024 ratio? Inarguably, if the question is whether the left atrium has enlarged since nine months ago, would not comparing the two measurements of that left atrium alone give the answer? Obviously, yes!
 We think we know why the cardiologist ignored the two measurements of the
left atrium alone and instead focused only upon the two LA/Ao ratios. And
the reason is not pretty. We think that far too many cardiologists have been
indoctrinated (brainwashed, perhaps?) into believing that the LA/Ao ratio is
the Gold Standard for determining if the left atrium is enlarged or not.
We think we know why the cardiologist ignored the two measurements of the
left atrium alone and instead focused only upon the two LA/Ao ratios. And
the reason is not pretty. We think that far too many cardiologists have been
indoctrinated (brainwashed, perhaps?) into believing that the LA/Ao ratio is
the Gold Standard for determining if the left atrium is enlarged or not.
Why so? Because the ACVIM's 2019 Consensus Statement says as much. That definition of left atrium enlargement (LA/Ao = 1.6) is not based upon any research evidence whatsoever. It was devised arbitrarily at the start of the EPIC Study and applied to all dogs, regardless of breed. It was and remains totally unscientific and unproven. But nonetheless, it remains. And, far too many cardiologists have bought into it. Mindlessly, if you will.
Aortic root dimensions are not static
 It
is well established that the dimension of the dog's aortic root constantly
changes during each heart beat cycle. So the timing of the measurement
during that cycle must be exactly the same each time a measurement is taken.
And, the starting and ending points of each such measurement likewise must
be exactly the same. Furthermore, the condition of the aortic root has been
known to change as the dog ages; it deteriorates. So, the size of the Ao
when measured when the dog is 5 years old may not be the same as it is when
the same dog is examined at age 9 years. In short, measuring the Ao of the
same dog over time is not bean-bag, and it makes no sense to include the Ao
measurement in calculations of changes in the dimension of the left atrium.
If you want to know whether the LA has changed in size over time, measure
only the LA and leave the Ao out of the equation.
It
is well established that the dimension of the dog's aortic root constantly
changes during each heart beat cycle. So the timing of the measurement
during that cycle must be exactly the same each time a measurement is taken.
And, the starting and ending points of each such measurement likewise must
be exactly the same. Furthermore, the condition of the aortic root has been
known to change as the dog ages; it deteriorates. So, the size of the Ao
when measured when the dog is 5 years old may not be the same as it is when
the same dog is examined at age 9 years. In short, measuring the Ao of the
same dog over time is not bean-bag, and it makes no sense to include the Ao
measurement in calculations of changes in the dimension of the left atrium.
If you want to know whether the LA has changed in size over time, measure
only the LA and leave the Ao out of the equation.
In this 2002 seminal veterinary journal article on the use of the LA/Ao in detecting left atrial enlargement - Left atrial to aortic root indices using two-dimensional and m-mode echocardiography in cavalier king charles spaniels with and without left atrial enlargement - authors Kerstin Hansson, Jens Haggstrom, Clarence Kvart, and Peter Lord warned against blindly relying upon the LA/Ao as the ultimate determinant of LA enlargement. They stated:
"If the Ao dimension becomes increased or decreased, it would alter the resulting ratio and give an under- or over-estimation of LA size. In such instances, an LA/Ao index, whether it is M-mode or two-dimensionally (2-D) derived, needs to be used with caution and only as a guideline." (p. 569)
When board certified veterinary cardiologists, having two echo scan reports in front of them, fail to compare the two measurements of the left atrium alone, and instead look only to the two LA/Ao ratios, they do their patients and the dogs' owners no service. It is the MVD-affected dogs which will continue to suffer because of this bogus definition of enlargement and the intellectually lazy cardiologists who blindly follow it. The dogs suffer because they end up being mis-diagnosed, with either no drug prescribed when necessary or too high a dose when not needed.
RETURN TO TOP
May 20, 2024:
Wild Hair Syndrome Infects
Cavalier Fanciers and DNA Labs
The sham search is on for cavaliers with the NEBL3
gene to
'end' mitral valve disease in the breed!
Two DNA testing labs make false claims that the
gene will prevent cavaliers
from getting MVD
 The idiomatic definition of a "WILD HAIR" is "To
have a fervent, usually sudden, desire to do something surprising or
unexpected." While cavalier King Charles spaniels (CKCS) have not been found to
suffer from a Wild Hair Syndrome (WHS), it appears that a
growing number of cavalier fanciers, including breeders, pet owners, social
media vixens, and even a couple of genetic testing laboratories, have displayed symptoms
of being infected with the WHS neurological disorder.
The idiomatic definition of a "WILD HAIR" is "To
have a fervent, usually sudden, desire to do something surprising or
unexpected." While cavalier King Charles spaniels (CKCS) have not been found to
suffer from a Wild Hair Syndrome (WHS), it appears that a
growing number of cavalier fanciers, including breeders, pet owners, social
media vixens, and even a couple of genetic testing laboratories, have displayed symptoms
of being infected with the WHS neurological disorder.
The primary symptom of WHS in these victims is a fervent, sudden desire to have all cavaliers' DNA tested for a specific gene, the wild-type variant of the nebulette (NEBL) allele, known as NEBL3. The underlying belief appears to be that CKCSs with that NEBL3 variant are impervious to mitral valve disease (MVD or MMVD), and therefore these dogs should be identified and promptly mated with each other to produce bloodlines which no longer suffer from this leading killer of cavaliers.
The motivation may be commendable, but the science behind it is virtually
nonexistent. It all stems from a veterinary journal article published in
December 2022 in which Australian researchers found 6 Australian
cavaliers with a wild-type version of the NEBL3 gene in their DNA.
The article's authors suggested that "Selection for the wild-type allele at
NEBL3 could decrease MMVD severity in the breed." The operative
word there is "could". After all, they are talking about research involving
only 6 dogs from a single (and very insular)
 country, and suggesting that
finding and breeding more cavaliers world-wide like those "could" reduce MVD
in the breed.
country, and suggesting that
finding and breeding more cavaliers world-wide like those "could" reduce MVD
in the breed.
One cavalier fancier, Beverley Cuddy, has inaccurately written about that study on page 6 of the June 2024 issue of Dogs Today magazine (right) that:
"Australian scientists have found a very rare and promising gene in six Cavaliers - a gene that might prove to be protective against mitral valve disease (MVD), a ghastly heart problem that afflicts half of all Cavaliers by the age of five." (Emphasis added.)
Considering that 5 of those 6 cavaliers (83.3%) in that Australian study already had been diagnosed with MVD, it clearly is a gross misreading to claim from that study that the gene "might prove to be protective against mitral valve disease (MVD)." The Wild Hair Syndrome is wildly evident in Ms. Cuddy's article.
Why only NEBL3 now?
And so, we must ask, Why the focus of so many non-geneticists upon NEBL3? Well, it appears that at least two of the canine gene testing laboratories, GenSol and Laboklin, have introduced a genetic test for that gene in cavaliers, based upon blood or saliva samples submitted to them. Presumably the GenSol and Laboklin folks decided to take it upon themselves to follow up on that December 2022 study of the wild-type NEBL3 allele. But apparently neither of them has ever actually read that study.
Laboklin goes well beyond any published research by falsely claiming that "It is very unlikely that the dog will develop Myxomatous mitral valve disease (MMVD)." GenSol goes even further by claiming "These dogs have two copies of the normal gene and will neither develop Myxomatous Mitral Valve Disease nor pass this mutation to their offspring."
There is nothing in the Australian study's article that supports that statement. In fact, the article flatly contradicts it. Five of the 6 cavaliers with the wild-type NEBL3 allele had mitral valve disease, and 1 of those 5 had enlargement of its left atrium and ventricle (ACVIM Stage B2). See Table 5 from the December 2022 article, here:
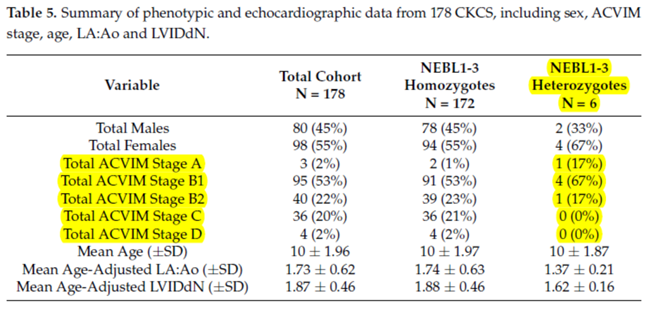
MVD in cavaliers has been indisputably polygenic
Thus far, no scientific evidence supports finding NEBL3 cavaliers and breeding them with each other will save the breed from MVD. So, why just NEBL3? This 2022 study is not the first and only such investigation into genes unique to cavaliers and tied to the breed's hereditary mitral valve disease. Other studies have identified other promising MVD-related genetic regions, and none of them have included NEBL.
Indeed, in one of the earliest studies into MVD in cavaliers, in January 1996, Swedish researchers Lennart Swenson, Jens Haggstrom, and Clarence Kvart studied 144 CKCSs and reported that MVD in cavaliers "is a polygenic threshold trait and that sex of the offspring influences threshold levels." That finding has never been disputed in any subsequent research.
Genetic research studies of cavaliers have been published since as early as 2011. In a September 2011 article by an international team of 15 renowned cardiologists and geneticists, they conducted a genome-wide association study (GWAS) to identify loci associated with MVD, using 241 cavaliers from 5 countries - Denmark, Sweden, Germany, England, and France. They identified two genetic regions - the CFA (cyclopropane fatty acid) 13 and 14 loci - as having "a strong association of MMVD". They noted that CFA 13 consists of 20 separate genes, and CFA 14 have 11 such genes, and that "some of these genes are good candidate genes for the development of MMVD".
In a November 2011 article, UK cardiologists and geneticists conducted a genome-wide genetic approach with 36 cavaliers, all with varying degrees of MVD. They reported finding no genetic regions of loci associated with MVD, and they concluded that:
"This analysis suggests that familial occurrence of mitral valve murmur in the CKCS breed is not due to a single major gene effect, indicating that breeding strategies to eliminate the disease cannot be based on genotype information at this time."
In a December 2017 article, a team of 10 American cardiologists and geneticists examined the DNA in 10 cavaliers and 10 dachshunds diagnosed with MVD, searching for varients of genes known to be analogous to genetic mutations associated with MVD in humans. They reported finding no such variants in any of the canine genes evaluated, and that they could not identify any genetic cause responsible for human MVD in the dogs studied. They concluded that MVD in the CKCS and dachshund may not share an identical genetic cause with the human MVD.
In an April 2020 article, a Royal Veterinary College team led by Dr. Brendan Corcoran examined the mitral valves of 30 euthanized MVD-affected dogs, including 8 cavaliers (27%) to classify the valves according to MVD severity (Grade 0 - normal -- to Grade 4 - severely affected) and to identify all differentially expressed genes (DEGs) in all four such grades. By transcriptomic profiling they identified a total of 1,002 DEGs associated with a large number of gene families. Depending upon the grade of MVD, they found significant changes in gene expression intensity in especially ACTA2, HTR2B, MMP12, and CDKN2A. The TGFß1, TNF, IFGN genes were identified as the top up-stream regulators in the diseased valve samples. Of those, they found that TGFß1 appears to have the strongest associations with the disease. Dr. Corcoran's research in this area is on-going. Note that NEBL was not included.
In a January 2023 article, Denmark investigators reported their examinations into the genetic makeup of 34 elderly (mostly aged 10 years) Swedish cavaliers, 19 of which had no mitral valve disease (MVD) or were in Stage B1 or B2, and 15 dogs in Stage C with severe MVD. Their aim was to identify genes which expressed themselves differently and which may explain the difference in the progression of MVD in the two groups of cavaliers. They identified 56 genes which were differentially expressed (DE) between the two groups. None of those 56 genes were in the NEBL loci.
Of those 56 genes, several were either "up-regulated" or "down-regulated" in the group with no MVD or in its earlier stages, suggesting that these changes in those genes were an appropriate reaction to whatever was the cause of their MVD, and that those same genes in the dogs in the severe MVD group did not respond accordingly. Of those genes, up-regulation of particularly ALDH1A2 and RDH10 may be a compensatory reaction to MVD rather than a cause of disease. If so, then this up-regulation resulted in the disease not progressing into severe MVD with congestive heart failure (CHF). They also found three other genes, MYH1, LOC102724058, and CNTN3, with the greatest difference in expression between the two groups of cavaliers, and which were not part of an orchestrated response to disease but instead may be causative agents of MVD. They concluded:
"Based on these observations, we suggest that the primary cause of MMVD in CKCS may be found in a gene coding for one of the heart muscle proteins. However, the conclusion based on the present results is that an appropriate upregulation of MYH1 and downregulation of CNTN3, as a response to a so far unknown causative factor, can protect a dog with MMVD from developing CHF. An alternative conclusion is that an inappropriate downregulation and upregulation of MYH1 and CNTN3, respectively, in CKCS with MMVD may lead to development of CHF."
In a December 2024 article, genetic researchers examined the genetic makeup of 24 13+ year old cavaliers, to determine which genes may be associated with longevity in the breed. All 24 13+ year old cavaliers and 17 younger "reference" CKCSs were owned by CKCS club members in the Czech Republic. Nine candidate genes were identified: B3GALNT1, NLRP1 like, PARP14 IQCJ-SCHIP1, COL9A1, COL19A1, SDHAF4, B3GAT2, and DIRC2. Note that NEBL3 is not among them.
These are just a sampling of genome-wide research into cavaliers and other breeds affected with MVD. None of that other research has suggested that the NEBL regions would be candidates, much less zeroing in on NEBL3.
The results remain to be seen. But the laser-like focus upon only one
gene to solve the MVD question, when so
 many others have been identified in
so many other studies of cavaliers, seems to us to be terribly misguided and
wasteful of financial resources.
many others have been identified in
so many other studies of cavaliers, seems to us to be terribly misguided and
wasteful of financial resources.
Nevertheless, a bandwagon effect has been started, which many cavalier fanciers scrambled upon in typical Wild Hair Syndrome fashion.
RETURN TO TOP
February 17, 2024:
Nutrition needs of dogs
with mitral valve disease
 General
nutrition for dogs diagnosed with mitral valve disease (MVD) is very important as
the MVD progresses
through its stages. As MVD worsens, the dog's loss of skeletal muscle
mass (cardiac cachexia) is a major threat to its survival. See our section on exercise
intolerance and loss of skeletal mass for details about cardiac
cachexia.
General
nutrition for dogs diagnosed with mitral valve disease (MVD) is very important as
the MVD progresses
through its stages. As MVD worsens, the dog's loss of skeletal muscle
mass (cardiac cachexia) is a major threat to its survival. See our section on exercise
intolerance and loss of skeletal mass for details about cardiac
cachexia.
MVD-affected dogs need complete proteins from animal sources (muscle meats from mammals, poultry, fish, eggs), which provide all of the essential amino acids. Plant-based foods which may provide some proteins, are not sufficiently healthful alone for dogs diagnosed with MVD.
All meats and vegetables should be as fresh and un-processed as possible. The MVD-affected dog's food should not be overly processed, such as dry dog foods (kibble) are, because each step in that processing removes natural nutrients esssential for a complete, well balanced diet. Meats should be changed periodically, such as each month, to assure that the dog is ingesting nutrients from a variety of sources.
Grains may be included or not, depending upon the other health issues of the dog, but grains never should be relied upon as the main sources of proteins for MVD-affected dogs.
An example of a truly unhealthful food which MVD-affected cavaliers should avoid is Royal Canin's "Cavalier King Charles Adult Dry Dog Food". According to Royal Canin, this food's ingredients are:
"Brewers rice, wheat gluten, chicken by-product meal*, corn, chicken fat, wheat, natural flavors, driedplain beet pulp, fish oil, pea fiber, dried tomato pomace, vegetable oil, rice hulls, calcium carbonate, sodium silico aluminate, L-lysine, potassium chloride, vitamins [DL-alpha tocopherol acetate (source of vitamin E), niacin supplement, L-ascorbyl-2-polyphosphate (source of vitamin C), D-calcium pantothenate, biotin, pyridoxine hydrochloride (vitamin B6), riboflavin supplement, thiamine mononitrate (vitamin B1), vitamin A acetate, folic acid, vitamin B12 supplement, vitamin D3 supplement], fructooligosaccharides, sodium tripolyphosphate, DL-methionine, L-arginine, taurine, potassium citrate, hydrolyzed yeast, choline chloride, salt, marigold extract (Tagetes erecta L.), L-tyrosine, trace minerals [zinc oxide, ferrous sulfate, zinc proteinate, manganous oxide, manganese proteinate, copper sulfate, calcium iodate, sodium selenite, copper proteinate], glucosamine hydrochloride, L-carnitine, magnesium oxide, green tea extract, chondroitin sulfate, rosemary extract, preserved with mixed tocopherols and citric acid." (Emphasis added.)
Notice that there is no meat included in this list, at all. The sources of protein are grains -- rice, wheat, corn. "Chicken by-product meal" by definition* does not include meat. So, this food is not providing the MVD-affected cavalier King Charles spaniel (or any MVD-affected breed, for that matter) with all of the essential proteins from natural sources, which are necessary for the dog to maintain as healthy a heart as possible.
* The Association of American Food Control Officials (AAFCO) defines "meat by-products" as: "the non-rendered, clean parts, other than meat, derived from slaughtered mammals." (Emphasis added.) The AAFCO defines "poultry by-products" as: "non-rendered clean parts of carcasses of slaughtered poultry, such as heads, feet and viscera, free from fecal content and foreign matter except in such trace amounts as might occur unavoidably in good factory practice. If the product bears a name descriptive of its kind, it must correspond thereto."
Read the ingredients lists on the containers
Before you buy any dog food, read the list of ingredients** on the container. Or, better yet, find the ingredients list via the Internet before going to the store. Chewy.com is a good on-line source for finding ingredients lists of the many brands of dog food they offer for sale. Look for the "Nutritional Information" link on each food's webpage.
** Some veterinary nutritionists will advise to "Stop reading your pet food ingredient list!". Ignore this advice. It is coming from veterinarians who are heavily funded by dry dog food companies who want you to feed your dogs their grains instead of meats for proteins. Far too many "board certified veterinary nutritionists" are so financially conflicted in this way, that their advice usually is very suspiciously motivated.
The ingredients are listed in descending order by weight on those lists. So, the first
ingredient is the heaviest
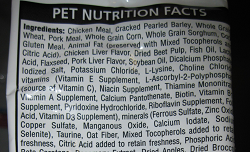 and the last ingredient is the lightest. If
the first ingredient is an identifiable animal's meat, such as "beef" or
"turkey", that is a positive piece of information about that food. But,
for example, if the second through fourth ingredients are grains, such
as corn, wheat, or rice, then very likely the combination of weights of
those grains far outweigh the quantity of meat listed first. So that
means that, even though a meat is listed first, most of the protein is
coming from the combination of grains listed after the meat.
and the last ingredient is the lightest. If
the first ingredient is an identifiable animal's meat, such as "beef" or
"turkey", that is a positive piece of information about that food. But,
for example, if the second through fourth ingredients are grains, such
as corn, wheat, or rice, then very likely the combination of weights of
those grains far outweigh the quantity of meat listed first. So that
means that, even though a meat is listed first, most of the protein is
coming from the combination of grains listed after the meat.
And, of course, if the animal ingredient is listed as "by-product", that means it is not meat at all. Also, if the meat ingredient is described as "meal", as in "chicken meal", that means the meat has been excessively processed and very likely has lost its nutrient value.
Generally speaking, the more items in an ingredients list means the more processed the food is and the more synthetic additives there are in that food. That is especially the case if the items low on the list are oddly named (as many are in the Royal Canin list quoted above) and not identifiable as vegetables or fruits. Artificial forms of vitamins and other nutrients are added to foods if the natural sources of those nutrients were destroyed in the processing (or not existing to begin with).
For example, if the amino acid taurine is listed separately way down on the list (as it is in the meatless Royal Canin list quoted above), that likely means that the meat (if any) was so overly processed that the natural taurine in that meat has been destroyed, so the maker had to add artificial taurine to the ingredients to make up for the destruction of the natural taurine in the meat. Dogs produce taurine in the liver of their own bodies. As long as MVD-affected dogs are fed sufficient fresh meats in their diets, they should not need chemically-produced supplemental taurine unless their blood tests show a taurine deficiency. See this link for more information about taurine supplementation.
MVD-affected dogs need sodium
 Unlike humans with heart conditions, who are on strict low or no sodium
diets, MVD-affected dogs need
sodium (table salt) to offset the effects which both MVD and its
medications, especially diuretics like furosemide (Lasix) and
torsemide, have upon both the heart and the kidneys. These diuretics
drain water from the body, and so they are a main medication for drawing
fluids from the lungs of MVD-affected dogs in Stages C and D (congestive
heart failure). While that process is good for the heart and lungs, it
unfortunately irritates the kidneys to no end. Also, an excessively low
sodium level is an electrolyte disorder in dogs, called hyponatremia.
Unlike humans with heart conditions, who are on strict low or no sodium
diets, MVD-affected dogs need
sodium (table salt) to offset the effects which both MVD and its
medications, especially diuretics like furosemide (Lasix) and
torsemide, have upon both the heart and the kidneys. These diuretics
drain water from the body, and so they are a main medication for drawing
fluids from the lungs of MVD-affected dogs in Stages C and D (congestive
heart failure). While that process is good for the heart and lungs, it
unfortunately irritates the kidneys to no end. Also, an excessively low
sodium level is an electrolyte disorder in dogs, called hyponatremia.
Dogs' kidneys operate most effectively with normal amounts of water and sodium flowing through the blood stream. When the kidneys detect dehydration and/or low levels of sodium in the blood, they release renin, a combination of amino acid residues which form a peptide, into the bloodstream. This renin triggers a cascade of peptides ("angiotensin I and II"), followed by the "angiotensin converting enzyme (ACE)", and then the hormone "aldosterone", which when combined is called the "renin-angiotensin-aldosterone system" (RAAS). This RAAS acts to narrow the blood vessels, increase blood pressure, and conserve sodium. The RAAS also acts upon the brain, causing the dog a sense of increased thirst and an appetite for salt.
Narrowing of blood vessels and high blood pressure are the last two things any MVD-affected dog needs to have happen. Indeed, heart medications such as pimobendan (Vetmedin) and sildenafil (Viagra) are among the MVD drugs designed to widen the blood vessels and lower the blood pressure. Benazepril and enalapril are angiotensin converting enzyme inhibitors (ACE-I), having the main purpose of offsetting the effects of the activated RAAS.
Activation of the RAAS also has been identified as either causing or aggravating chronic kidney disease (CKD), excessively high blood pressure, and proteinuria (excess of proteins in the blood).
In the ACVIM's 2019 Consensus Statement, that panel of cardiologists recommends only "modestly" restricting sodium intake. Specifically, they state:
"Modestly restrict sodium intake, taking into consideration sodium from all dietary sources (including dog food, treats, table food, and foods used to administer medications) and avoid any processed or other salted foods." (Emphasis added.)
In a January 2017 article, Dr. Anton C. Beynen reviewed sodium restricted diets for MVD-affected dogs and concluded:
"There is no evidence that sodium restriction improves clinical signs in canine cardiac disease. Worse still, there are good reasons for contraindication."
Veterinary cardiology researchers feed low sodium dog foods to healthy dogs to intentionally activate their RAAS in order to test the effectiveness of ACE-inhibitor medications. For example, in a July 2022 article, Iowa State Univ. researchers fed nine healthy dogs a low-sodium diet of Hill's Prescription Diet h/d dry food for five days. Their levels of sodium reached such low levels that it resulted in steady activiation of the dogs' renin-angiotensin-aldosterone system (RAAS). The researchers intentionally wanted to activate the RAAS in order to conduct a study of dosages of the ACE-inhibitor benazepril. In a November 2024 article, researchers testing Cardalis (benazepril and spironolactone) on the RAAS in healthy dogs intentionally activated their RAAS by feeding them the low-sodium diet of Hill's Prescription h/d Heart Care.
MVD-affected cavaliers should avoid low sodium diets, such as Hill's Prescription Diet h/d dry food (with only 17 mg sodium per 100 kcal, 0.12%). To avoid activation of the RAAS, the minimum amount of sodium should never be below the range of from 22.5 to 62 mg per 100 kcal. A solution to the question of what to feed the MVD-affected cavalier, is to choose a high-quality canned or frozen food with fresh, identifiable meats (for example, beef, turkey, chicken -- not "poultry" or "meat") as the main sources of protein and with a moderate amount of sodium (but not a low level), and avoid high sodium dry foods and treats.
The International Small Animal Cardiac Health Council (ISACHC) recommends these minimum amounts of sodium in the diets of MVD-affected dogs:
• Stage B1 or B2: no less than 100 mg/100 kcal.
• Stage C: no less than 80 mg/100 kcal
• Stage D: no less than 50 mg/100 kcal
Cardiac "prescription diets" to avoid
Beware of dog foods touted by veterinarians as "prescription diets" which are claimed to be designed to treat dogs with heart problems. Some vets, indeed many of them, fall for any dog food with the word "cardiac" on its label and which they "prescribe" for MVD-affected dogs. Here are two of the absolute worst such foods:
• Hill's Heart Care h/d: This dry food has an excessively low quantity of sodium, which has been known to activate the dog's kidneys' RAAS. In a July 2022 article, researchers fed healthy dogs this food for five days. Their levels of sodium reached such low levels that it caused the dogs' RAAS to steadily activate. In a November 2024 article, researchers testing Cardalis (benazepril and spironolactone) on the renin-angiotensin-aldosterone system in healthy dogs intentionally activated their RAAS by feeding them the low-sodium diet of Hill's Prescription h/d Heart Care.
• Purina Pro Plan CC Cardiocare: This dry food has been found in a peer-reviewed study to have no significant effects upon the left atrium and left ventricle in 101 MVD-affected dogs (29 CKCSs). It also contains medium chain triglycerides (MCTs), which have been found to be dangerous to a high percentage of cavaliers. See our webpage on the hazards of MCTs to far too many cavaliers.
See more about these two hazardous-to-cavaliers dog foods at this link.
Heart supplements for the dog's daily meals
MVD-affected dogs will need their diets fortified with heart supplements. Some supplements will benefit the dog in general. Others are mostly beneficial once MVD has been diagnosed. Others should be held back, or not increased in dosages, until the stage of MVD is more advanced than just having a murmur. Most heart supplements are compatible with heart medicines, and in some instances, the supplements will complement the drugs to the extent that lower doses of the drugs may be possible.
From the beginning, even prior to a murmur being detected, a good multi-vitamin, Omega-3s, and a low dose of CoQ10 should be beneficial. Others to add after MVD is diagnosed and progresses are d-Ribose, hawthorn, magnesium, and a higher dose of CoQ10. Read all about them and others at this link.
RETURN TO TOP
January 29, 2024:
Is the cavalier breed about to run out of healthy genes?
 A veterinary study* published this month
recommends that cavalier breeders should not breed any cavalier younger than
3 years and even then, exclude from breeding all breeding stock with a
syringomyelia syrinx as tiny as a half millimeter wide. In that study of 555
dogs, they found that 46% of them had a syrinx at least that large.
A veterinary study* published this month
recommends that cavalier breeders should not breed any cavalier younger than
3 years and even then, exclude from breeding all breeding stock with a
syringomyelia syrinx as tiny as a half millimeter wide. In that study of 555
dogs, they found that 46% of them had a syrinx at least that large.
Add this breeding prohibition to this ever growing list of these hereditary disabilities for which affected cavaliers should not be bred:
• Mitral valve disease
• Eye disorders
• Hereditary hearing deficiencies
• Luxating patellas
• Hip dysplasia
• Brachycephalic airway obstruction syndrome
• Episodic falling syndrome
• Flycatcher's syndrome
• Renal dysplasia
• Medium chain triglyceride mutation (MCADD)
• Seizures of any of several causes
• Curly coat syndrome
• Chondrodystrophy
• Degenerative myelopathy
• Muscular dystrophy
• Xanthinuria
Also, add to this list, the stringent requirements of every country's national CKCS breed club that the offspring of only purebred cavaliers be registered, and that in conformation competitions, they adhere to the clubs' breed standards of:
• general appearance
• personality
• structure
• skull shape
• eye size
• nose shape
• muzzle length
• teeth positions
• ears set
• neck length
• shape of shoulders
• position, shape, and musculature of legs
• tail position and motion
• coat length and curliness
• coat colors
• feathering
• overall size
• weight.
 And, finally, consider that probably 90% of each generation of cavaliers
are placed as pets and not bred at all.
And, finally, consider that probably 90% of each generation of cavaliers
are placed as pets and not bred at all.
* Limpens, C., et al. The effect of MRI-based screening and selection on the prevalence of syringomyelia in the Dutch and Danish Cavalier King Charles Spaniels. Front. Vet. Sci. January 2024; doi: 10.3389/fvets.2024.1326621.
RETURN TO TOP
January 25, 2024:
Eggs shells are a poor source of calcium in dogs' diets
Use calcium citrate, instead
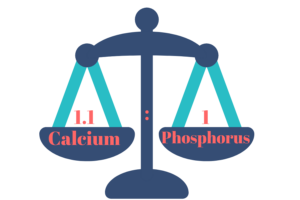 Calcium
is an important ingredient for many of the dog's bodily systems and
functions, including bone and tooth formation, blood clotting, enzyme
activation, muscle contraction, skin and hair growth, and nerve impulse
transmission. Most all sources of proteins, especially meats, contain
much higher levels of phosphorus and lower levels of calcium.
Calcium
is an important ingredient for many of the dog's bodily systems and
functions, including bone and tooth formation, blood clotting, enzyme
activation, muscle contraction, skin and hair growth, and nerve impulse
transmission. Most all sources of proteins, especially meats, contain
much higher levels of phosphorus and lower levels of calcium.
Dogs are naturally equipped internally to maintain a normal ratio of calcium to phosphorus -- usually a ratio of 1.1 or 1.2 calcium to 1.0 phosphorus, by weight. As phosphorus levels in the dog's blood rise due to an insufficiency of calcium, the body draws calcium from the bones to keep that ratio in balance.
Dietary calcium insufficiency is a common and dangerous consequence of not adding appropriate quantities of digestible calcium to each meal. See this tragic March 2021 case study: A pair of University of Liverpool veterinary clinicians report treating a 5-month old Bernese mountain dog for severe bone pain and inability to stand. The puppy had been fed only raw chicken and beef. They diagnosed nutritional secondary hyperparathyroidism due to dietary calcium insufficiency. After five days of in-hospital treatment, the puppy was able to walk stiffly. A re-evaluation appointment was scheduled for four weeks later, but the owner failed to fed the dog a prescribed diet, and the patient was euthanized three weeks later.
When preparing dog foods from scratch, it is essential that this ratio of calcium-to-phosphorus be calculated accurately and that sufficient calcium powder be added to the recipe to balance the excess phosphorus in the protein sources. To do this properly, if the recipe does not tell you how much calcium to add, you first must determine how much excess phosphorus is in the protein source in the recipe. Then calculate, using the ratio, how much calcium to add. Examples of excess phosphorus levels in meats:
• Beef: 859 mg/lb net phosphorus over calcium
• Non-beef (turkey, chicken, beef organs): 1100 mg/lb net phosphorus over calcium.
Beware of egg shells as the calcium source
Beware of any recipes or commercial brands of dog food which use egg
shells as the added source of calcium. Egg shells are composed of
calcium carbonate (CaCO3), which is
 an antacid and is used
medically to treat
heartburn. Calcium carbonate reduces the amount of acid
in the stomach by stopping the enzyme pepsin that creates acid to digest
food. The active ingredient in the antacid TUMS® is calcium carbonate.
an antacid and is used
medically to treat
heartburn. Calcium carbonate reduces the amount of acid
in the stomach by stopping the enzyme pepsin that creates acid to digest
food. The active ingredient in the antacid TUMS® is calcium carbonate.
When egg shells are the source of calcium in a dog's diet, the
undesirable side effect is that dogs' digestive system acids are
neutralized, and much of the consumed foods, particularly meats, do not
 get
fully digested. So, no matter how finely ground the egg shells may be (and
they should be as fine as a talc-like powder), they are more likely to
interfere with the dog's digestion than to serve to balance excess phosphorus in the meats in the recipes.
get
fully digested. So, no matter how finely ground the egg shells may be (and
they should be as fine as a talc-like powder), they are more likely to
interfere with the dog's digestion than to serve to balance excess phosphorus in the meats in the recipes.
Also, most commercial brands of eggs are coated with a non-organic mineral oil, as a preservative, which is not digestible at all.
Calcium citrate is an excellent source of calcium to use as a supplement, such as this NOW product. Calcium citrate will not neutralize the dog's stomach acid and will not interfere with the digestion of the meats and other foods the dog consumes, unlike the calcium carbonate in egg shells. Calcium absorption from calcium citrate also has been found in published studies to to be significantly greater than that from calcium carbonate.
Egg shells attract bacteria and must be thoroughly cleaned if consumed
The outer shells of commercially processed eggs are required to be washed
soon after being collected. This washing removes the protective cuticle (the
bloom) which covers the egg as it is being laid by the hen. The washing also
is expected to remove most or all bacteria from the surface of the shell,
which particularly would
 include
strains of Salmonella and Escherichia coli (E. coli). Eggs obtained directly
from farms rarely are washed and therefore the outer shells are likely
carriers of such dangerous bacteria. All egg shells remain susceptible to
attracting such bacteria, and therefore any egg shells which are going to be
crushed and added to dogs' food must be thoroughly cleaned.
include
strains of Salmonella and Escherichia coli (E. coli). Eggs obtained directly
from farms rarely are washed and therefore the outer shells are likely
carriers of such dangerous bacteria. All egg shells remain susceptible to
attracting such bacteria, and therefore any egg shells which are going to be
crushed and added to dogs' food must be thoroughly cleaned.
Then the shells must be crushed to a fine powder, to avoid any sharp edged pieces damaging the dogs internally.
RETURN TO TOP
November 16, 2023:
Not all PEA (palmitoylethanolamide) is alike
Ordinary PEA is not absorbed well in the gut
 Palmitoylethanolamide (PEA) is a
N-acylethanolamine molecule in a family of long-chain fatty acid
amides
called ALIAmides. PEA has been found in rat and mice studies to limit
hyperactvity in immune cells and thereby control inflammatory responses
and resulting tissue damage.
Palmitoylethanolamide (PEA) is a
N-acylethanolamine molecule in a family of long-chain fatty acid
amides
called ALIAmides. PEA has been found in rat and mice studies to limit
hyperactvity in immune cells and thereby control inflammatory responses
and resulting tissue damage.
PEA is produced naturally by the animal's body as needed in response to certain types of injuries. PEA is a product of normal fatty acid synthesis from palmitic acid. It is found in many common foods, particularly palm oil, soy beans, egg yolks, and peanuts. The commercial versions are most commonly manufactured from palm oil.
Thus far, no objective, un-conflicted clinical studies of the effect of PEA in treating dogs have been published. PEA vendors' claims that PEA may relieve symptoms due to arthritis, urinary tract disorders, neuropathic pain (CM/SM), cancer, or lung conditions are not based upon any scientific studies of dogs. The only such canine study thus far has involved atopic dermatitis, sponsored by PEA patent holders.
Not all PEA is alike
There are three types of PEA:
• Basic PEA, called "naive PEA" or ordinary PEA, is insoluble in water, and therefore the oral intake of it (rather than being injected directly into the abdomen) has very poor bioavailability, meaning that it does not get absorbed well in the dog's gut.
• Micronized PEA (m-PEA) is a patented technique that reduces the diameter of PEA particles, making them absorbable in the intestine, which has been found to be more effective than ordinary naive PEA in activating PEA levels in blood plasma in dogs. See this August 2014 article.
• Ultra-micronized PEA (um-PEA), also patented, reduces the PEA particle size further, to enable it to cross the blood-brain barrier, likewise has been found to be much more effective than naive PEA and was used in the dermatitis study. See also this August 2014 article.
 If a PEA product is not advertised as being micronized or
ultra-micronized, then
Dr. Clare Rusbridge advises that
"You
probably are wasting your money."
A variety of brands of
micronized and ultra-micronized PEA are offered on-line.
If a PEA product is not advertised as being micronized or
ultra-micronized, then
Dr. Clare Rusbridge advises that
"You
probably are wasting your money."
A variety of brands of
micronized and ultra-micronized PEA are offered on-line.
Recent research has produced evidence that ALIAmides can relieve dogs with hypersensitive skin disorders. In an August 2015 article, Italian researchers conducted an 8-week study of the effectiveness of oral ultra-micronized palmitoylethanolamide (um-PEA) in 160 dogs with moderate atopic dermatitis. Each dog received a daily dose of um-PEA at the rate of 10 mg/kg for 56 days. They report finding that um-PEA appeared to be effective and safe in reducing pruritus and skin lesions, and in improving the quality of life in dogs with moderate atopic dermatitis and moderate pruritus.
As for dosages, the studies using micronized PEA, the range was from 10 to 15 mg/kg/day, and the range for ultra-micronized was 24 mg/kg (for osteoarthritis).
Also, as for palm oil, the palm oil cultivation industry has been destroying rainforests in Sumatra and Borneo in Indonesia and Malaysia, the only habitats of orangutans. If you are going to obtain PEA, we suggest that you do so only from vendors whose PEA has been manufactured with palm oil from sustainable sources and not the deforestation of rainforests. This link connects to a "PalmOil Scan Mobile App" which will enable you to determine if the PEA vendors you select obtain their palm oil from sustainable sources.
RETURN TO TOP
October 17, 2023:
MVD-affected cavaliers need
sodium in their daily meals
Too little salt activates the kidneys' RAAS
 General nutrition is very important as
mitral valve disease (MVD) progresses through its stages. Dietary treatment varies, depending upon the stage
(B1, B2, C, D) of the MVD. For dogs with any heart enlargement, the panel of cardiologists
authoring the
ACVIM's 2019 Consensus
Statement on diagnosing and treating MVD
recommends only a "mild dietary sodium restriction and provision of a highly
palatable diet with adequate protein and calories for maintaining
optimal body condition." (Emphasis added.)
General nutrition is very important as
mitral valve disease (MVD) progresses through its stages. Dietary treatment varies, depending upon the stage
(B1, B2, C, D) of the MVD. For dogs with any heart enlargement, the panel of cardiologists
authoring the
ACVIM's 2019 Consensus
Statement on diagnosing and treating MVD
recommends only a "mild dietary sodium restriction and provision of a highly
palatable diet with adequate protein and calories for maintaining
optimal body condition." (Emphasis added.)
Unlike humans with heart conditions, who are on strict low or no sodium diets, MVD-affected dogs need sodium (table salt) to offset the effects which both MVD and its medications, especially loop diuretics, like furosemide (Lasix) and torsemide, have upon both the heart and the kidneys. These diuretics drain water from the body, and so they are a main medication for drawing fluids from the lungs of MVD-affected dogs in Stages C and D (congestive heart failure). While that process is good for the heart and lungs, it unfortunately irritates the kidneys to no end. Also, an excessively low sodium level is an electrolyte disorder called hyponatremia.
The renin-angiotensin-aldosterone system (RAAS)
Dogs' kidneys operate most effectively with normal amounts of water and sodium flowing through the blood stream. When the kidneys detect dehydration and/or low levels of sodium in the blood, they release renin, a combination of amino acid residues which form a peptide, into the bloodstream. This renin triggers a cascade of peptides ("angiotensin I and II"), followed by the "angiotensin converting enzyme (ACE)", and then the hormone "aldosterone", which when combined is called the "renin-angiotensin-aldosterone system" (RAAS). This RAAS acts to narrow the blood vessels, increase blood pressure, and conserve sodium. The RAAS also acts upon the brain, causing the dog a sense of increased thirst and an appetite for salt.
Narrowing of blood vessels and high blood pressure are the last two things any MVD-affected dog needs to have happen. Indeed, heart medications such as pimobendan (Vetmedin) and sildenafil (Viagra) are among the MVD drugs designed to widen the blood vessels and lower the blood pressure. Benazepril and enalapril are angiotensin converting enzyme inhibitors (ACE-I), having the main purpose of offsetting the effects of the activated RAAS.
Activation of the RAAS also has been identified as either causing or aggravating chronic kidney disease (CKD), excessively high blood pressure, and proteinuria (excess of proteins in the blood).
ACVIM says: only "modestly" restrict sodium
In the ACVIM's 2019 Consensus Statement, that panel of cardiologists recommends only "modestly" restricting sodium intake. Specifically, they state:
"Modestly restrict sodium intake, taking into consideration sodium from all dietary sources (including dog food, treats, table food, and foods used to administer medications) and avoid any processed or other salted foods."
In a January 2017 article, Dr. Anton C. Beynen reviewed sodium restricted diets for MVD-affected dogs and concluded:
"There is no evidence that sodium restriction improves clinical signs in canine cardiac disease. Worse still, there are good reasons for contraindication."
In the 2012 book, Applied Veterinary Clinical Nutrition, the authors of the chapter, "Nutritional Management of Cardiovascular Diseases", state this about sodium in dog foods:
"The sympathetic nervous system and the RAA system become increasingly activated as heart disease progresses. Thus, severe sodium restriction in animals with early heart disease could theoretically be detrimental by early and excessive activation of the RAA system (Pedersen 1996; Freeman, Rush et al. 2006). The results of one study reported that a low-sodium diet fed to dogs with asymptomatic CVD resulted in increased aldosterone concentrations and heart rate, with no improvement in cardiac size or function (Freeman, Rush et al. 2006). Because of the potential detrimental effects and lack of documented benefits of severe sodium restriction in asymptomatic disease, the authors recommend only mild sodium restriction (<100 mg/100 kcal) in asymptomatic heart disease (ISACHC Stages 1a and 1b) [Stages B1 and B2]."
"In dogs with ISACHC Stage 2 [late Stage B2 or early Stage C], the authors recommend moderate sodium restriction (i.e., <80 mg/100 kcal)."
Veterinary cardiology researchers feed low sodium dog foods to healthy dogs to intentionally activate their RAAS in order to test the effectiveness of ACE-inhibitor medications. For example, in a July 2022 article, Iowa State Univ. researchers fed nine healthy dogs a low-sodium diet of Hill's Prescription Diet h/d dry food for five days. Their levels of sodium reached such low levels that it resulted in steady activiation of the dogs' renin-angiotensin-aldosterone system (RAAS). The researchers intentionally wanted to activate the RAAS in order to conduct a study of dosages of the ACE-inhibitor benazepril.
And so, MVD-affected cavaliers should avoid low sodium diets, such as Hill's Prescription Diet h/d dry food (with only 17 mg sodium per 100 kcal, 0.12%). A solution to the question of what to feed the MVD-affected cavalier, is to choose a high-quality canned food with fresh, identifiable meats (for example, beef, turkey, chicken -- not "poultry" or "meat") as the main sources of protein and with a moderate amount of sodium (but not a low level), and avoid high sodium dry foods and treats.
RETURN TO TOP
August 21, 2023:
'Prescription' dog foods which are
hazardous to cavaliers' health
 Two
major dog food producers, Hill's and
Purina, are marketing 'prescription' dog foods to owners of dogs with mitral
valve disease. Both of these dry foods, Hill's Prescription Diet Heart Care
h/d and Purina Pro Plan CC Cardiocare, can be life-threatening to cavalier
King Charles spaniels diagnosed with mitral valve disease (MVD).
Two
major dog food producers, Hill's and
Purina, are marketing 'prescription' dog foods to owners of dogs with mitral
valve disease. Both of these dry foods, Hill's Prescription Diet Heart Care
h/d and Purina Pro Plan CC Cardiocare, can be life-threatening to cavalier
King Charles spaniels diagnosed with mitral valve disease (MVD).
Hill's Heart Care h/d
Hill's Heart Care h/d dry food has an excessively low quantity of sodium, which has been known to activate the dog's renin-angiotensin-aldosterone system (RAAS) in the kidneys. When a dog does not consume enough sodium, the RAAS is activated, narrowing the blood vessels and causing the kidneys to retain water and conserve sodium, thereby increasing the amount of fluid in the dog's body and raising its blood pressure.
This is a particularly serious problem for MVD-affected dogs, especially those in Stage C -- congestive heart failure -- because the main medication for removing fluid (including sodium in that fluid) from the lungs of these patients is a strong diuretic, such as furosemide or torsemide. The diuretic alone may signal to the kidneys that the sodium level is dropping. But when that is combined with an extremely low sodium dog food -- Hill's Heart Care h/d -- the RAAS is sure to be activated.
Avoiding activating of the RAAS is so important for cavaliers with MVD that they are prescribed medications specifically designed to prevent the RAAS from kicking in, mainly ACE-inhibitors such as enalapril and benazepril, and angiotensin receptor blockers (ARBs) such as telmisartan and Entresto.
Unlike humans with heart conditions, who are on strict low or no sodium diets, MVD-affected dogs need a moderate amount of sodium in their daily diets. In the ACVIM's 2019 Consensus Statement, the panel of cardiologists recommends only "modestly" restricting sodium intake. Specifically, they state:
"Modestly restrict sodium intake, taking into consideration sodium from all dietary sources (including dog food, treats, table food, and foods used to administer medications) and avoid any processed or other salted foods."
In a January 2017 article, Dutch Dr. Anton C. Beynen reviewed sodium restricted diets for MVD-affected dogs and concluded:
"There is no evidence that sodium restriction improves clinical signs in canine cardiac disease. Worse still, there are good reasons for contraindication."
Activation of the RAAS also has been identified as either causing or aggravating chronic kidney disease (CKD), excessively high blood pressure, and proteinuria (excess of proteins in the blood).
Hill's Heart Care h/d is so effective at activating the RAAS that veterinary researchers who investigate how to treat dogs with RAAS activation have fed this food to healthy laboratory dogs for the sole purpose of intentionally causing the dogs' RAAS to activate. See, for example, this July 2022 article, in which nine healthy dogs were fed Hill's Heart Care h/d for five days in order that their levels of sodium reached such low levels that it caused the dogs' RAAS to steadily activate.
Purina Pro Plan CC Cardiocare
Purina Pro Plan CC Cardiocare dry food is marketed to owners of MVD-affected dogs to lead them to believe that the food will slow of even halt enlargement of the dogs' left atria and left ventricles, the hallmarks of Stage B2 patients. In a recent peer-reviewed study conducted by an international team of veterinary cardiologists and nutritionists, published in a July 2023 article, they report finding that the claim is false.
The researchers tested Purina's Pro Plan CardioCare on a group of 101 MVD-affected dogs, including 29 cavaliers (29%), all in Stage B1, over a 365 day period to see if it met its claims that it would slow or arrest echocardiographic left heart enlargement in Stage B1 dogs. After a year of dogs being fed the Purina recipe or a control diet, the researchers reported that:
"In conclusion, a specially formulated diet [Purina Pro Plan CC Cardiocare dry food] was not associated with significant changes in LAD [left atrium dimension] and LVIDd [left ventricle dimension] when fed to dogs with mild subclinical DMVD for 1 year as compared to control diet." (Emphasis added.)
In other words, Purina Pro Plan CC Cardiocare dry food was no better than plain old kibble in treating MVD.
This food offers a dangerous double whammy to cavaliers because one of its main ingredients is medium chain triglycerides (MCTs). Purina apparently has failed to recognize that other studies have found evidence that a high percentage of cavaliers have a genetic deficiency of medium-chain acyl-coenzyme A dehydrogenase z9 (MCAD), causing epileptic seizures and more severe consequences when fed MCTs as their primary source of fat. Therefore, researchers are recommending that all CKCSs be genetically tested for a specific mutation of the ACADM gene which causes the MCAD deficiency, before including MCTs in their diets.
RETURN TO TOP
May 26, 2023:
Why some holistic canine nutritionists
may be their own worst enemies
 We have been feeding our cavalier King Charles spaniels (CKCSs) home-made
dog food recipes since the 1990s, all of which have been drafted by or
reviewed and approved by veterinarians who also have been trained and
certified in holistic care modalities. Over those 25+ years of making our
dogs' food, we have used more than a dozen different recipes, all tailored
to focus upon each dog's particular health issues.
We have been feeding our cavalier King Charles spaniels (CKCSs) home-made
dog food recipes since the 1990s, all of which have been drafted by or
reviewed and approved by veterinarians who also have been trained and
certified in holistic care modalities. Over those 25+ years of making our
dogs' food, we have used more than a dozen different recipes, all tailored
to focus upon each dog's particular health issues.
Even for a single dog, our recipes have changed because the dog's health issues have changed. Because all of our dogs have been cavaliers, most all of the recipes have focused largely upon mitral valve disease (MVD), but other conditions have been considered, especially gastro-intestinal ones. Some of the diets have been raw and others cooked, because the holistic vets have determined which would be best for each dog at the current stage of its life.
Keep it simple
If there is just ONE piece of advice we could give to holistic nutritionists after over two decades of making dog food at home, it would be: KEEP IT SIMPLE! The more complicated a recipe, the less compliance you should expect from the owners of your patients in following your recipe, or even in preparing the food from scratch at all.
We have seen some bizarre dog food recipe ingredients over the years, all surely drafted with the best of intentions by the holistic veterinarians, but also all quite nearly impossible to follow exactly. The three main types of crazy ingredients are:
(1) hard to find types of meats and vegetables and herbs, and
(2) minuscule quantities of meats and vegetables which usually are sold only in large quantities, and
(3) too many ingredients, like six or seven different types of vegetables and fruits instead of just two or three.
Examples of the first category - the hard to find ones - would be game meats, like kangaroo, rabbit, venison, and some rare types of seafood. Examples of the second category - minuscule quantities - would include a single oyster, or two clams. It is unrealistic to expect many dog owners to buy a pint of oysters just to retrieve a single one of them for their dogs' recipes, especially owners who are not seafood fans themselves.
MVD kills cavaliers! Dry eye syndrome does not
And if there were just TWO pieces of advice we could give, the other one would be: FOCUS ON THE MOST IMPORTANT HEALTH CONDITION the patient has, and not a secondary one. A recently published recipe for treating dogs with dry eye syndrome (keratitis sicca or keratoconjunctivitis sicca) brought this issue to our attention. Dry eye syndrome is one of the two most common health conditions suffered by CKCSs, the other being mitral valve disease (MVD). One of those is the leading killer of cavaliers; the other is dry eye.
Neither of these diseases is curable, short of complicated surgeries. But, dry eye is treatable with eye drops. MVD in cavaliers almost always keeps getting worse and worse, no matter how many drugs are given. Our dogs' diets always emphasize the most life-threatening or debilitating health conditions our dogs have been diagnosed as having. We treat the minor ones. like dry eye, with supplements and medications.
RETURN TO TOP
May 14, 2023:
Why do cavaliers' coat colors matter?
From a health standpoint, they do not
Eliminating coat colors may have spread CM and SM
Off-colors should be added to the breed standard
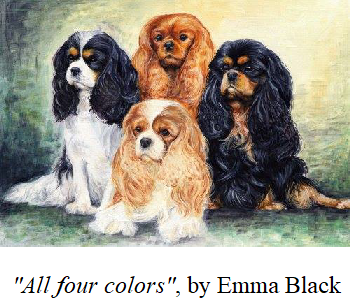 Today, one would think that cavalier King Charles spaniels (CKCS) can
come in only four color varieties - red-&-white (called "Blenheim"),
black-&-white-&-tan (called "tricolor" or "tricolour"), red (called "ruby"),
and black-&-tan (called "black-&-tan"). Indeed, the official breed standards
for the CKCS are limited to those four varieties of their coats.
Today, one would think that cavalier King Charles spaniels (CKCS) can
come in only four color varieties - red-&-white (called "Blenheim"),
black-&-white-&-tan (called "tricolor" or "tricolour"), red (called "ruby"),
and black-&-tan (called "black-&-tan"). Indeed, the official breed standards
for the CKCS are limited to those four varieties of their coats.
The breed standard for the United Kingdom's national cavalier club ("the World's Original Cavalier Club") lists those four "recognised colours" but also acknowledges the existence of other ones, by stating "Any other colour or combination of colours unacceptable." (See below.)
Historically, there have been more than just four colors
 The
documented history of this breed harks back at least to the toy spaniels of
the 1500s, before even the birth of King Charles I of England in 1600. In
that era in Great Britain, they were referred to simply as Toy Spaniels, and
at that time, they mainly came in two color combinations: Brown-and-White
and Black-and-White. By the time of King Charles II, the colors expanded by
adding the Tricolour, a combination of black, white, and reddish brown, and
what later would be called the Blenheim, reddish brown and white, as well as
a pure Black version. Later came the Black-and-Tan and the reddish Ruby and
the Brown and the Brown-and-Tan. This 1651 painting at the right is of King
Charles II of England, for whom the cavalier King Charles spaniel is named.
He is holding one of his brown-and-white toy spaniels, a color combination
no longer acceptable under the various national club breed standards.
The
documented history of this breed harks back at least to the toy spaniels of
the 1500s, before even the birth of King Charles I of England in 1600. In
that era in Great Britain, they were referred to simply as Toy Spaniels, and
at that time, they mainly came in two color combinations: Brown-and-White
and Black-and-White. By the time of King Charles II, the colors expanded by
adding the Tricolour, a combination of black, white, and reddish brown, and
what later would be called the Blenheim, reddish brown and white, as well as
a pure Black version. Later came the Black-and-Tan and the reddish Ruby and
the Brown and the Brown-and-Tan. This 1651 painting at the right is of King
Charles II of England, for whom the cavalier King Charles spaniel is named.
He is holding one of his brown-and-white toy spaniels, a color combination
no longer acceptable under the various national club breed standards.
To what other colors of cavaliers could the UK's breed standard be referring? Here is a list of "off-colors":
• Brown-and-White
• Black-and-White
• Brown (called Chocolate)
• Brown-and-Tan (called Chocolate Tan)
• Black
• Black-and-Brown
See these paintings of "off-color" King Charles spaniels by British artists dating back to the 1700s and 1800s:
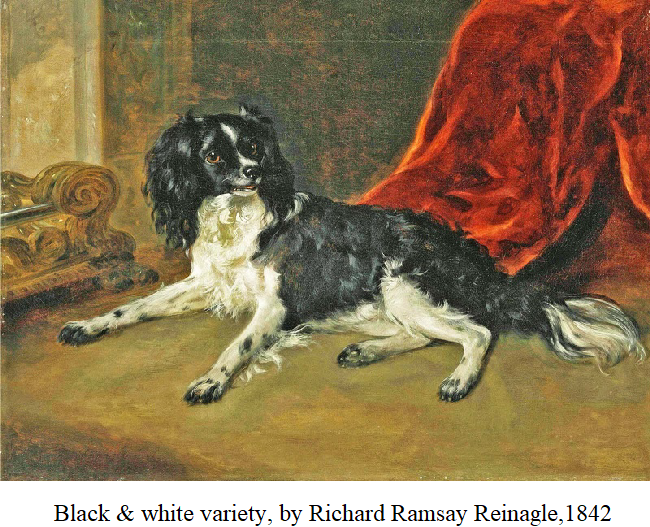
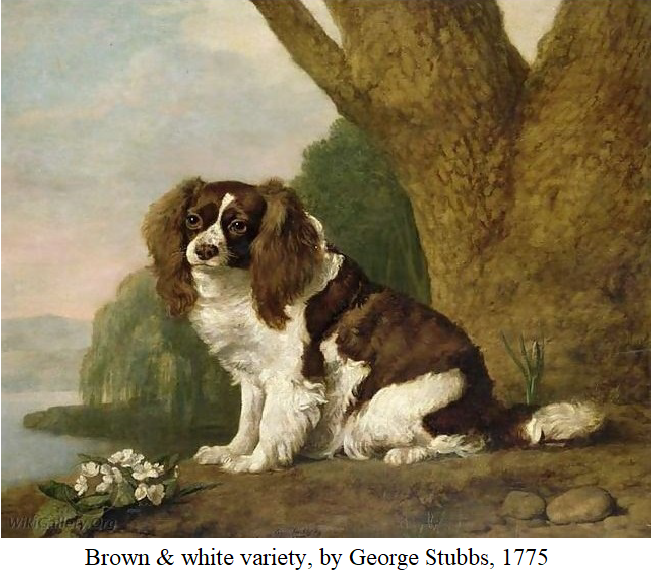
Lady Mary Forwood, a long-time breeder of cavaliers in England wrote in her 1967 book, The Cavalier King Charles Spaniel:
"It would appear that the Toy Spaniels of that day [1554] were mainly Brown and White and Black and White. In 1565, when Mary Queen of Scots was beheaded, a small Black/White dog was found under her skirts. This is generally thought to have been a Cavalier. ... As far as is known by all the paintings there were only the three colours in Charles II's time - the Brown/White, Black/White and Tricolour. ... Charles II's sister, Henrietta of Orleans, who was brought up from a baby in France, is pictured by Pierre Mguard with one of these little dogs in her lap, this one is a red and white spaniel. There is also a picture of the Dauphin with a black dog and a Black/White one, and one of Louis XIV with a beautiful Black/White Toy Spaniel. The Black/White are also very prominent in Watteau's Embarquement pour Cythere and La Toilette, to mention only two of his pictures."
So the blood and the genes of these off-colors are part of the foundation of the modern cavalier King Charles spaniel. In the original (1928) breed standard drawn up by the Committee of [the UK] Cavalier King Charles Spaniel Club, it states: "Colour: All recognized".
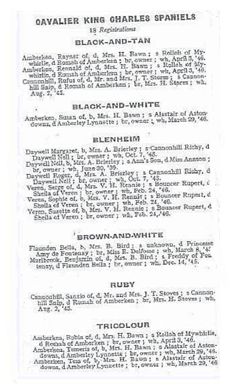 Among 18 cavaliers registered
with the UK's club in May 1945, two were brown-&-whites and one was a
black-&-white, comprising 17% of the registrations. (See May 1945
registration list at right.) And, these off-color
cavaliers even were registered and shown in UK conformation shows as late as
the 1970s. In 1971, Mrs. Amice Pitt of the UK club wrote of her preference
for the now-recognized four color combinations, and since 1973 all CKCS
breed standards have adhered to her choices. This decision appears to have
been based solely upon personal preference without any thought to breed
health consequences.The elimination of the other colors clearly has had a
major damaging effect upon the breed's gene pool.
Among 18 cavaliers registered
with the UK's club in May 1945, two were brown-&-whites and one was a
black-&-white, comprising 17% of the registrations. (See May 1945
registration list at right.) And, these off-color
cavaliers even were registered and shown in UK conformation shows as late as
the 1970s. In 1971, Mrs. Amice Pitt of the UK club wrote of her preference
for the now-recognized four color combinations, and since 1973 all CKCS
breed standards have adhered to her choices. This decision appears to have
been based solely upon personal preference without any thought to breed
health consequences.The elimination of the other colors clearly has had a
major damaging effect upon the breed's gene pool.
It appears that the vice president of the American Cavalier King Charles Spaniel Club (ACKCSC), John Ioia, is spreading falsehoods about the history of the various colors of the ancestors of the breed. He wrote in the September 2022 issue of the AKC Gazette:
"These are the four accepted colors of the CKCS and the only four accepted colors based on the history of our breed, beginning with its country of origin, England, and the 1600s." (Emphasis added.)
His "history" is totally false, as the details in this blog article establish. But the ACKCSC is notorious for making stuff up. That club has not provided any redeeming value among its "contributions" to the CKCS breed.
Off-color cavaliers have no unique health issues
But limiting the official, recognized coat colors to just those four, did not affect the genetic potential of the breed to continue to produce the off-color coats that had been in the breed for hundreds of years. Since 1971, purebred cavaliers have been bred to other purebred cavaliers and have produced offspring of black-&-whites, brown-&-whites, brown-&-tans, and all blacks. Since these varieties are not eligible to compete in CKCS conformation events, most all breeders have tried to eliminate such genes from their breeding stock. In most all cases, they have been successful, so the production of off-color cavaliers today is quite rare. But such offspring are not inconceivable, and a few breeders still find off-colors among their litters.
Susan Cochran, a long-time breeder of cavaliers in the United States, has
being finding "chocolate" colored
 cavalier puppies in her
purebred CKCS litters since the
1980s. (See her "chocolate tan" Cochran's Kitkat, at right.) She writes:
cavalier puppies in her
purebred CKCS litters since the
1980s. (See her "chocolate tan" Cochran's Kitkat, at right.) She writes:
"In 1985, we purchased a very pretty Blenheim from Canada. She was from a mating of Can. Ch. Kilspindie Bryony of Beauchamps and Ch. Kindrum Simon of Silvercrest. Her name was Beauchamps Royal Flirtation and we called her "Flirt". We found, years later, that Flirt was a carrier for the rare chocolate color gene that runs in the longevity bloodlines of Cavalier King Charles Spaniels. Flirt lived 15+ years and was a healthy, sweet, affectionate Cavalier. She is behind all of our dogs and was our foundation female. ... The Chocolate gene expresses itself as Chocolate Tan or Chocolate Tri. They are registered with AKC. I have also registered Chocolates with the CKCSC, USA."
Since our concern primarily is with the health of cavaliers, we have looked into whether any purebred off-colors are more or less vulnerable to the disorders known to affect the CKCS, or even if the off-colors tend to develop other diseases to which the recognized colors seem immune. We have found no such evidence. The only differences between cavaliers of the "recognized" colored coats and the formerly recognized off-color coats are the colors of the coats. The recognized colors were chosen based solely upon personal preferences of such breeders as Mrs. Pitt, and not due to any health issues whatsoever.
Eliminating coat colors may have spread CM and SM
Unfortunately, from a genetic health standpoint, the elimination of the off-colors has served as one more step in reducing the CKCS gene pool, which is very undesirable, as a general rule. In a September 2004 article, the investigators presented evidence that selection for coat color has not only narrowed the CKCS gene pool, but also has influenced the spread of Chiari-like malformation (CM) and syringomyelia (SM) throughout the breed.
It may be too late to rescue the CKCS breed from the deleterious health effects resulting from the elimination of the off-colors, but it is not too late to add them again. Considering that the only alternative approach to refreshing the gene pool has been to crossbreed with other breeds and then backcross, the insertion of off-color purebred cavaliers certainly is a less risky method of refreshing the gene pool.
RETURN TO TOP
March 11, 2023:
Are medium chain triglycerides (MCTs)
hazardous to many cavalier King
Charles spaniels?
A recent study finds the answer is YES!
 Medium
chain triglycerides (MCTs) are fats derived from coconut oil and
palm kernel oil. They have been found to be more rapidly absorbed into the
canine digestive system than other dietary oils.
Medium
chain triglycerides (MCTs) are fats derived from coconut oil and
palm kernel oil. They have been found to be more rapidly absorbed into the
canine digestive system than other dietary oils.
Various claims have been made on the Internet websites of MCTs vendors, including so-called "natural solution" veterinarians, that MCTs made from "virgin coconut oil" will resolve dogs suffering from epilepsy, gastrointestinal disorders, and even mitral valve disease, and all sorts of other undesirable disorders.
In fact, there is veterinary literature evidence to support some of these claims of health benefits to dogs, when treated with MCTs. One study reported that dogs fed a diet high in MCTs had a significant reduction in the frequency of epileptic seizures when compared with control dogs in that study.
Another journal article reports that MCTs are beneficial in treating gastrointestinal symptoms due to protein-losing enteropathy (PLE). And still another one claims that a combination of supplements including MCTs was "able to slow or reverse cardiac changes in dogs with early, preclinical MMVD [mitral valve disease]."
A dog food containing MCTs is marketed specifically for epileptic dogs, advertising that the MCTs will reduce seizure frequency. Another dog food is advertised that the MCTs in its ingredients "support cardiac function in dogs".
Why CKCSs should avoid MCTs
All that said, however, it appears that MCTs are a serious health hazard for a high percentage of cavalier King Charles spaniels.
MCAD (medium-chain acyl-coenzyme A dehydrogenase) is an enzyme which is controlled by a specific gene in canines, called the ACADM gene. A mutation of that gene in dogs causes a MCAD-deficiency in the dogs with that mutation. MCAD-deficiency is a presumably inherited disorder called an organic aciduria that prevents the dog's body from converting certain fats to energy, particularly medium-chain fatty acids.
Two published studies suggest that MCAD-deficiency is fairly common among CKCSs. In a May 2007 article, veterinary neurologists report finding that a young cavalier, exhibiting seizures which were not controllable with anti-convulsants (potassium bromide, phenobarbital, and gabapentin), had an organic aciduria with excessively high urine excretion of hexanoylglycine. They diagnosed a MCAD-deficiency.
In an October 2022 study of 162 cavaliers, researchers found that 52 of them were carriers of the protein changing variant of ACADM, and another 12 CKCSs were homozygous mutant dogs - 39.5% of the 162 cavaliers in the study. That research was prompted by examination of a 3 year old, male neutered cavalier which displayed complex focal seizures and prolonged lethargy. The dog was found to have a single insertion deletion variant of ACADM causing the MCAD deficiency. The affected dog was treated with various dosages of levetiracetam and phenobarbital and was prescribed a low fat diet and a midnight snack consisting of carbohydrates. Prolonged periods of fasting and formulas that contained medium chain triglycerides as primary source of fat were also advised to avoid.
Fats are one of the three essential categories of food nutrients, the others being proteins and carbohydrates. In short, CKCSs affected with the MCAD-deficiency cannot digest MCTs, and so when MCTs are the primary or sole source of fats in their diets, they digest no fats. In humans, MCAD-deficiency has been found to lead to severe liver disorders, atrophy of the skeletal muscles, loss of consciousness, coma, and even sudden death.
The authors of the leading (November 2020) veterinary journal article finding that MCT oils improve dogs' cognitive abilities now advise that MCT-enriched diets may be inappropriate for some CKCSs, based upon the findings of the October 2022 study. They recommend having cavaliers tested for the ACADM mutation before feeding MCT-enriched diets for those dogs.
So, the answer to the question in the title is: Yes, MCT oils, including coconut oil, should not be fed to any cavalier unless that dog first has been tested clear for the ACADM mutation causing the MCAD-deficiency.
Short of DNA testing* for the MCAD-deficiency
(MCADD), the best solution would be
to avoid dog foods which have MCTs as their primary oils
(e.g., ketogenic diets, Purina Pro Plan Bright Mind, Purina Pro
 Plan
CardioCare) and also MCT oil supplements (e.g., coconut oil).
Plan
CardioCare) and also MCT oil supplements (e.g., coconut oil).
This Facebook group is dedicated to this disorder in cavaliers.
* Laboklin offers a DNA test for the MCADD genetic mutation. See this link.
RETURN TO TOP
November 26, 2022:
When not to separate cavalier puppies from their mothers - before the 14th week
Cavaliers need longer periods with their mothers and siblings
than the
average puppy
It generally is accepted that early life experiences are of prime importance in shaping later behaviors. This appears to be as true with canines as with humans and other mammal species. We call this process "socialization" (or "socialisation" in UK parlance) - the learning process of interacting acceptably with others.
 Puppy
socialization consists of a variety of sub-sets. They include interacting
(a) with the puppy's mother, (b) with its fellow siblings and other dogs,
preferably in the breeder's home or kennel, (c) and with humans. A lack of
proper and timely socialization with other dogs has been found to result in
higher levels of fear of other dogs. Similarly, the same is the case with
lack of timely, positive contacts with humans - fear of people.
Puppy
socialization consists of a variety of sub-sets. They include interacting
(a) with the puppy's mother, (b) with its fellow siblings and other dogs,
preferably in the breeder's home or kennel, (c) and with humans. A lack of
proper and timely socialization with other dogs has been found to result in
higher levels of fear of other dogs. Similarly, the same is the case with
lack of timely, positive contacts with humans - fear of people.
Puppies are said to have a sensitive period for this dog and human socialization in their early post-natal life, during which their neurological and emotional development is immature and most receptive for novel external stimuli of all of their senses. (Kinsman, August 2020 article.) This early process of learning behavioral patterns sometimes is called "imprinting". This time period, found to occur especially from the third week to the fourteenth week of age, can significantly affect a dog's behavior throughout its life. (Freedman, March 1961 article; Morrow, July 2015 article.)
It is during the third week that most puppies' eyes and ears
become functional, and they become more mobile. (Stolzlechner, November 2022
article.) This is followed by an initial fear response exhibited by puppies
 to sudden sounds and other startling novel events, which has been found to
develop around the sixth or seventh week, give or take up to a couple of
weeks, depending upon the breed and particular dog. The puppy's typical
reaction to fearful events is avoidance. Recent research has found that this
fear of novelty - leading to increased avoidance - continues to increase in
intensity until the twelfth to fourteenth week. (Stolzlechner, November 2022
article.)
to sudden sounds and other startling novel events, which has been found to
develop around the sixth or seventh week, give or take up to a couple of
weeks, depending upon the breed and particular dog. The puppy's typical
reaction to fearful events is avoidance. Recent research has found that this
fear of novelty - leading to increased avoidance - continues to increase in
intensity until the twelfth to fourteenth week. (Stolzlechner, November 2022
article.)
And so, an important window of opportunity exists for both puppy-to-other-dogs socialization and puppy-to-humans socialization during those weeks from the third to up to fourteenth. It would appear that the best source for providing these new sensory stimulations to other dogs and humans on a consistent and continuing knowledgeable basis, would be the puppy's breeder.
All of this brings us to the uniqueness of the cavalier King Charles spaniel as a breed. Published studies have found these characteristics about the development of the cavalier's nervous system:
• Cavalier puppies tend to have their eyes open and begin weaning and exploration at a later age than many other breeds. (Morrow, July 2015 article.)
• Unlike other breeds (e.g., including German shepherd dogs and Yorkshire terriers in the Morrow, July 2015 study) cavalier puppies failed to respond to any stimuli until five weeks of age, rather than the usual three weeks. (Morrow, July 2015 article.)
• Cavalier puppies demonstrated a significantly later onset of fear-related avoidance behavior (compared with both the Yorkshire terrier and German shepherd dog puppies in the 2015 study) (Morrow, July 2015 article.)
• Cavaliers appear to require a longer socialization period than other breeds. (Morrow, July 2015 article.)
Notwithstanding this evidence, CKCS breed clubs adhere to a species-wide policy of recommending that cavalier puppies be transferred from breeder to buyer as early as the eighth week.
In the United Kingdom (UK), the Cavalier King Charles Spaniel Club's Code of Ethics provides that "Members who breed or exhibit should: ... Not part with a puppy under the age of eight weeks to a new owner." That club also requires that its members "Will abide by all aspects of the Animal Welfare Act.'
Interestingly, the UK's "Animal Welfare (Licensing of Activities Involving Animals) (England) Regulations (2018 ed.)" states at Schedule 6, Section 1(5):
"No puppy aged under 8 weeks may be sold or permanently separated from its biological
mother."
So, separating puppy from mother, litter, and breeder is condoned ethically and legally in the UK at eight weeks of age.
The American Kennel Club (AKC) recommends that:
"You should not expect to bring a puppy home until it is between eight to 12 weeks of age. Puppies need ample time to mature and socialize with their mother and littermates to set them up for success in their future homes."
This, of course, is a species-wide recommendation - in other words, for all puppies of all breeds - and therefore is not based upon any scientific basis, because all breeds are not alike.
The American Cavalier King Charles Spaniel Club (ACKCSC - the AKC's
"parent" club for cavaliers) goes one step
 further by stating in its
"ethical guidelines" that:
further by stating in its
"ethical guidelines" that:
"I [meaning, the cavalier puppy's breeder] will not allow any puppy to leave for its new home before the age of eight weeks although twelve weeks is suggested."
The Cavalier King Charles Spaniel Club, USA, (CKCSC,USA) has a code of ethics which includes this statement:
"I [the cavalier puppy's breeder] will not allow any puppy to leave for its new home before the age of eight weeks. The CKCSC recommends ten to twelve weeks as the appropriate age for transfer."
Contrary to all of the above regulations, cavalier club ethical codes, and recommendations, it is quite clear that separating pup from mother, litter, and breeder prior to the fourteenth week is not in the best interests of the long-term healthy development of cavaliers. Cavaliers in general have their peculiarities, and among them is their overly slow development from birth to their fourteenth week.
Cavaliers need to be socialized longer than other breeds, and that socialization should be with mother, siblings and other dogs, and humans, on a consistent and continuing basis from their weaning until at least their fourteenth week.
------
REFERENCES:
Freedman: Critical Period in the Social Development of
Dogs. Daniel G. Freedman, John A. King, Orville Elliot. Science. March 1961;
doi: 10.1126/science.133.3457.10.
Kinsman: Puppy acquisition: factors
associated with acquiring a puppy under eight weeks of age and without
viewing the mother. Rachel H. Kinsman, Rachel A. Casey, Toby G. Knowles,
Severine Tasker, Michelle S. Lord, Rosa E. P. Da Costa, Joshua L. Woodward,
Jane K. Murray. Vet. Rec. August 2020: doi: 10.1136/vr.105789.
Morrow: Breed-dependent differences in the onset of fear-related avoidance
behavior in puppies. Mary Morrow, Joseph Ottobre, Ann Ottobre, Peter
Neville, Normand St-Pierre, Nancy Dreschel, Joy L. Pate. J. Vet. Behavior.
July 2015; doi: 10.1016/j.jveb.2015.03.002.
Pirrone: The importance
of educating prospective dog owners on best practice for acquiring a puppy.
Federica Pirrone. Vet. Rec. August 2020; doi: 10.1136/vr.m3024.
Stolzlechner: Optimising Puppy Socialisation-Short- and Long-Term Effects
of a Training Programme during the Early Socialisation Period. Lisa
Stolzlechner, Alina Bonorand, Stefanie Riemer. Animals. November 2022; doi:
10.3390/ani12223067.
RETURN TO TOP
September 15, 2022:
Beware of Internet advice to stop treating
MVD-affected dogs with
prescription medications
We recently discovered on the website of a retired veterinarian who sells herbs for treating a variety of disorders in dogs and cats, that she also includes a webpage in which she is selling a combination of products called "Five Leaf Botanicals Canine Heart Health Program for Canine Heart Disease".
 The "program", selling for $145.00 plus shipping
per month, consists of five
products:
The "program", selling for $145.00 plus shipping
per month, consists of five
products:
• a bottle of "Canine Heart Tonic" containing a variety of herbal tinctures;
• a bottle of "Hawthorne Tincture" (a misspelling of hawthorn);
• a jar of "Dog Greens" containing a combination of algae and grasses;
• a jar of "L-Carnitine", an amino acid derivative ;
• a jar of "Taurine", another amino acid derivative;
• a pamphlet telling how the dog should be fed these ingredients over a 30-day period.
If the dog has been diagnosed with mitral valve disease (MVD), and especially if the dog has an enlarged heart (Stage B2) or also has progressed to heart failure (Stage C), some of these ingredients may be modestly beneficial to the heart, but certainly two of them - the l-carnitine and the taurine - will serve only to produce more expensive urine.
L-carnitine: To date, no published veterinary literature has found that L-carnitine supplementation aids in slowing the progression of MVD in dogs, either before or after the onset of heart failure. Most dogs make enough l-carnitine from the foods they consume. Studies have shown that MVD-affected dogs, particularly those in heart failure (CHF - Stage C or D) tend to have higher concentrations of l-carnitine in their blood serum than do healthy dogs. Read more about it here.
Taurine: This synthetic is not an appropriate supplement for MVD-diagnosed dogs unless taurine concentrations in the dogs' blood has been found to be low. Research studies have shown that MVD-affected dogs tend to have higher plasma taurine concentrations than unaffected dogs. Veterinary cardiologist Dr. Bruce Keene has stated: "Taurine supplementation is indicated whenever plasma or whole blood taurine concentrations are found to be low. ... [S]upplementation is generally only recommended after discovery of deficiency." Read more about it here.
So, right off the bat, two of the five items are a waste, both of money and of the dog's digestive processes. But the most disturbing thing about this "Canine Heart Health Program" is the advice on that webpage to stop giving the MVD-affected dog its heart medications - namely pimobendan in Stages B2, C, and D, and diuretics in Stages C and D - and instead treat the dog only with these supplements. To be specific, it states on the webpage:
"[I]t is important to recognize the danger of pharmaceuticals and the effectiveness of quality herbal preparations. Herbs work best without toxic drugs; many people do not see the desired improvement in their dog's health by using pharmaceuticals and seek out natural healing as an alternative. ... The fact of the matter is while our formulae are safe to take with pharmaceuticals, herbs and pharmaceutical drugs do not compliment each other. Herbs support the body and help in healing the injured or disease area whereas drugs do the heart's job, do not support healing and can be extremely toxic. ...
"If your dog is currently on prescription medication and if you wish to heal his heart naturally, weaning him off the drugs is crucial. Gradually wean him off over a period of a few weeks to a month."*
Even worse than the advertising of these products by the former
veterinarian is the website of the lady who is the ultimate seller of these
products. She describes
 herself as an "Herbalist". On her website, she
insists that her "Canine Heart Health Healing program", consisting of a few
herbs and a couple of un-needed amino acid derivatives (synthetic versions
of L-carnitine and
taurine), is intended to heal the hearts of dogs diagnosed with
valvular disease and congestive heart failure, without continuing to take
the drugs prescribed by the dogs' cardiologists. It has been well
established in veterinary literature that diseased mitral valves do not
"heal".
herself as an "Herbalist". On her website, she
insists that her "Canine Heart Health Healing program", consisting of a few
herbs and a couple of un-needed amino acid derivatives (synthetic versions
of L-carnitine and
taurine), is intended to heal the hearts of dogs diagnosed with
valvular disease and congestive heart failure, without continuing to take
the drugs prescribed by the dogs' cardiologists. It has been well
established in veterinary literature that diseased mitral valves do not
"heal".
We believe it is irresponsible for anyone to recommend that for any MVD-affected dog being treated with pimobendan (in Stages B2, C, and D) and a diuretic like furosemide (in Stages C and D) to stop giving those medications and instead give the dog only a few herbs and amino acids. The only exception would be if the dog cannot tolerate the pimobendan or diuretic due to significant adverse reactions.
* September 18, 2022 Update: Since the date of this post
(September 15, 2022) the content of the "Canine Heart Health Program" webpage
on the former veterinarian's website has been revised to the
extent that in the first paragraph quoted above, the phrase "herbs and
pharmaceutical drugs do not compliment each other" has been deleted, and
that the second paragraph now states: "If your dog is currently on prescription medication and if you wish to
heal his heart naturally, weaning him off the drugs may be possible with the
support of your cardiologist. Gradually
wean him off over a period of a few weeks to a month under the supervision
of your cardiologist." Nevertheless, that webpage continues to advise that
"Herbs work best without toxic drugs" and that "drugs ... do not support
healing, and can be toxic", and recommends that the dog be "weaned off" of
the "prescription medication" and the dog be given only the herbal formulas.
June 22, 2023 Update: Today, the United States Food & Drug
Administration (FDA) issued a
Warning Letter to Five Leaf Pet Botanicals, stating that its Canine
Heart Tonic and Hawthorne Tincture "are unapproved new animal drugs and
introducing or delivering these products for introduction into interstate
commerce is prohibited under section 301 (a) of the FD&C Act [21 U.S.C. §
331 (a)]. These products are also sold as part of packages which include,
but may not be limited to, "Canine Heart Health Packages (One, Two, Three,
and Four). ... Therefore, the products are unsafe within the meaning of
section 512(a) of the FD&C Act, [21 U.S.C. § 360b(a)], and adulterated under
section 501(a)(5) of the FD&C Act [21 U.S.C. § 351(a)(5)]."
RETURN TO TOP
August 24, 2022:
Giving your cavalier a bone will not prevent or treat
dental disease and
may fracture teeth
 Giving
the dog a bone is not the answer to either preventing or treating
periodontal disease. While
periodontal disease (PD)
affects the teeth, it actually is an inflammatory disease of the
periodontium -- the gums, periodontal ligament, cementum, and/or alveolar
bone.
Giving
the dog a bone is not the answer to either preventing or treating
periodontal disease. While
periodontal disease (PD)
affects the teeth, it actually is an inflammatory disease of the
periodontium -- the gums, periodontal ligament, cementum, and/or alveolar
bone.
PD usually is a late stage of a series of infectious disorders which begin when bacteria which enters the dog's mouth adheres to its teeth, both above and below the gumline, and to the gums themselves in the form of a biofilm (a complex accumulation of microbes) called plaque. Plaque can attach to the teeth and gums within twenty-four hours if not subject to daily cleaning.
Periodontal disease is infection below the gumline
Plaque on the tooth surface above the gumline is called supragingival plaque. Supragingival plaque can be treated and then reversed in most cases by daily dental care. Within three days, undisturbed plaque becomes calcified by minerals in the dog's saliva, becoming calculus or tartar.
If the plaque is not removed by daily cleaning, the bacteria adheres to the gums (the gingiva) and causes inflammation which is called gingivitis. This process can occur in as early as two weeks.
If left untreated, the plaque will advance by extending under the gums between the teeth and underlying alveolar bone, a stage called subgingival plaque. The presence of the darkened tartar on the visible crowns serve as an early warning that the dog has a potential PD problem which needs professional veterinary attention. Therefore, the plaque must be removed from both above and below the gumline to defeat the progression of the gingivitis to becoming PD.
While the hardened tartar is visible on the crown of the teeth as a stained coating, that does not cause PD. It is the plaque beneath the gumline -- the subgingival plaque -- which causes gingivitis, the precursor of PD.
Bone chewing will not remove plaque beneath the gumline
Chewing on bones will not remove plaque beneath the gumline. In a February 2020 article, a team of Brazilian veterinary dental researchers studied the effects of twelve Beagles chewing either sterile cortical (hard) bovine femur bones or sterile spongy bovine femur bones over a two week period, to evaluate the effect of bone chewing on the dental roots, enamel, and gingiva of the dogs. They report that both types of bones "were highly effective in removing dental calculus" and gingival inflammation reduction, with the spongy bones being more effective than the hard ones. Dental calculus was completely removed from the first and second premolars and molars in less than three days. No lesions or teeth root and enamel fracture, or esophageal or intestinal obstructions were observed. However, the spongy showed some gingival lesions and bone remnants between the dogs' teeth. Gingival lesions were caused by the daily and continuous supply of new pieces of bone for the 13 days. However, the bones failed to cure or even partially treat periodontal disease, which is a below-the-gumline disorder. They stated:
"Although there was an improvement in the visual appearance of the gum, there was no reduction in plaque and calculus under the gumline. The maintenance of subgingival [below the gumline] plaque and calculus is the etiological factor of loss of dental adhesion to its alveolus, characteristic to periodontal disease. Thus, bones are not efficient in removing plaque and calculus under the gumline, they are only able to remove it on the crown."
Chewing on bones can break the dog's teeth
 Dogs
also can fracture their teeth by chewing on bones. When veterinary
specialist
Dr. Jan Bellows was asked, "How can I prevent my dog from
fracturing more teeth?", he responded: "Examine your dog's treats and chew
toys. Eliminate any bones, antlers, cow hoofs, nylon chews, and pizzle
sticks. Throw out chews or toys that do not readily bend."
Dogs
also can fracture their teeth by chewing on bones. When veterinary
specialist
Dr. Jan Bellows was asked, "How can I prevent my dog from
fracturing more teeth?", he responded: "Examine your dog's treats and chew
toys. Eliminate any bones, antlers, cow hoofs, nylon chews, and pizzle
sticks. Throw out chews or toys that do not readily bend."
Broken teeth cause pain and may lead to infection, especially if the inner pulp is exposed. (See photo at right of exposed pulp in a broken tooth.) Infection in turn may lead to abscesses and jaw bone weakness.
RETURN TO TOP
July 20, 2022:
Peer-reviewed breed-specific ranges of normal-sized left atria (LA/Ao) and left ventricles (LVIDDN) in cavalier King Charles spaniels
Left atrium/aorta ratio (LA/Ao)
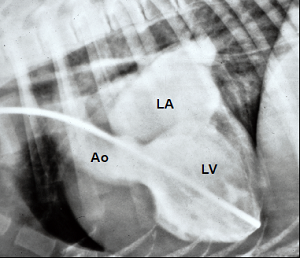 The 2016 EPIC Study (1) and the 2019 ACVIM Consensus Statement
(2) both
have defined left atrial (LA) enlargement in dogs diagnosed with myxomatous
mitral valve disease (MMVD), on a species-wide basis, as having a left
atrium to aorta ratio (LA/Ao) of 1.6 or more. The authors of these two
articles cited no scientific evidence to support such a definition. They
simply arbitrarily selected that 1.6 ratio as the cut-off between a normal
sized LA and an enlarged LA for all of the dogs in the world.
The 2016 EPIC Study (1) and the 2019 ACVIM Consensus Statement
(2) both
have defined left atrial (LA) enlargement in dogs diagnosed with myxomatous
mitral valve disease (MMVD), on a species-wide basis, as having a left
atrium to aorta ratio (LA/Ao) of 1.6 or more. The authors of these two
articles cited no scientific evidence to support such a definition. They
simply arbitrarily selected that 1.6 ratio as the cut-off between a normal
sized LA and an enlarged LA for all of the dogs in the world.
There have been dozens of peer-reviewed veterinary journal articles advocating breed-specific ranges of LA/Ao ratios in order to distinguish normal-sized left atria from enlarged ones in MMVD-affected dogs. Many of these articles were published prior to even the 2011 start of the EPIC Study. A list of several of them may be found at this link.
One of the breeds fortunate enough to have published LA/Ao data is the cavalier King Charles spaniel (CKCS).There are at least four peer-reviewed veterinary journal articles documenting the LA/Ao ranges (and/or means) of the dimensions of normal-sized left atria in heart-healthy CKCSs. They are labeled here as Haggstrom 1995 (3), Hansson 2002 (4), Misbach 2014 (5), and Bagardi 2022 (6). One other one, Wilshaw 2022 (7), provides LA/Ao ratio ranges for Stages B1 and C cavaliers.
Three of these articles were published before the 2016 publication of the EPIC Study results. The Hansson 2002 article actually was cited by the authors of the EPIC Study (at footnote 14) and the 2019 ACVIM Consensus Statement (at footnote 45), and one of the three lead investigators in the EPIC Study as well as one of the ten authors of the Consensus Statement (Haggstrom in both) was a co-author of that Hansson 2002 article.
The EPIC Study authors knowingly chose this arbitrary, scientifically baseless species wide cut-off definition of enlarged LAs even though over 45% of all dogs in their EPIC Study were cavaliers.
The cavaliers in these five breed-specific articles were either heart-healthy without MMVD (Stage A) or had been diagnosed as having only a murmur and no enlargement (Stage B1) or had reached heart failure (Stage C). The detailed findings in the five articles are in the Table below.
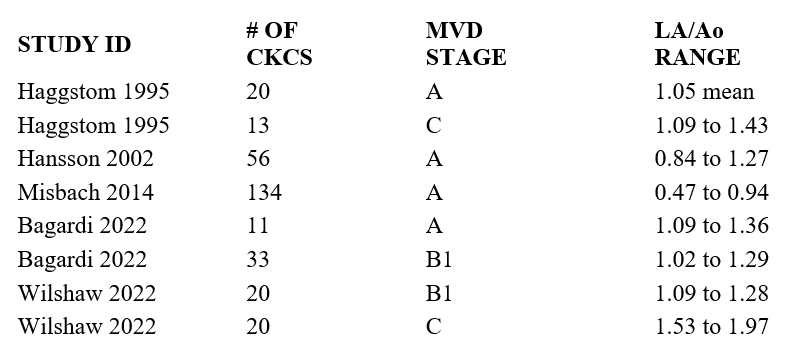
In none of these reported articles is any heart-healthy cavalier's LA/Ao anywhere close to the EPIC's and ACVIM's 1.6 cut-off ratio. In two of the articles, CKCSs already in heart failure - Stage C - have LA/Ao values well below the EPIC's and ACVIM's 1.6 cut-off of allegedly normal-sized LAs.
Diastolic left ventricular normalized dimensions (LVIDDN)
The EPIC's and ACVIM's species-wide definition of enlarged left ventricles (LV), using the diastolic left ventricular normalized dimensions (LVIDDN), likewise is totally unscientific and arbitrary. In an August 2022 article (8), Drs. Mark Rishniw and Donald J. Brown studied the echocardiograms of 59 CKCSs. They concluded that the EPIC and 2019 ACVIM definition of enlargement of the LVIDDN, being greater than the value of 1.7, was "arbitrarily chosen" and that over 10% of healthy dogs in the study, including the cavaliers, would be mis-classified as having enlarged LVs when in fact they had normal-sized LVs. They single out five specific breeds, including the CKCS, as having larger normal-sized LVs than average dogs of similar size. They state:
"The EPIC study employed an essentially arbitrary value of LVIDDN to dogs subsequently randomized to treatment with pimobendan or placebo and showed that dogs with LVIDDN>1.7 (and LA:Ao>1.6 and a VHS>10.5V) generally do better with the drug than without. ... The criterion for left ventricular enlargement used by the EPIC investigators for study inclusion has never been critically evaluated as indicative of left ventricular enlargement. ...
"We should note, however, that the definition of LV enlargement proposed by both the EPIC trial and, subsequently, by the ACVIM Consensus panel, is not a reference value, but a somewhat arbitrarily chosen threshold for inclusion in the EPIC trial. Therefore, clinicians adhering to these guidelines should be cautious in ascribing LVIDDN that exceed the threshold value of 1.7 as being indicative of LV enlargement. Furthermore, clinicians should note that the ACVIM Stage B2 classification requires enlargement of both the left atrium (to a LA:Ao>1.6) and enlargement of the left ventricle. How many dogs with mild left atrial enlargement, but without LV enlargement, might consequently be misclassified as having cardiomegaly remains unknown."
Drs. Rishniw and Brown warn that such breeds as the CKCS "likely require breed-specific reference intervals for LVIDDN to correctly identify left ventricular enlargement." Specifically for the 59 cavaliers in the study, they determined that the upper limit for normal-sized LVIDDN should have a scaling exponent of 0.33 (compared to EPIC's and ACVIM's arbitrary, species-wide exponent of 0.294), and that the range of LVIDDNs derived using 0.33 would be from 1.62 to 1.71 with a mean of 1.69.
------
REFERENCES:
1. Boswood A., Effect of Pimobendan in Dogs with Preclinical Myxomatous Mitral Valve Disease and Cardiomegaly: The EPIC Study--A Randomized Clinical Trial. J. Vet. Int. Med. November 2016;30(6):1765-1779.
2. Keene, B.W., ACVIM consensus guidelines for the diagnosis and treatment of myxomatous mitral valve disease in dogs. J. Vet. Intern. Med. May 2019;33(3):1127-1140.
3. Haggstrom J., Heart sounds and murmurs: changes related to severity of chronic valvular disease in the Cavalier King Charles spaniel. J. Vet. Intern. Med. March 1995;9(2):75-85.
4. Hansson, K., Left atrial to aortic root indices using two-dimensional and M-mode echocardiography in cavalier King Charles spaniels with and without left atrial enlargement. Vet. Rad. & Ultra. November 2002;43(6):568-575.
5. Misbach, C., Echocardiography and conventional Doppler examination in clinically healthy adult Cavalier King Charles Spaniels: effect of body weight, age, and gender, and establishment of reference intervals. J. Vet. Cardio. June 2014;16(2):91-100.
6. Bagardi, M., Circulating miR-30b-5p is upregulated in Cavalier King Charles Spaniels affected by early myxomatous mitral valve disease. PlosONE. July 2022;17(7):e0266208.
7. Wilshaw, J., Evidence of altered fatty acid metabolism in dogs with naturally occurring valvular heart disease and congestive heart failure. Metabolomics. May 2022;18:34. Note: CKCSs comprised 20 of the 30 MMVD-affected dogs in this study (67%).
8. Rishniw, M., The ACVIM consensus statement definition of LV enlargement in myxomatous mitral valve disease does not always represent LV enlargement. J. Vet. Cardiol. August 2022;42:92-102.
RETURN TO TOP
July 10, 2022:
Japanese mitral valve surgeons at JASMINE
report their MVD surgery
statistics
 At
a July 10, 2022 Internet webinar, the veterinary surgery team at the Japan
Animal Specialty Medical Institute (JASMINE) Veterinary Cardiovascular
Medical Center reported on the their mitral valve disease (MVD) repair
surgery procedures and post-operation statistics. JASMINE has been the
world's leading mitral valve repair center for MVD-affected dogs since its
inception in 2014. Drs. Masami Uechi, Masashi Mizuno, Sayaka Takeuchi and
their team have performed over 1,800
mitral valve repair surgeries as of April 2022. The vast majority of their
canine patients have been from Japan, but they also have treated 110 dogs
from overseas and have performed 103 additional surgeries at clinics
elsewhere in the world.
At
a July 10, 2022 Internet webinar, the veterinary surgery team at the Japan
Animal Specialty Medical Institute (JASMINE) Veterinary Cardiovascular
Medical Center reported on the their mitral valve disease (MVD) repair
surgery procedures and post-operation statistics. JASMINE has been the
world's leading mitral valve repair center for MVD-affected dogs since its
inception in 2014. Drs. Masami Uechi, Masashi Mizuno, Sayaka Takeuchi and
their team have performed over 1,800
mitral valve repair surgeries as of April 2022. The vast majority of their
canine patients have been from Japan, but they also have treated 110 dogs
from overseas and have performed 103 additional surgeries at clinics
elsewhere in the world.
Their typical open heart surgery involves replacing damaged mitral chordae tendineae - the tendons which control the opening and closing of the valve - with GoreTex struts, and tightening the valves themselves with GoreTex thread sutures to improve closure (called annuloplasty). Nearly half (47%) of their patients have been Chihuahuas, the most popular small breed in Japan that is prone to MVD. Thus far, only 4% of their patients have been cavalier King Charles spaniels. They currently are performing nine to ten surgeries each week in a state-of-the-art facility in Yokohama, just south of Tokyo.
The MVD-affected dogs considered the most likely candidates for mitral valve surgery at JASMINE are in advanced Stage B2 (murmur + significant heart enlargement + severe mitral regurgitation), and Stage C (heart failure), and Stage D (heart failure resistant to medication). Thus far, over half of their patients have been in Stage C. The ages of their patients have ranged from 5 years to 15 years, with 10 years being the median age. They advise that dogs with other serious illnesses - particularly inflammatory diseases, infections, uncontrolled Cushings disease, active cancer, heart tumors, and severe pulmonary hypertension - are not good candidates for open heart surgery.
Post-operation recovery steps include total confined rest, with tubes attached to monitor the immediate healing process, post-surgery drugs such as blood thinners, and being given oxygen for up to five days. The most likely complication is an unwanted blood clot, and so the dogs are examined by echocardiogram and other monitors repeatedly during their post-surgery confinement. Most all post-operation complications will heal themselves or with the aid of drugs, in a short period of time. Japanese dogs usually are released to their referring vets earlier than those from overseas. Once the dogs return home, they need to be kept confined for a month or so and quiet and not particularly active at least three months. None of these post-op dogs are good candidates for very active lifestyles, such as competing in agility trials.
JASMINE's successful surgeries are measured over a series of time frames - (a) as of the date of discharge from the hospital, (b) three months, and (c) one year:
(a) As of discharge, they report that their 2021 results were that 97.5% of their patients survived the surgeries. The recovering dogs' most vulnerable time has been the first two days following the surgeries. Of all patients which died prior to discharge, 70% of them passed away during those first two days.
(b) As of three months following discharge, 97% continued to survive.
(c) As of a year after discharge, 91.4% were alive.
They have found that the stage of the dogs' MVD (B2, C, or D) has not been determinative of post-operation survivability. The dogs at greatest risk following surgery have been those with other serious disorders, including pulmonary hypertension due to non-MVD causes (e.g., lung disease, heartworm damage, tricuspid valve regurgitation), chronic kidney disease, recent pancreatitis, Cushing's disease, hypothyroidism, seizures, certain arrhythmias, and previous blood transfusions.
The heart health of the surgically-repaired dogs may be expected to vary
widely. While the goal of the repair is to enable the mitral valve to open
and close as it was designed, with no leakage back through the valve from
the left ventricle to the left atrium, in some dogs this mitral
regurgitation (MR) will continue and possibly even
 severely. But for most
all recovered dogs, their left atriums and left ventricles have reduced in
size significantly, and they no longer have required medication with
pimobendan or diuretics. Nevertheless, the disease may continue to progress,
and ultimately may reach the stage of heart failure again. Interestingly,
the most vulnerable category of post-surgery patients to continued MVD are
the younger ones, because over time their MVD is more likely to have the
time to re-activate and progress back to heart enlargement and heart
failure. For most of the older dogs, they are more likely to die of
non-cardiac causes.
severely. But for most
all recovered dogs, their left atriums and left ventricles have reduced in
size significantly, and they no longer have required medication with
pimobendan or diuretics. Nevertheless, the disease may continue to progress,
and ultimately may reach the stage of heart failure again. Interestingly,
the most vulnerable category of post-surgery patients to continued MVD are
the younger ones, because over time their MVD is more likely to have the
time to re-activate and progress back to heart enlargement and heart
failure. For most of the older dogs, they are more likely to die of
non-cardiac causes.
Contact JASMINE on-line here. For additional information and assistance in communication with JASMINE and support traveling to Japan for MVR surgery, contact Mighty Hearts Project here.
RETURN TO TOP
June 29, 2022:
Why are cardiologists obsessed with predicting
when MVD-affected
cavaliers will die?
 Time
and again we receive reports from cavalier owners that their dogs'
cardiologists tell them when they may expect their pets to die of mitral
valve disease (MVD). It is as if these board certified 'healers' are
passively-aggressively obsessed with predicting the deaths of their
patients, like they may even get a perverted thrill out of depressing the
people who pay their bills.
Time
and again we receive reports from cavalier owners that their dogs'
cardiologists tell them when they may expect their pets to die of mitral
valve disease (MVD). It is as if these board certified 'healers' are
passively-aggressively obsessed with predicting the deaths of their
patients, like they may even get a perverted thrill out of depressing the
people who pay their bills.
The fact is that no veterinarian knows when most any MVD-affected dog will die, unless that dog presently is in his clinic's oxygen cage on an IV of diuretic and cannot breathe on its own. Nevertheless, we often hear reports of ominous statements from them, such as, "Your dog is in heart failure and has only x months to live." Usually, that 'x' is three, six, or nine months - rarely even a year. We personally witnessed a cardiologist recommending to a cavalier owner that her dog be euthanized during that visit to his clinic because the dog probably would not survive the trip back to their home. Wrong again, Grim Reaper!
If perversity is not their motive, what is? What objective value can there be in telling owners when to expect their dogs to die? What difference should it make in how the dogs are to be medicated and cared for after leaving the cardiologist's office? The usual consequence is that the owners become terribly depressed, and these hopeless souls likely pass that same message telepathically but unintentionally on to their dogs. Some may even decide further medical care for their star-crossed dogs would be useless, a waste of time and money.
Are these seers just trying to show off? Have they forgotten that their patients' owners look to them as 'the specialists' who know much, much more than the owners do about MVD, and therefore to the owners, these 'experts' are viewed as absolutely accurate in predicting time of death as well as they are in diagnosing the stage of the disease?
These cardiologists do not know how much longer their MVD patients will live. They may have read veterinary journal articles in which the deaths of the dogs in the studies were ranged from the earliest to the latest, with the mean or average date in between. But that information applied only to the dogs in those studies, not to the dog now on the examining table with its owner seated on the other side of that table.
RETURN TO TOP
February 22, 2022:
Veterinarians' seat-of-the-pants diagnosis and treatment of mitral valve disease
Too many vets think they know what they don't know about medicating MVD
Don't let vets use your cavaliers as their laboratory guinea pigs
 Ever
since pimobendan (Vetmedin) was approved by the
U.S. government's Food & Drug Administration (FDA) in 2007 to treat dogs
in heart failure due to mitral valve disease (MVD), more and more general practice (GP)
veterinarians have been prescribing this powerful drug, with its potentially
severe adverse side effects, to dogs diagnosed with MVD but which have no
business yet being treated with it. And even worse, more recently, many GPs
have been treating MVD-affected dogs with loop diuretics, such as furosemide
(Lasix), long before they reach heart failure, with
fluid from their hearts seeping into their lungs.
Ever
since pimobendan (Vetmedin) was approved by the
U.S. government's Food & Drug Administration (FDA) in 2007 to treat dogs
in heart failure due to mitral valve disease (MVD), more and more general practice (GP)
veterinarians have been prescribing this powerful drug, with its potentially
severe adverse side effects, to dogs diagnosed with MVD but which have no
business yet being treated with it. And even worse, more recently, many GPs
have been treating MVD-affected dogs with loop diuretics, such as furosemide
(Lasix), long before they reach heart failure, with
fluid from their hearts seeping into their lungs.
Both categories of these drugs - pimobendan and loop diuretics - are the go-to medications for treating MVD, depending upon the severity and the stage of the disease. But the appropriate timing of the start of treatment is an essential factor. For example, the FDA's approval letter of pimobendan expressly limited it to treat MVD-affected dogs once they have been diagnosed with heart failure. This is known as Stage C of the list of MVD stages first published by the American College of Veterinary Internal Medicine (ACVIM) in 2009. Any prescription of pimobendan prior to heart failure, therefore, is considered "off label" by the FDA. However, in June 2022, the FDA "conditionally approved" pimobendan as treatment of dogs diagnosed with Stage B2 of MVD. This conditional approval is valid for one year with the possibility of up to four annual renewals. During that time, the drug's sponsor, Boehringer Ingelheim Animal Health USA, must demonstrate active progress toward proving the effectiveness of the drug, for full approval.
In the 2016 EPIC Study report, the investigators concluded that pimobendan may significantly delay the onset of heart failure if started when the patient's left heart chambers are significantly enlarged (Stage B2). That EPIC Study (fully financed by the patent-holder of Vetmedin) has a myriad of research defects, which essentially nullify its scientific validity. But nonetheless the ACVIM bought into it in 2019 when that group's cardiologists, in a "Consensus Statement", foolishly revised its 2009 definitions of Stage B1 and Stage B2 of MVD to incorporate earlier pimobendan treatment into them.
Some GP vets are putting MVD-affected dogs at severe risk
Far too many GP veterinarians have ignored both the FDA and the ACVIM and have been starting treatment of their MVD patients with pimobendan as soon as they first hear a mild murmur over the dogs' mitral valves. These intentionally ignorant doctors apparently do not know the difference between a mere mitral valve murmur and either heart enlargement or heart failure. And worse, they also apparently do not realize that the premature administration of pimobendan may compound the risk of life-threatening adverse reactions, including ruptured mitral valve chords and arrhythmias. (See the list below, published by the maker of Vetmedin.)
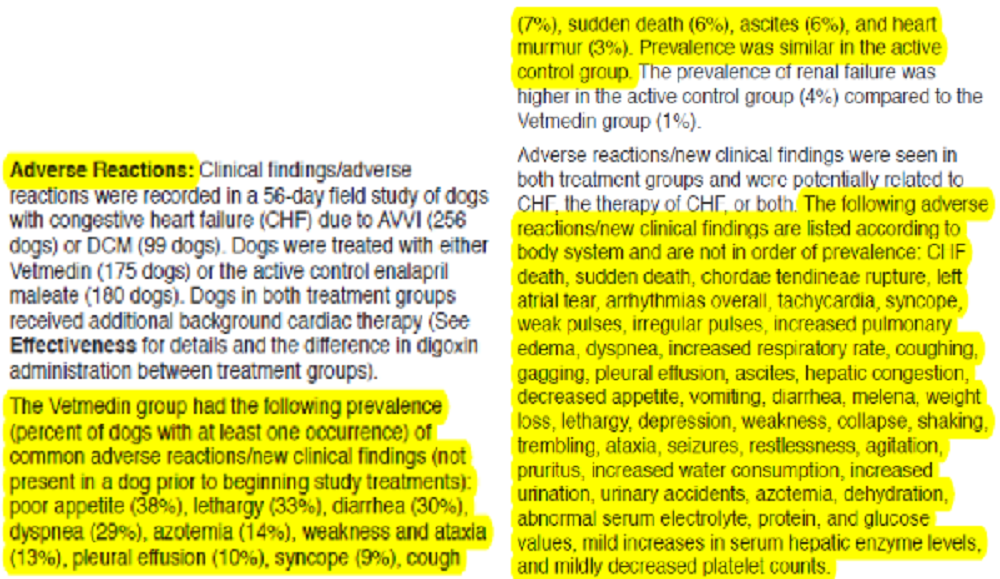
In addition, some GPs have gone so far as to treat MVD-affected dogs with loop diuretics despite not having diagnosed their patients with fluid in their lungs. In some cases, the GP veterinarians do not even bother to x-ray the dogs' hearts to see if there is any enlargement. To them, if the dog has a murmur and maybe (or maybe not) some heart enlargement, it is okay to start oral furosemide medication. These diuretics can destroy a dog's kidneys and liver, but that threat is lost on these seat-of-their-pants professionals.
70+% of MVD-affected dogs with mild enlargement
will never need any medications
Studies have found that as many as 70% or more of MVD-affected dogs with a murmur and mild heart enlargement, will not progress to heart failure, even it they remain unmedicated. That means that a vast majority of MVD-affected dogs will never need either pimobendan or a diuretic and will not die of MVD. Unfortunately, those statistics do not include cavalier King Charles spaniels, which as a breed develop MVD far earlier than the average dog and suffer the progression of MVD far more rapidly. But even including CKCSs, GP vets have no business prescribing pimobendan to dogs not yet having significant heart enlargement and prescribing diuretics to dogs not yet being in heart failure. Those who do essentially are using their MVD patients as laboratory guinea pigs.
A veterinary journal article published in February 2022 reviewed the medical records of 6,102 dogs diagnosed with MVD by GPs and which then were referred to cardiology specialists. In 88% of the cases in which the GPs not only diagnosed the MVD but also prescribed medications, the cardiologists either discontinued the medications prescribed by the GP vets or at least modified the GPs' treatments. The most troubling statistics include 191 dogs not yet in heart failure, for which GP vets prescribed a diuretic. In all but one of those cases, the cardiologists had to cancel those prescriptions. Further, in the cases of Stage C dogs - those already in heart failure and in dire need of diuretics - the GP vets prescribed them only 44% of the time, while the cardiologists rightly did so 100% of the time.
The bottom line is that GP vets should consult with cardiologists before prescribing medicines to treat MVD-affected dogs. Otherwise, in many cases the GPs are putting these dogs at grave risk by either under- or over-medicating.
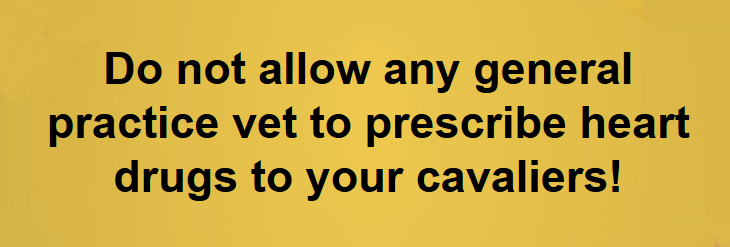
RETURN TO TOP
November 18, 2021:
Don't be fooled by Purina's hype of its new
"Pro Plan CardioCare" kibble
dog food

In January 2022, Purina intends to introduce a new dry dog food (kibble) containing a "Cardiac Nutritional Blend" of nutritional ingredients which it claims can delay the progression of mitral valve disease (MVD) and even reduce the size of enlarged hearts.
While Purina claims its new kibble is based upon "ground-breaking" research, what it really consists of is a handful of heart supplements which we have been discussing on these pages for several years. They are: Vitamin E, fish oil (for omega-3s), taurine, carnitine, magnesium, and medium-chain triglycerides (MCTs).
The "research" upon which Purina relies to back up its claims is, in short, pathetic. It is a 2019 study sponsored by Purina and conducted by Purina employees and consultants, in which ten MVD-affected dogs (nine Purina laboratory beagles and a miniature Schnauzer) were fed dry food containing the Cardiac Nutritional Blend (CNB) for six months. At the end of the study, six of the ten MVD-affected dogs being fed the CNB-laced kibble showed modest improvements in their heart measurements, while one of those dogs progressed to severe mitral regurgitation.
This 2019 research was intended to be a pilot study, and the researchers acknowledged that, "More small dogs from different breeds should be enrolled in future studies." They also disclosed that:
"Second, five [of the ten] MMVD dogs ... were on long-term medications [enalapril, pimobendan]. ... [W]e were unable to rule out potential confounding effects from medications."
Further, since they lumped all of the nutrients in a blend, they admit that:
"This study did not provide the opportunity to extrapolate effects from any single nutrient within the CPB."
Since 2019, instead of doing more research with more dogs of more breeds, and comparing the nutritional value of the individual supplements in their Cardiac Nutritional Blend, Purina decided to forego this additional research and just start selling its CardioCare kibble as if it was the be-all-to-end-all solution to keeping MVD-affected dogs from reaching heart failure.
UPDATE FEBRUARY 2022: In a February 2022 article, the lead author of Purina's 2019 study reiterated his call for more investigation. He stated: "Large studies with more dogs from different breeds should be conducted to confirm the results."
UPDATE JULY 2023: In a July 2023 article, an international team of veterinary cardiologists and nutritionists tested Purina's Pro Plan CardioCare kibble dog food on a group of 101 MVD-affected dogs, including 29 cavalier King Charles spaniels (29%), all in Stage B1, over a 365 day period to see if it met its claims that it would slow or arrest echocardiographic left heart enlargement in Stage B1 dogs. After a year of dogs being fed the Purina recipe or a control diet, the researchers reported that:
"In conclusion, a specially formulated diet was not associated with significant changes in LAD [left atrium dimension] and LVIDd [left ventricle dimension] when fed to dogs with mild subclinical DMVD for 1 year as compared to control diet. Additional studies are needed to better understand the effect of diet and the metabolome in dogs with DMVD. "
Purina and its employed researchers also fail to recognize that other studies have found evidence that a high percentage of cavalier King Charles spaniels appear to have a genetic deficiency of medium-chain acyl-coenzyme A dehydrogenase z9 (MCAD), causing epileptic seizures when fed medium chain triglycerides as their primary source of fat. Therefore, researchers are recommending that all CKCSs be genetically tested for a specific mutation of the ACADM gene which causes the MCAD deficiency, before including MCTs in their diets.
Not only is the scientific basis for this product dubious, but the other ingredients in this kibble are nothing new - the usual suspects of oats, corn, rice, and cellulose. Here is the list of main ingredients:
"Oat meal, corn gluten meal, rice, chicken meal, beef fat preserved with mixed-tocopherols, natural flavor, vegetable oil (source of medium-chain triglycerides), cassava root flour, dried beet pulp, potato protein, powdered cellulose, fish meal ..."
So, the bottom line is: Avoid this kibble! Instead, keep adding heart-healthy supplements to high-quality canned or home-made dog foods with fresh meats as the main sources of protein.
RETURN TO TOP
October 2, 2021:
Your MVD-affected cavalier is losing weight.
What to do?
It needs a protein-rich food to maintain muscle-mass
 Picture
it: Your cavalier King Charles spaniel has had
mitral valve disease (MVD) for
several years. Her (or his)
murmur grade is
high and her heart has been getting larger. She gradually has progressed to
heart failure (CHF), and
now she seems to be losing weight no matter how good her appetite has been.
She is on the full cocktail of heart pills (pimobendan, diuretic,
ACE-inhibitor, spironolactone, maybe even sildenafil).
Picture
it: Your cavalier King Charles spaniel has had
mitral valve disease (MVD) for
several years. Her (or his)
murmur grade is
high and her heart has been getting larger. She gradually has progressed to
heart failure (CHF), and
now she seems to be losing weight no matter how good her appetite has been.
She is on the full cocktail of heart pills (pimobendan, diuretic,
ACE-inhibitor, spironolactone, maybe even sildenafil).
Your dog probably has canine cachexia, severe weight loss of mostly her lean muscle mass. This is but one more symptom of MVD-affected dogs in heart failure. Over half of all dogs in CHF due to MVD will develop cardiac cachexia.
Cardiac cachexia is defined as the loss of muscle mass associated with CHF. A second definition is the rapid loss of overall weight (at least 5%) within 12 months. Researchers have found that dogs with cachexia have a significantly shorter survival time compared with dogs without cachexia. They emphasize "the importance of preventing, diagnosing, and treating muscle loss in dogs with CHF". Tufts University's veterinary school provides this chart (below) to detect muscle loss in MVD-affected dogs in CHF.
MVD-affected dogs diagnosed with cachexia should be fed any protein-rich palliative food to maintain muscle mass. It is vitally important that these dogs maintain body weight as a preventative measure.
In the ACVIM's 2019 Consensus Statement on diagnosing and treating MVD, the panel of cardiologists recommend maintaining an adequate calorie intake to minimize weight loss that often occurs in CHF. Specifically, they advise a maintenance calorie intake in Stage C of approximately 60 kcal/kg (27 calories per lb.) of body weight. They suggest warming food, mixing wet food with dry food, and offering a variety of foods, to encourage the affected dogs to eat.
Cardiologists may prescribe an appetite stimulant, such as mirtazapine (Remeron) or meclizine (Antivert, Bonine, Dramamine II, Driminate II), or capromorelin (Entyce). See more details about these drugs and other medications to offset cachexia, at this link of our MVD webpage.
RETURN TO TOP
August 27, 2021:
The cavalier King Charles spaniel is pre-disposed to ...
 Cavalier
King Charles spaniels are more likely than the average dog to develop many of
the health disorders we write about on this website. Veterinary researchers
conclude that our breed is "pre-disposed" to these diseases, and that is a major
reason for including them here. Some are considered to be "genetic" and others
just more common in the breed than in other breeds.
Cavalier
King Charles spaniels are more likely than the average dog to develop many of
the health disorders we write about on this website. Veterinary researchers
conclude that our breed is "pre-disposed" to these diseases, and that is a major
reason for including them here. Some are considered to be "genetic" and others
just more common in the breed than in other breeds.
As a handy resource, we have listed all of those common disorders here, with links to the webpages where they are discussed in some detail. We urge you all to read about them and become aware of their symptoms. You may save your dogs' lives by recognizing signs which often elude your veterinarians. One of the unfortunate facts about owning cavaliers is that many veterinarians are totally clueless about some of these serious diseases, mainly because they are either unique to our breed or darn close to it.
The cavaliers' "pre-disposed" list? Here it is:
Mitral valve disease (MVD)
Chiari-like malformation (CM)
Syringomyelia (SM)
Low blood platelets (idiopathic asymptomatic
thrombocytopenia)
Periodontal disease
Cerebellar infarcts - strokes
Anal sac disorders
Chronic pancreatitis
Brachycephalic airway obstruction syndrome (BAOS)
Curly coat syndrome
Deafness - progressive hereditary hearing loss
Intervertebral disk disease (IVDD)
Diabetes mellitus
Dry eye syndrome
Eosinophilic stomatitis
Facial nerve paralysis
Hip dysplasia (HD)
Idiopathic epilepsy
Episodic falling syndrome
Exocrine pancreatic insufficiency (EPI)
Fly catchers syndrome
Primary secretory otitis media (PSOM) - glue ear
Chronic kidney disesase
Masticatory muscle myositis (MMM)
Hydrocephalus
Muscular dystrophy
Myoclonus
Obesity
Patellar luxation
Pneumocystis pneumonia
Temporomandibular
joint dysplasia
Aortic thrombosis
Aortic thromboembolism
RETURN TO TOP
March 24, 2021:
Should MVD-Affected Dogs Start Furosemide Treatment Before Congestive Heart Failure?
One top cardiologist says 'Hell No!'
but another says 'Sometimes
Yes!'
 Cavalier King Charles spaniels diagnosed with myxomatous mitral valve
disease (MVD) uniformly have been administered a loop diuretic, usually
furosemide (brand names such as Lasix, Diuride, Frusemide, Salix), once
fluid has been detected in their lungs, due to congestive heart failure
(CHF).
Cavalier King Charles spaniels diagnosed with myxomatous mitral valve
disease (MVD) uniformly have been administered a loop diuretic, usually
furosemide (brand names such as Lasix, Diuride, Frusemide, Salix), once
fluid has been detected in their lungs, due to congestive heart failure
(CHF).
The 2009 ACVIM MVD Consensus Statement, which defined Stage C of MVD as "patients with past or current clinical signs of heart failure associated with structural heart disease", specified furosemide as the initial drug for relieving the lungs of the fluid build-up, and once the lungs have been relieved of that fluid, to continue daily doses of furosemide for the rest of the dog's life, in order to keep the fluid from re-entering the lungs. The 2019 ACVIM MVD Consensus Statement does likewise.
In neither of those ACVIM Consensus Statements is furosemide or any other diuretic mentioned for treatment of the earlier MVD stages (B1 or B2), not even by a minority of the ten authors of each of those consensus statements. In addition, for many years, board certified veterinary cardiologists have warned against prescribing diuretics to treat MVD-affected dogs prior to them reaching heart failure. For instance, Dr. Janet Olson wrote in her "'Dos and DON'Ts' for Lasix Use in Dogs" in 2016:
"It is necessary to take thoracic radiographs to confirm the presence of pulmonary edema prior to starting lasix. ... Thoracic radiographs are a must as you donʼt want to use lasix if it is not indicated. ... You donʼt want to put your patient on life long lasix if it is not (or not yet) indicated."
It is well established scientifically that diuretics can cause electrolyte losses, including sodium, potassium, calcium, magnesium, and chloride, in dogs with MVD. Low levels of these ion concentrations in the blood and heart cells can reduce the contractility of the heart and cause lethal arrhythmias and permanently damage the kidneys. These risks are inevitable when diuretics necessarily are prescribed to dogs already in heart failure, with fluid in their lungs which must be removed so that the dogs can continue to breathe.
During CHF, treating vets scramble to offset and compensate for these threats. Dogs receiving such diuretic treatment need to be be closely monitored for renal and electrolyte abnormalities. Also, the usual first line diuretic, furosemide, is known to lose its effectiveness eventually, as the dog's body tends to resist the effects of the drug (diuretic resistance).
Cardiologist #1: 'Hell No!'
Recently, a leading veterinary cardiologist who has headed the cardiology department at a major USA veterinary school (Cardiologist #1) reiterated the dangers of pre-heart failure treatment with diuretics:
"There is no evidence that furosemide should be given prior to heart failure, and there are good reasons why it shouldn't - effects on renal function, electrolytes, and stimulation of the renin-angiotensin system. I would berate my residents if they tried to do it. I have no idea why some cardiologists are recommending it."
He focuses on the truly nasty side effects which loop diuretics can have, particularly on the dog's kidneys. Why start a dog down that path, potentially destroying its kidneys, before it is absolutely necessary?
Another highly respected cardiologist and former department head at a major USA veterinary school has referred to this pre-CHF treatment as "overzealous diuresis". Nevertheless, we hear of more and more cardiologists prescribing furosemide to MVD-affected dogs diagnosed with left-sided heart enlargement (Stage B2) but not yet in heart failure (Stage C). How could that be?
This pre-heart-failure treatment with loop diuretics appears to be a relatively recent phenomenon. In a February 2022 article in which cardiologists' prescription habits for treating 4,780 MVD-affected dogs in Stage B during the years 2015 through 2018 were reviewed, in only one case out of all of those (0.02%) did a cardiologist prescribe a loop diuretic to a dog not yet in heart failure.
Using a diuretic to reduce left atrial pressure
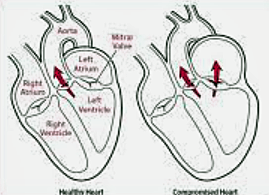 While no one is putting anything in writing and publishing it, there is a
theory floating around the cardiology community which attempts to justify
starting MVD-affected dogs at only Stage B2 on furosemide, despite the dire
warnings and the total lack of veterinary literature supporting it.
While no one is putting anything in writing and publishing it, there is a
theory floating around the cardiology community which attempts to justify
starting MVD-affected dogs at only Stage B2 on furosemide, despite the dire
warnings and the total lack of veterinary literature supporting it.
The theory may be based on some related veterinary research, that of furosemide reducing left atrial pressure (LAP) in dogs with experimentally-induced MVD. In a 2011 study by a team of Japanese veterinary cardiologists, they induced mitral regurgitation (MR) in five laboratory Beagles by surgically rupturing chordae tendineae attached to their mitral valves. Five weeks later the investigators echocardiographed the dogs and found enlarged left atriums and left ventricles in all five of them, but none of them were yet in heart failure. So, theoretically, the Beagles were in Stage B2 and not Stage C.
The Japanese team measured the dogs' LAP just prior to administering furosemide and then 30 minutes after the dosage and then for several hours thereafter for a total of 24 hours. Furosemide was delivered either intravenously (IV) or by mouth (PO) or placebo, and the dogs were rotated on a weekly basis, so that all dogs eventually were in all three groups - IV, PO, and placebo. They report finding that the dogs' maximum LAP was significantly reduced a half hour after the IV dosage of furosemide, with maximum reduction at 1 hour and 3 hours, and the significant reduction lasted 12 hours. Following the oral dosage of furosemide, they found similar results except that the maximum LAP reductions took an hour longer than the IV dosages. They report that maximum LAP returned after 24 hours following dosing. They concluded that:
"LAP was significantly reduced with furosemide in dogs with surgically induced MR. In addition, LAP was decreased in proportion to the dosage of furosemide; however, it did not significantly differ between IV and PO at the same dosage."
The cause of LAP - pressure build-up in the left atrium - is excess fluid, in this case, blood regurgitated back through the faulty mitral valve. In the Japanese study, the furosemide was used as a diuretic to reduce the volume of blood in the atrium and thereby relieve the excess pressure.
What is LAP's relationship to heart failure? Other studies have shown that abnormally high LAP due to MVD is associated with pulmonary edema (fluid in the lungs), respiratory distress, and poor prognosis. This sounds like LAP is the forerunner and perhaps the cause of eventual fluid build-up in the lungs, what we identify as congestive heart failure.
Cardiologist #2: 'Sometimes Yes!'
Some cardiologists reportedly have been prescribing diuretics to Stage B2 dogs with "cardiac coughs", in an effort to eliminate coughing caused by an enlarged left atrium pressing against either the bronchus or the trachea, by relieving the LAP and thereby reducing the size of the left atrium.
Other cardiologists even go so far as to assert that LAP alone - without any pulmonary fluid - really is the first phase of heart failure, and that congestive heart failure is a later phase. A leading investigative veterinary cardiologist who heads the cardiology department at another major USA veterinary school (Cardiologist #2) recently has opined that the onset of heart failure is not finite, and that severe enlargement of the heart, combined with rapid MVD progression, really may be the first phase of heart failure, even before fluid build-up in the lungs. He writes:
"Stage B2 is very heterogeneous and includes dogs with very mild cardiomegaly up to dogs with a level of cardiomegaly that may be heart failure. Indeed, in humans the definition of heart failure is based on the presence of clinical signs, such as exercise intolerance, while in dogs we define heart failure patients that have 'congestive heart failure', that is a step after heart failure. I personally start furosemide in patients presenting severe cardiomegaly on echo and have some echocardiographic parameters suggesting they have higher risk of fast progression."
This Cardiologist #2 acknowledges the lack of evidence-based research supporting administering furosemide prior to heart failure. He explains:
"There are no studies on furosemide on preclinical/clinical dogs, and likely we will never have one. This is not unusual, and in my opinion doesn't really matter. For example, despite not having any 'double blind clinical trial' we still use antibiotics for infection. I don't think you would like to be in the placebo arm of a study assessing the efficacy of a new antibiotic in stopping an infection. Moreover, we don't have any controlled study for treatment of heart failure with furosemide. Regardless, I would be very unhappy if my physician would not prescribe to me furosemide if I develop congestive heart failure, just because there is no study published."
Thus, calling for such advance peer-reviewed studies of pre-CHF treatment with loop diuretics would present an ethical dilemma of sorts. So, this dispute may boil down to the question of: Is it worth the risk of incurring the potentially damaging side effects, particularly to the kidneys, by medicating MVD-affected dogs with diuretics prior to the onset of any lung congestion? Two top veterinary cardiologists sharply disagree about the answer to that question. One emphatically says 'NO!' and the other says 'sometimes YES!'.
RETURN TO TOP
December 3, 2020:
Boehringer Academy spreads dangerously false information about when MVD-affected dogs should first be treated with Vetmedin.
 In a currently available free webinar series called the
"Canine
Cardiology Clinic", the maker of Vetmedin (pimobendan), Boehringer Ingelheim
Animal Health, is spreading scientifically false advice to gullible general
practice veterinarians about when to start administering Vetmedin to dogs
diagnosed with mitral valve disease.
In a currently available free webinar series called the
"Canine
Cardiology Clinic", the maker of Vetmedin (pimobendan), Boehringer Ingelheim
Animal Health, is spreading scientifically false advice to gullible general
practice veterinarians about when to start administering Vetmedin to dogs
diagnosed with mitral valve disease.
The current series of videos includes one titled "Series 2: Is this dog's heart big? Learn how to diagnose cardiomegaly using ultrasound - the LA:Ao", presented by board certified veterinary cardiologist Dr. Kieran Borgeat of Langford Vets in the UK (see below). In that video, Dr. Borgeat states while staring at his computer's camera:
"If the left atrium to aortic root ratio is 1.6 or more, your patient has cardiomegaly which requires treatment with Vetmedin."
Sheer tommyrot! This advice is contrary to all published veterinary literature of which we are aware. It contradicts the 2016 EPIC Study report's findings and conclusions, and it contradicts the unanimous advice of the ACVIM's 2019 Consensus Statement on when to treat MVD-affected dogs with Vetmedin (pimobendan).
In addition, recently published reports have found that in some breeds, healthy dogs with normal-sized hearts may have left atrium-to-aortic root ratios (LA:Ao) significantly higher than 1.6.*
There is evidence from prior veterinary research studies that premature treatment with pimobendan of dogs may accelerate the symptoms of MVD, including increased regurgitation of blood through the mitral valve, deterioration of the chordae tendineae, and enlargement of the left side of the heart. In the 2007 French study, "Comparative Adverse Cardiac Effects of Pimobendan and Benazepril Monotherapy in Dogs with Mild Degenerative Mitral Valve Disease: A Prospective, Controlled, Blinded, and Randomized Study", the researchers found (a) "increased systolic function in the PIMO group by comparison to baseline value as assessed by fractional shortening"; (b) "the maximum area and peak velocity of the regurgitant jet signal increased, whereas these variables remained stable in the BNZ group"; (c) "histologic grades of mitral valve lesions were more severe in the PIMO group than in the BNZ group"; and (d) "acute focal hemorrhages, endothelial papillary hyperplasia, and infiltration of chordae tendinae with glycosaminoglycans were observed in the mitral valves of dogs from the PIMO group but not in those of the BNZ group." They concluded:
"This study demonstrates that long-term administration of PIMO in dogs with asymptomatic MVD is associated with an increase in systolic function and, concomitantly, a progressive worsening of MVD with development of specific mitral valve lesions."
See also the 2005 study "Increased Mitral Valve Regurgitation and Myocardial Hypertrophy in Two Dogs With Long-Term Pimobendan Therapy", in which normal doses of pimobendan were determined to have increased mitral valve regurgitation and caused ventricular hypertrophy.
Any veterinarians who watch and listen to that video and believe what they are being told, should proceed at their own risk when treating MVD-affected dogs prior to heart failure.
* Mark Rishniw, et al.
Two-dimensional echocardiographic left-atrial-to-aortic ratio in healthy
adult dogs: a re-examination of reference intervals. J. Vet.
Cardiol. November 2019; doi: 10.1016/j.jvc.2019.11.001.
Lance C. Visser,
et al.
Evaluation of radiographic predictors of left heart enlargement in dogs.
2020 ACVIM Forum. J. Vet. Intern. Med. June 2020; doi: 10.1111/jvim.15903.
RETURN TO TOP
October 5, 2020:
Should arbitrary reference intervals in research studies also be used to diagnose individual MVD patients?
The unfortunate answer for MVD-affected dogs apparently is "Yes".
In recent veterinary studies of mitral valve disease (MVD or MMVD) in
cavaliers, the researchers have been categorizing dogs as either having
or not having enlarged hearts (cardiomegaly) by a set of arbitrary
reference intervals which include cut-off points between what they contend
are healthy, normal-sized hearts and MVD- affected enlarged hearts. A
prime example is the
2016 EPIC Study, in which its authors arbitrarily assumed that any
and all MVD-affected dogs necessarily had enlarged hearts only
if the echocardiographic dimensions of their left atrium and left
ventricle measurements equaled or exceeded LA:Ao = 1.6 and LVIDdN = 1.7
respectively, and if their VHS value on x-rays exceeded 10.5.
affected enlarged hearts. A
prime example is the
2016 EPIC Study, in which its authors arbitrarily assumed that any
and all MVD-affected dogs necessarily had enlarged hearts only
if the echocardiographic dimensions of their left atrium and left
ventricle measurements equaled or exceeded LA:Ao = 1.6 and LVIDdN = 1.7
respectively, and if their VHS value on x-rays exceeded 10.5.
These three parameters - the definitive tipping points between normal and enlarged hearts as far as the EPIC Study authors were concerned - had absolutely no scientific, published, peer-reviewed, veterinary literature cited to support their use. In fact, even since the EPIC Study report was issued, no such support has been published. To the contrary, before and since the EPIC Study article was published in 2016, there have been numerous empirically researched studies which have found and concluded that species-wide echocardiographic parameters for distinguishing between normal and enlarged hearts do not exist and also that the healthy dogs of several breeds can have normal-sized hearts with dimensions significantly greater than the EPIC Study cut-off points, or truly enlarged hearts with dimensions significantly smaller than those cut-off points. See this list for 34 such articles.
However, the EPIC Study authors chose to pretend that their dividing lines were absolute and inarguable between normal-sized and enlarged hearts for any dog of any breed. These arbitrary tipping points are a classic example of self-deception and circular reasoning. Interestingly, however, when the EPIC Study authors advised clinician veterinarians how to utilize the EPIC Study findings, they wrote this self-contradictory conclusion:
"The conclusions of this study are only relevant to dogs with cardiac enlargement secondary to preclinical MMVD (stage B2) as all dogs entering the study met or exceeded 3 different heart size criteria (LA/Ao > 1.6, LVIDDN > 1.7, and VHS > 10.5) and no dogs without cardiac enlargement were recruited to the study."
You see, on the one hand, they state that their findings "are only relevant to dogs with cardiac enlargement secondary to preclinical MMVD (stage B2)". On the other hand, they state that the dogs in their study "met or exceeded 3 different heart size criteria (LA/Ao > 1.6, LVIDdN > 1.7, and VHS > 10.5)". These two sets of findings are 180 degrees opposites for many dogs.
So, from the standpoint of the veterinary clinician treating cavaliers with MVD, which of the EPIC Study opposites should apply when deciding to treat with pimobendan? Should it be prescribed only if the dog has "cardiac enlargement secondary to preclinical MMVD"? Or should it be administered to any dogs which meet those three arbitrary minimum measurements, even though we know for a scientific fact that they do not define cardiac enlargement in many dogs?
It is pretty clear that since the EPIC Study's 2016 article was published, many veterinary cardiologists have chosen the arbitrary-dimensions approach and have ignored the well-established, gold-standard objective and subjective methods of determinating whether their patients really have enlarged hearts or not. (See this excerpt from a typical post-2016 echo report, below.)
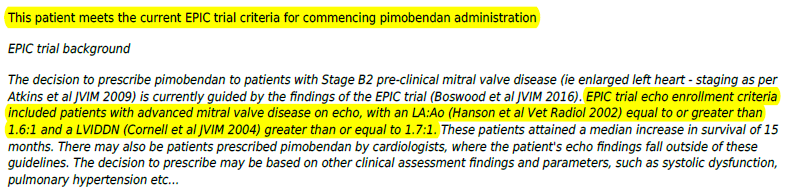
Unfortunately, the wrong answer to those questions has been codified in the 2019 ACVIM Consensus Statement. The ACVIM now has provided veterinary cardiologists with professional cover from potential malpractice by redefining its 2009 versions of Stages B1 and B2 of MVD to make the EPIC Study's two echo parameters to be the definitive cut-points between normal-sized hearts and enlarged ones. Now, nonsensically, Stage B2 dogs must have both LA/Ao > 1.6 and LVIDdN > 1.7 to be considered having enlarged hearts and thereby qualified to be treated with pimobendan, regardless of whether they really do have any cardiomegaly in either left chamber (atrium or ventricle) or not. And now, Stage B1 dogs are any that do not meet both of those cut-points and therefore are not eligible for pimobendan, even if they really do have enlarged hearts.
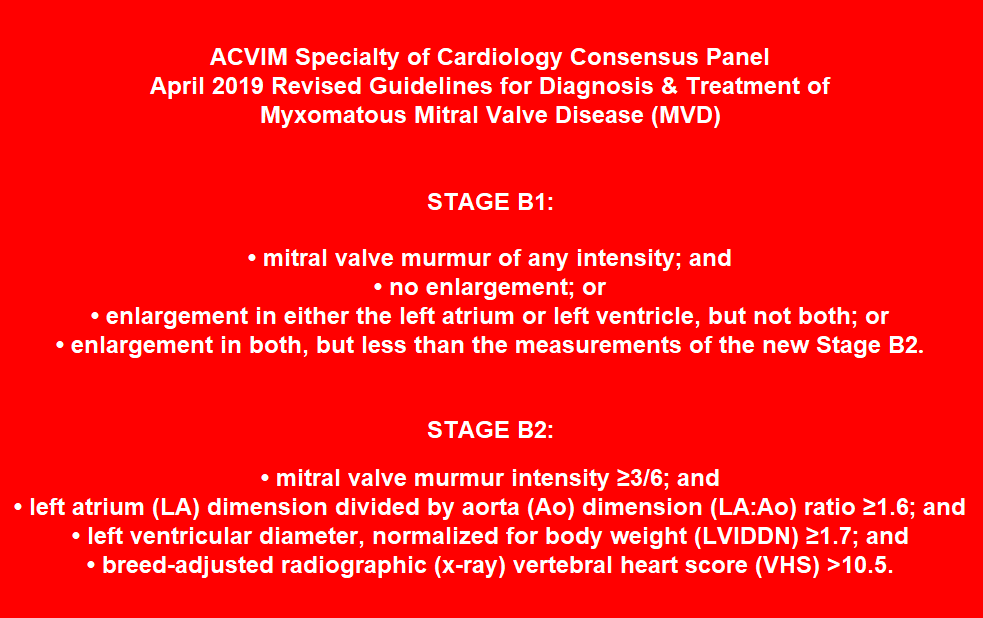
Many MVD-affected dogs have become and shall continue to be the losers. Thanks to the EPIC Study and the ACVIM's 2019 Consensus Statement, many MVD-affected dogs with enlarged hearts necessarily will be denied treatment with pimobendan, and many of them without enlarged hearts necessarily will be wrongfully treated with pimobendan.
You cardiologists know who you are; you know what you have been doing and the risks to which you have been putting your patients; and you know it is contrary to good, professional veterinary practice. You have dumbed down the practice of clinical veterinary cardiology, as a result. In that process, you have turned echocardi-ography into a computer game.
RETURN TO TOP
July 17, 2020:
Cavaliers' coats are not meant to be
cut, trimmed, or shaved
The coats (fur/hair) of cavalier King Charles spaniels are not
intended to be trimmed or cut. That rule is so
 important to the breed,
that the CKCS clubs in the UK and USA and elsewhere specifically include
"No Trimming" in their official breed standards. Conformation judges are
told to disqualify cavaliers with trimmed coats
from being judged and to ask their handlers to leave the ring. The only
allowable trimming is of hair growing between the pads on the bottoms of
the dogs' paws.
important to the breed,
that the CKCS clubs in the UK and USA and elsewhere specifically include
"No Trimming" in their official breed standards. Conformation judges are
told to disqualify cavaliers with trimmed coats
from being judged and to ask their handlers to leave the ring. The only
allowable trimming is of hair growing between the pads on the bottoms of
the dogs' paws.
The primary reason cavalier clubs have prohibited coat trimming is
because
 cavaliers have double coats of hair - a soft undercoat and a harsher
outer coat. The two coats grow independently and to different lengths. The
outer coat tends to grow slower. The undercoat is shorter and grows more
rapidly. The undercoat sheds about twice a year. In general, dogs with
double coats have sensitive skin, making them more susceptible to
irritation, inflammation, and sunburn. Their double coat protects them from
these things. Trimming the dog with a double coat can result in leaving only
the undercoat exposed to the elements.
cavaliers have double coats of hair - a soft undercoat and a harsher
outer coat. The two coats grow independently and to different lengths. The
outer coat tends to grow slower. The undercoat is shorter and grows more
rapidly. The undercoat sheds about twice a year. In general, dogs with
double coats have sensitive skin, making them more susceptible to
irritation, inflammation, and sunburn. Their double coat protects them from
these things. Trimming the dog with a double coat can result in leaving only
the undercoat exposed to the elements.
The
undercoat provides insulation in winter and cools the dog in summer. Dogs
with full double coats tend to have body surface temperatures 4 degrees lower than
those which have been trimmed or shaved because their full double coat
serves to insulate the body from higher temperatures. The thermographic
image at upper right
 shows
the temperature variations eminating from a dog who has been half shaved.
The unshaved reion's temperature is 24 degrees, while the shaved region's
temperaure is 30.8 degrees. Trimming double coated
dogs can also damage the condition of the coats, and the undercoat may never
grow back properly, leaving a sparser coat.
shows
the temperature variations eminating from a dog who has been half shaved.
The unshaved reion's temperature is 24 degrees, while the shaved region's
temperaure is 30.8 degrees. Trimming double coated
dogs can also damage the condition of the coats, and the undercoat may never
grow back properly, leaving a sparser coat.
So, if you want a cute, small dog with a nice temperament but with a short coat and no long hair on its paws, don't get a cavalier; get a Boston terrier.
RETURN TO TOP
May 12, 2020:
Why do so many ACVIM cardiologists
insist upon being Stuck On Stupid?
They fall for a Fool's Gold Standard
of heart enlargement
Dumbing-down diagnosing heart enlargement
puts our cavaliers at
high risk
 For the past
9 years (as of 2025), beginning with publication of
the EPIC Study report in September 2016, numerous ACVIM board
certified veterinary cardiologists have published articles in which they
have defined left-sided cardiomegaly (heart enlargement) for any dog of
any breed by two minimum echocardiograph measurements, one of the left
atrium (LA/Ao = 1.6) and the other of the left ventricle (LVIDDN = 1.7).
The EPIC Study authors cited no authority for their
definition, and the authors of subsequent articles simply cited the EPIC
Study as their only authority. It is a classic example of ipsedixitism.
For the past
9 years (as of 2025), beginning with publication of
the EPIC Study report in September 2016, numerous ACVIM board
certified veterinary cardiologists have published articles in which they
have defined left-sided cardiomegaly (heart enlargement) for any dog of
any breed by two minimum echocardiograph measurements, one of the left
atrium (LA/Ao = 1.6) and the other of the left ventricle (LVIDDN = 1.7).
The EPIC Study authors cited no authority for their
definition, and the authors of subsequent articles simply cited the EPIC
Study as their only authority. It is a classic example of ipsedixitism.
We have published several editorials (see below on this webpage) pointing out the obvious fallacy about the EPIC Study's baseless definition of heart enlargement in MVD-affected cavaliers and other breeds of dogs. We have noted that there is absolutely no published veterinary literature which provides any scientific support for either of these cut-off measurements on a species-wide basis. In fact, we can find no such veterinary journal publications which provide such data for any single breed of dog. To the contrary, in one of our editorials, we even have provided a detailed list of 34 (and still counting) veterinary journal articles in which their cardiologists-authors concluded that there are significant breed-specific variations in echocardiographic indices measuring left chamber dimensions, when determining whether or not an MVD-affected dog's left atrium or left ventricle is, in fact, enlarged. Significantly, one of the authors of that sham definition of enlargement in the EPIC Study even has publicly admitted -- without apology -- that they had no scientific support for their LV echo cutpoint, and that they simply made it up.
And yet, these two echo measurements for the left atrium and left ventricle have spread like a metastasizing cancer among many veterinary cardiologists, who have clambered aboard this bandwagon of a simplistic, fictitious definition of heart enlargement in MVD-affected dogs.
The Crowning Blow: ACVIM's 2019 Consensus Statement
The crowning blow - at least to date - has been
the ACVIM Consensus Statement issued in 2019, which we covered in these
two editorials ("ACVIM's
new definition of Stage B2 mitral valve disease will include dogs with
normal-sized hearts" & "ACVIM's
new definition of Stage B2 heart enlargement in MVD-affected dogs ignorantly
assumes that one size fits all").
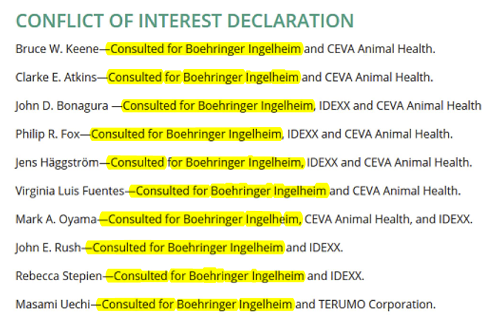 Surely,
we thought (hoped) that these ten elite ACVIM clerisy (listed at right) would admit that EPIC's definition wore no clothes,
but no such luck. Of course, since all ten of them were co-investigators in
the EPIC Study (fully funded by Vetmedin patent-holder Boehringer Ingelheim), their selection by the ACVIM to author an official ACVIM
Consensus Statement highlights ACVIM's now certain non-existent ethical
conflict-of-interest rules.
Surely,
we thought (hoped) that these ten elite ACVIM clerisy (listed at right) would admit that EPIC's definition wore no clothes,
but no such luck. Of course, since all ten of them were co-investigators in
the EPIC Study (fully funded by Vetmedin patent-holder Boehringer Ingelheim), their selection by the ACVIM to author an official ACVIM
Consensus Statement highlights ACVIM's now certain non-existent ethical
conflict-of-interest rules.
It is evident that no measurement of a heart chamber in a single echo exam can determine whether that chamber is enlarged or not. Yes, such a measurement can provide the size of the chamber - its 2-dimensional linear width at a certain instant in the heart beating cycle - but not if that chamber is larger than it had been previously. No less than two such echo exams, the earlier one serving as a baseline and a second current one, can possibly verify whether that heart chamber has increased in size since MVD was first diagnosed. But this obvious fact does not seem to bother the cardiologists authoring these scientifically baseless articles.
As a result of this flagrant incestuous connection between the EPIC Study's "investigators" (all fully funded by Vetmedin's maker) and the ACVIM's ethics-be-damned choice of consensus panelists, we have a textbook example of the long-term cancerous consequences of confirmation bias. None dare call their baby, the EPIC Study's definition of enlargement, the sham which it obviously is.
A new "Gold Standard" has emerged
 To compound this fallacious "definition" of cardiomegaly, in
a single month, we have observed that in three separate veterinary
journal articles (two in JAVMA), these single-exam echo measurements are
being labeled as "The Gold Standard" for assessing left-sided heart
enlargement in MVD-affected dogs. Here is the list:
To compound this fallacious "definition" of cardiomegaly, in
a single month, we have observed that in three separate veterinary
journal articles (two in JAVMA), these single-exam echo measurements are
being labeled as "The Gold Standard" for assessing left-sided heart
enlargement in MVD-affected dogs. Here is the list:
(1) Mostafa, A. et al. Use of cardiac sphericity index and manubrium heart scores to assess radiographic cardiac silhouettes in large-and small-breed dogs with and without cardiac disease. JAVMA. April 2020;256(8):288-896:
"Nonetheless, echocardiography remains the noninvasive gold standard for assessment of cardiomegaly in dogs." (Emphasis added.)
(2) Stepien, R.L. et al. Use of radiographic measurements to diagnose stage B2 preclinical myxomatous mitral valve disease in dogs. JAVMA. May 2020;256(10):1129-1136:
"... echocardiographic criteria (ie, LA:Ao [obtained from the right-sided short-axis view in early diastole] > 1.6 and LVIDDN > 1.7) have been used as the gold standard for identifying dogs with stage B2 MMVD." (Emphasis added.)
(3) Chhoey, S. et al. Effect of expiratory phase for radiographic detection of left heart enlargement in dogs with mitral regurgitation. Vet. Radiol. Ultrasound. May 2020;61(3):291-301:
"... echocardiographic LA/Ao > 1.5 used as the gold standard for LA enlargement." (Emphasis added.)
From where did this "Gold Standard" nonsense come? As recently as 2021, board certified veterinary cardiologists John Bonagura and Virginia Luis Fuentes wrote in their chapter "Echocardiography", in Small Animal Diagnostic Ultrasound (Fourth Edition, 2021):
"Although ventricular and atrial volumes can be estimated by M-mode and 2D/3D echocardiographic techniques, magnetic resonance imaging (MRI) is considered the gold standard for these assessments." (Emphasis added.)
And, in October 2018, other board certified veterinary cardiologists were acknowledging the non-existence of any such Gold Standard. See, Strohm, L.E. et al. Two-dimensional, long-axis echocardiographic ratios for assessment of left atrial and ventricular size in dogs. J. Vet. Cardiol. October 2018;20(5):330-342:
"Importantly, the relative merits of this method of left heart measurement cannot be truly compared with other approaches considering the lack of a gold standard for left heart size." (Emphasis added.)
Previously, in a 2014 study (Wesselowski S, et al. Discrepancies in identification of left atrial enlargement using left atrial volume versus left atrial-to-aortic root ratio in dogs. J Vet Intern Med 2014;28:1527e33), those authors expressly stated that the LA/Ao ratio was not the gold standard. They described the gold standard for measuring left atrial size as: "gold standard diagnostic imaging such as MSCT [multi-slice computed tomography] or CMR [cardiac magnetic resonance imaging]".
Also, in a September 2016 article (Franco, R.P. Determination of left atrial volume in healthy dogs and dogs with myxomatous mitral valve disease. Pesquisa Vet. Brasileira. September 2016;36(8):743-748), the authors discounted the accuracy of the LA/Ao measurement of LA size, stating:
"In this study, the obtained results were not compared with the standard values from the tests considered to be 'gold standard' for LA volume measurement, such as MRI and CT. These comparisons would indicate real LAV values and differences from volumes obtained by 2D echocardiography."
Further to the contrary, consider: Buchanan, J.W., et al. Vertebral scale system to measure canine heart size in radiographs. JAVMA. January 1995;206(2):194-199. This was the seminal piece of veterinary literature introducing the vertebral heart score (VHS) to measure heart enlargement in dogs. In that article, Professor Buchanan demonstrated that not only is the VHS method intended to be used to compare sets of x-rays "over time in a given dog" to monitor the progression of heart enlargement, but that the VHS method is superior to periodic echocardiographic measurements as cardiomegaly progresses, because each VHS consists of two measurements while echo exams measure only a single dimension. Specifically, Dr. Buchanan stated:
"ln addition to initial assessment of heart size, the VHS method also is useful in monitoring the progression of heart enlargement over time in individuals. Recording the heart size in vertebral scale encourages objectivity and is a convenient way of recording changes in heart size in response to treatment or progression of cardiomegaly. The examples of radiographic and echocardiographic measurements in a dog with progressive cardiomegaly reveal that absolute M-mode echocardlographic measurements did not reflect the extent of the heart size increase as well as the VHS method over the final 2.5-year period. This is because the echocardiographic measurements represent only a single dimension (mainly short axis), whereas the VHS method reflects change in 2 dimensions.
"The major uses of the VHS method are in helping determine whether cardiomegaly exists in dogs with minimal radiographic changes and quantificatlon of the progression of cardiomegaly over time in a glven dog."
This verifies that both methods - VHS and echo - must entail at least two exams - a baseline and another at later date, to possibly detect cardiomegaly. So, how did this nonsense about a single echo "Gold Standard" even come to pass? The obvious fact is that the only Gold Standard for determining if any MVD-affected dog's heart has become enlarged is to compare at least two - a baseline echo or x-ray with a current echo or x-ray. Anything less than that is simply fool's gold.
The dumbing-down of diagnosing MVD in our cavaliers
The bottom line here is that far too many board certified veterinary cardiologists are dumbing down their profession by re-defining cardiomegaly to be a couple of meaningless echocardiographic measurements during a single echo examination. They essentially have been using a Fool's Gold Standard and inexplicably insist upon being Stuck On Stupid.
The result for their patients - our cavalier King Charles spaniels and
other breeds with MVD - is that they can
 end up being mis-diagnosed and
therefore mis-treated. If a dog which does not have an enlarged heart is
assumed to have one, because of a false-positive due to this nonsensical
definition of enlargement, then the dog likely will be prescribed pimobendan
unnecessarily before it's time, a potentially very dangerous
mistake. And, conversely, a dog which does have an enlarged heart
could be assumed not to have one - a false negative - and be denied
pimobendan when that drug could save the dog's life.
end up being mis-diagnosed and
therefore mis-treated. If a dog which does not have an enlarged heart is
assumed to have one, because of a false-positive due to this nonsensical
definition of enlargement, then the dog likely will be prescribed pimobendan
unnecessarily before it's time, a potentially very dangerous
mistake. And, conversely, a dog which does have an enlarged heart
could be assumed not to have one - a false negative - and be denied
pimobendan when that drug could save the dog's life.
It is one thing for the echocardiograph to be the cardologist's favorite device. It is a far more dangerous thing for that cardiologist to become so addicted to that device that he thinks it is the answer to diagnosing every MVD-affected dog's clinical condition.
RETURN TO TOP
October 7, 2019:
Cardiologist Dr. Sonya Gordon recommended a VHS value of >10.5 as a heart enlargement definition but then rejects a higher VHS value of 11.5
Go figure!
Does she not see the fallacy of her reasoning?
 At the April 3, 2019 meeting of the UK
BSAVA's Veterinary Cardiovascular
Society, board certified veterinary cardiologist Dr. Sonya Gordon led a
discussion titled
"Can VHS predict EPIC echo inclusion criteria?" In
that title, "VHS" refers to the Vertebral Heart Score (VHS) formula for
measuring the size of a dog's heart as compared to the length of the
dog's spinal column. Also, in that title, "EPIC" refers to the 2016 EPIC
Study report in which Dr. Gordon and two other cardiologists led a team
of 33 other cardiologists in an effort to determine if pimobendan
(Vetmedin) could delay the onset of congestive heart failure in dogs
having enlarged hearts due to mitral valve disease (MVD).
At the April 3, 2019 meeting of the UK
BSAVA's Veterinary Cardiovascular
Society, board certified veterinary cardiologist Dr. Sonya Gordon led a
discussion titled
"Can VHS predict EPIC echo inclusion criteria?" In
that title, "VHS" refers to the Vertebral Heart Score (VHS) formula for
measuring the size of a dog's heart as compared to the length of the
dog's spinal column. Also, in that title, "EPIC" refers to the 2016 EPIC
Study report in which Dr. Gordon and two other cardiologists led a team
of 33 other cardiologists in an effort to determine if pimobendan
(Vetmedin) could delay the onset of congestive heart failure in dogs
having enlarged hearts due to mitral valve disease (MVD).
The published abstract of Dr. Gordon's April 2019 presentation does not fully disclose what she said at the UK Veterinary Cardiovascular Society's meeting or what questions she may have been asked by the UK cardiologists in attendance. But that abstract does highlight an obvious absurdity in her topic. As she states in the abstract:
"The EPIC Trial had three cardiac size inclusion criteria, two echocardiographic (LVIDDN > 1.7 and LA:Ao ratio [2D Swedish] > 1.6) and one radiographic (VHS > 10.5)." (Emphais added.)
Thus, she admits that for the EPIC Study, the VHS definition of an enlarged heart is any VHS score above a value of 10.5. But then, she immediately goes on to criticize cardiologists* who would dare to rely upon a higher VHS value of 11.5 as defining heart enlargement. She states:
"Several reports and publications have suggested a VHS > 11.5 may be predictive of EPIC echocardiographic inclusion criteria (now ACVIM Stage B2) in dogs with MMVD, however this cutoff is based on small sample sizes, or was made based on inferences from other publications." (Emphasis added.)
Thus, she states an impossible conundrum: If defining heart enlargement using a cutoff VHS value of 11.5 "is based on small sample sizes, or was made based on inferences from other publications", then why was not the significantly lower VHS value of >10.5, which she used in her EPIC Study, even less reliable?
Dr. Gordon does not answer that question in her presentation abstract, and frankly we doubt she answered it (or was even asked) during her oral discussion with the UK cardiologists. But in her abstract, she conveniently, if unintentionally, points out the insanity that underlies the EPIC Study and its findings and conclusions. You see, in the EPIC Study, the investigators assumed (without any scientific evidence at all to back themselves up) that a VHS score of >10.5 (along with the two equally bogus echocardiographic measurements) was the unquestionable gold standard for defining an enlarged heart in any MVD-affected dog of any breed. (Breed-specific measurements be damned!)
At some point, the EPIC Study investigators are going to have to come to terms with reality, but that certainly did not appear to have happened at this past April's meeting of UK Veterinary Cardiovascular Society. In the meantime, MVD-affected dogs surely are continuing to be mis-diagnosed as either having enlarged hearts when they do not (and being improperly treated with pimobendan) or not having enlarged hearts when they do (and not being prescribed pimobendan when they should be).
Since all 36 of the EPIC Study investigators have confessed in a conflict-of-interest statement (see below) to having been majorly financially compensated by the sole manufacturer of pimobendan (Vetmedin), we doubt any of them will break ranks and speak truth-to-power anytime soon.
* To compound this absurdity, Dr. Gordon is one of seven ACVIM board certified cardiologists who are members of the Caridac Education Group (CEG), which on their website expressly recommend: "Pimobendan treatment should be initiated in dogs with ... a VHS > 11.5."
RETURN TO TOP
July 30, 2019:
CavalierHealth.org's first aid kit
for our traveling cavaliers
 Whenever we travel with our cavaliers, we also bring two first aid kits,
one for us and the other for our dogs. Over many years, we have added to our
list of dog first aid kit contents.
Whenever we travel with our cavaliers, we also bring two first aid kits,
one for us and the other for our dogs. Over many years, we have added to our
list of dog first aid kit contents.
We have found that bandaids and antiseptics may not be enough to treat what health problems our dogs can get into. Torn paw pads, eye injuries, burns, bee stings, snake bites, broken bones are a few of the less common things that can happen to a dog away from home.
Here is our current list (with the brand names in parentheses) and a brief explanation of their uses:
CANINE FIRST AID KIT CONTENTS
Water -- to clean skin and wounds
Povidone-iodine (iodopovidone) pads (Dynarex) -- to clean wounds
Triple antibiotic ointment packets (Safetec) -- to treat open wounds
Eye irrigating solution (Bausch+Lomb Advanced Eye Relief) -- to cleanse eyes
Sinus rinse powder packets (NeilMed Sinus Rinse) -- to clean nasal passages
Benadryl capsules and liquid -- to treat insect and snake bites
Insect bite antiseptic and pain reliever packets (Sting Relief)
Lubricating jelly packets (McKesson) -- to protect eyes from skin medications
Sterile non-stick pads
Veterinary bandages
Cotton balls and swabs
Clotting powder (Bleed Clot) -- to stop bleeding
Veterinary tissue adhesive (3M Vetbond) -- to seal lacerations
Syringes (without needles)
Paw pad moisturizer (Pura Natural Pet Paw Rescue) -- to treat torn or abrased foot pads
Veterinary thermometer (American Diagnostic Corp.)
Stethoscope
Veterinary tourniquet (Nye Tourniquet) -- for arterial bleeding
Soft shell splint (SAM Medical Products) -- for leg breaks
Rescue thermal mylar blanket
Dog carrier sling
Bach Rescue Remedy (bottle & dropper)
Exam gloves
 Truth be told, we actually have a couple of other first aid kits in our
vehicle -- one for treating severe burns and the other for gunshot wounds --
which can be used for our dogs and ourselves.
Truth be told, we actually have a couple of other first aid kits in our
vehicle -- one for treating severe burns and the other for gunshot wounds --
which can be used for our dogs and ourselves.
Several vendors offer complete kits of canine first aid supplies. We have accumulated these items separately as we have learned about their usefulness in treating our dogs for common ailments and injuries while traveling. Whole Dog Journal has its own list, linked here. If you have any suggestions or comments about what should be in a canine first aid kit, let us know by posting on our Facebook page.
RETURN TO TOP
June 25, 2019:
ACVIM's 2019 definition of Stage B2 heart enlargement in MVD-affected dogs ignorantly assumes that one size fits all
ACVIM's 2019 Stage B2 definition intentionally ignores
differences
among breeds and is scientifically bogus
It is cramming many square pegs into one round hole!
 On
April 11, 2019, the American College of Veterinary Internal Medicine's
(ACVIM) Specialty of Cardiology consensus panel (consisting of ten board
certified veterinary cardiologists) published
revised guidelines for the
diagnosis and treatment of mitral valve disease (MVD) in dogs. The
ACVIM's initial set of MVD guidelines was published in 2009 and included
the creation of the stages of MVD which have been used ever since. They
consisted of Stages A, B1, B2, C, and D. At that time, Stage B1 applied
to any MVD-affected dog which had only a mitral valve murmur and did not
also have any enlargement of the heart or symptoms of congestive heart
failure (CHF). Stage B2 in the 2009 guidelines included left-sided heart
enlargement in addition to a murmur but no CHF.
On
April 11, 2019, the American College of Veterinary Internal Medicine's
(ACVIM) Specialty of Cardiology consensus panel (consisting of ten board
certified veterinary cardiologists) published
revised guidelines for the
diagnosis and treatment of mitral valve disease (MVD) in dogs. The
ACVIM's initial set of MVD guidelines was published in 2009 and included
the creation of the stages of MVD which have been used ever since. They
consisted of Stages A, B1, B2, C, and D. At that time, Stage B1 applied
to any MVD-affected dog which had only a mitral valve murmur and did not
also have any enlargement of the heart or symptoms of congestive heart
failure (CHF). Stage B2 in the 2009 guidelines included left-sided heart
enlargement in addition to a murmur but no CHF.
These new 2019 ACVIM guidelines redefine Stages B1 and B2. From now on, according to this new Consensus Statement, any MVD-affected dog of any breed is classified as Stage B2 (meaning, has an enlarged heart) if it has:
STAGE B2
• mitral valve murmur intensity grade >3/6; and
• left atrium (LA) dimension divided by aorta (Ao) dimension (LA:Ao) ratio >1.6; and
• left ventricular diameter, normalized for body weight (LVIDDN) >1.7; and
• breed-adjusted radiographic (x-ray) vertebral heart score (VHS) >10.5.
There really is no excuse for recommending that a species-wide set of minimum echocardiographic parameters (LA:Ao > 1.6 and LVIDDN >1.7) determine whether any MVD-affected dog of any breed has, or does not have, heart enlargement. "Pseudo-science" is defined as the assertions of alleged scientific data but which are unsupported by empirical evidence. By any standard, the definition of an enlarged heart in this Consensus Statement is a textbook example of pseudo-science. Even consensus panelist Dr. Haggstrom admitted as much when he debunked this new dumbed-down concept by ironically stating in another recently published article:
"Many common echocardiographic variables are presumed to be influenced by breed, and breed-specific reference ranges are likely to be more accurate than ranges generated from dogs of all-breeds."
Giraut, S., Haggstrom, J., et al., Breed-specific reference ranges for standard echocardiographic measurements in salukis: Breed-specific reference ranges. J. Sm. Anim. Pract. 2019;60(6):374-378.

Numerous veterinary journal articles have concluded that there are significant breed-specific variations in echocardiographic indices measuring left chamber dimensions, when determining whether or not an MMVD-affected dog's left atrium or left ventricle is, in fact, enlarged. Here are over two dozen examples (with emphasis added):
(1) Morrison, S.A., et al., Effect of Breed and Body Weight on Echocardiographic Values in Four Breeds of Dogs of Differing Somatotype. J. Vet. Intern. Med. 1992;6:220-224:
"This study demonstrated that breed, in addition to weight, is an important factor in the determination of normal echocardiographic measurements for dogs."
(2) Snyder, P.S., et al., A Comparison of Echocardiographic Indices of the Nonracing, Healthy Greyhound to Reference Values from Other Breeds. Vet. Rad. & Ultra. 1995;36(5):387-392:
"Adult nonracing greyhounds were shown to have increased left ventricular cavity dimensions, systolic time intervals and wall thicknesses as compared to mongrels and various other dog breeds. ... Our finding that greyhounds have cardiac dimensions that are apparently larger than other dogs of similar weight is supported by earlier gross anatomic studies of greyhounds."
"In summary, normal nonexercised adult greyhounds have increased left ventricular cavity dimensions, systolic time intervals and left ventricular and septal wall thicknesses that differ markedly from reported normal echocardiographic values derived from mixed breed and other dogs. ... Despite correction of the data for body weight or surface area, the differences remained, suggesting that breed and body conformation may need to be considered in addition to heart rate when interpreting echocardiographic studies in the dog. Nonetheless, caution should be employed in utilizing generic reference ECHO values in the evaluation of echocardiographic studies in greyhounds."
(3) P.K. Della Torre, et al., Echocardiographic measurements in Greyhounds, Whippets and Italian Greyhounds -- dogs with a similar conformation but different size. Austr. Vet. J. 2000;78(1):49-55:
"The results from this study, taken together with previous reports, suggest Greyhounds, Whippets and Italian other breeds of comparable body size. This possibly reflects selection for athletic performance. This study adds further weight to the notion that breed variation precludes the determination of an effective reference range for echocardiographic measurements widely applicable to all purebred and crossbred dogs."
(4) O'Leary, C.A., et al., Echocardiographic parameters in 14 healthy English Bull Terriers. Austr. Vet. J 2003;81(9):535-542:
"In this study, the prediction interval for LA:Ao calculated from 2D long axis measurements in English Bull Terriers was 1.3 to 2.1."
"The dogs in this study had increased LA diameter, LV wall thickness and AoV, and decreased aortic root diameter compared with other breeds of similar body size. In addition, FS% was lower than in dogs of comparable size, and more similar to the values reported from giant breeds."
(5) Muzzi, R.A.L., et al., Echocardiographic indices in normal German shepherd dogs. J. Vet. Sci. 2006;7(2):193-198:
"Adult German shepherd dogs were shown to have larger left ventricular dimensions and wall thicknesses than other small breeds of dogs. These differences suggest that the breed and body conformation in addition to the heart rate may need to be considered when interpreting echocardiographic studies in dogs. Caution should be taken in extending these generic reference echocardiographic values to an evaluation of echo studies."
(6) Kayar, A., et al., M-Mode Echocardiographic Parameters and Indices in The Normal German Shepherd Dog. Vet. Rad. & Ultra. 2006;47(5):482-486:
"Although some normal echocardiographic values for dogs have been published, there is variation based on breeds, body size, and somatotype. Indeed, echocardiographic reference ranges derived from some dog breeds may be misleading for others."
(7) Bavegems, V., et al. Echocardiographic Reference Values in Whippets. Vet. Rad. & Ultra. 2007;48(3):230-238:
"We confirm that whippets have a larger LVD, a thicker IVS and LVW, and a lower FS than expected for dogs of comparable body weight. The clinician should be aware of these specific differences in whippets to avoid misdiagnosis of cardiac dilation, hypertrophy, and/or myocardial failure in these dogs."
(8) Voros, K., et al., M-Mode and Two-Dimensional Echocardiographic Reference Values for Three Hungarian Dog Breeds: Hungarian Vizsla, Mudi and Hungarian Greyhound. Acta Vet. Hungarica. 2009;57(2):217-227:
"Breed has been demonstrated to be an important factor, influencing intracardiac parameters in addition to body weight in dogs. Therefore, the need for normal breed-specific reference ranges has been emphasised for comparison of pathological changes caused by cardiac disorders."
(9) Jacobson, J.H., et al., An echocardiographic study of healthy Border Collies with normal reference ranges for the breed. J. Vet. Cardiol. 2013;15(1):123-130:
"There are differences in some echocardiographic parameters between healthy Border Collies and the general dog population, and the echocardiographic reference ranges provided in this study should be used as breed specific reference values for Border Collies."
"Although echocardiographic values for the general dog population have been published, it is now known that there can be variation based on breed, body size, somatotype and body surface area. Echocardiographic reference ranges derived from some dog breeds may be misleading for others, limiting their clinical usefulness."
"There are over 37 papers investigating breed specific and generic echocardiographic parameters. These studies add support to the belief that breed variation precludes the determination of a single reference range for echocardiographic measurements that may be widely applied to all purebred and crossbred dogs."
(10) M. Hollmer, et al. Left atrial volume and phasic function in clinically healthy dogs of 12 different breeds. Vet. J. September 2013; doi: 10.1016/j.tvjl.2013.05.045:
"We provided breed-specific reference ranges for 12 breeds and clinical reference ranges for use in all dogs based on BW. ... These values of LA volume might provide a better basis for assessing LA size than linear LA dimensions when examining dogs with heart disease, since small increases in linear dimensions can reflect significant increases in LA volume due to the asymmetrical nature of LA dilatation. Since body size is a major determinant of LA size, LA volume should be indexed to a measure of body size to allow meaningful comparison."
"Even when the effects of body size were taken into account, these data showed significant breed differences for LA volume. Thus, LA volume measurements in dogs of the same weight can differ slightly among breeds. It would be ideal to establish breed-specific reference values due to the differences in type of breed, size and conformation of the thorax."
(11) Gugjoo, M.B., et al., Reference values of M-mode echocardiographic parameters and indices in conscious Labrador Retriever dogs. Iranian J. Vet. Res. 2014;15(4):341-346:
"The echocardiographic indices show significant breed variations and it is important to know the normal echocardiographic values for each dog breed considering the influence of body weight on the established echocardiographic values."
(12) Misbach, C., et al. Echocardiography and conventional Doppler examination in clinically healthy adult Cavalier King Charles Spaniels: Effect of body weight, age, and gender, and establishment of reference intervals. J. Vet. Cardiol. 2014;16(2):91-100:
"Due to the large variations in size and conformation within the canine population, significant breed and body weight (BW) effects on echocardiographic variables have been demonstrated, mainly for left ventricular (LV) M-mode measurements. Body weight independent differences among breeds have also been reported. For these reasons, the breed must be considered when establishing echocardiographic RI [reference intervals] in the dog."
"In conclusion, although predictive RI assessed according to Cornell's formula seem to be acceptable for CKCS dogs, the present results suggest that establishing specific RI for echocardiographic and Doppler variables in this breed is relevant."
(13) Limm, C.K., et al., Two-dimensional left atrium-to-aorta ratios and left ventricular M-mode transthoracic echocardiographic measurements in clinically normal adult Dachshunds. AJVR 2016;77(4):374-382:
"The mean LA:Ao for the clinically normal Dachshunds of the present study was markedly different from the mean LA:Ao for clinically normal CKCSs in another study, even though the body weights for the Dachshunds (range, 5.0 to 12.6 kg) and CKCSs (5.5 to 11.9 kg) were similar. The LA:Ao as determined by the diameter method was < 1.67 for all the Dachshunds of the present study and < 1.28 for all the CKCSs of that other study."
(14) Duler, L., Interreader agreement of radiographic left atrial enlargement in dogs and comparison to echocardiographic left atrial assessment. J. Vet. Cardiol. August 2018; doi: 10.1016/j.jvc.2018.07.004:
"Our results also suggest that there are limitations to using a single linear dimension (LA:Ao) to assess LA size. The LA is a complex cardiac structure that can enlarge in multiple planes, so single measurement may not accurately reflect actual LAE. This is supported by the stronger agreement of radiographic LAE with LAV, rather than LA:Ao. Owing to the eccentric manner in which atrial enlargement occurs, large differences in overall LA size may be misrepresented by a small range of LA:Ao values. Enlargement of the LA primarily in the dorsal-ventral orientation may not be apparent in the single plane LA:Ao measurement, while enlargement in multiple directions is incorporated into the LAV value by tracing the LA border. In addition, dividing by the aortic dimension is an attempt to index LA size to a cardiac structure that theoretically does not change much in disease states. However, the size of the aorta may vary throughout the cardiac cycle [15]. While LA:Ao is less time consuming than volumetric measurements, this study and other recent veterinary studies emphasize the limitations of the LA:Ao measurement."
(15) Garncarz, M, et al., Reference intervals for transthoracic echocardiographic measurements in adult Dachshunds. Polish J. Vet. Sci. 2018;21(4):779-788:
"In recent years many breed specific echocardiographic parameters have been published for canines showing significant differences between these measurements in different dog breeds. This underlines the necessity to prepare reference values for specific breeds."
"It appears that the different size heart in the Dachshunds could simply be a characteristic of the breed, possibly resulting from a smaller body size compared to other dog breeds, a different chest conformation, or even the influence of systemic blood pressure. ... To minimize the chance of erroneously accepting an enlarged left ventricle as normal, Dachshund specific values should be used. This is especially important when classifying disease stage in Dachshunds with chronic mitral valve disease according to the most recent guidelines (Atkins et al. 2009) as this disease readily leads to chamber enlargement, including the left atrium and left ventricle."
(16) Visser, L.C., et al, Echocardiographic quantitation of left heart size and function in 122 healthy dogs: A prospective study proposing reference intervals and assessing repeatability. J. Vet. Intern. Med. 2019; doi: 10.1111/jvim.15562:
"Unlike in human medicine, recommended standards for quantitation of cardiac chamber size and function by echocardiography in dogs do not currently exist."
"Currently, no accepted standard exists on how to determine RIs [reference intervals] (ie, clinical cutoffs to help distinguish normal from abnormal) for echocardiography data sets in healthy dogs."
"Thus, common approaches for indexing linear measurement to body size have included breed-specific reference values ...".
(17) Rishniw, M., Two-dimensional echocardiographic left-atrial-to-aortic ratio in healthy adult dogs: a re-examination of reference intervals. J. Vet. Cardiol. November 2019;doi: 10.1016/j.jvc.2019.11.001:
"Twenty-eight dogs [12%] had LA:AoMAX (RPSA) >1.6, and seven dogs [3%] had LA:AoMAX (RPSA) >1.7. ... In our current study, approximately 10% of apparently healthy dogs exceeded this [LA:Ao = 1.6] limit. ... Our finding that LA:AoMAX, obtained from the right parasternal short-axis view, might exceed 1.6 in approximately 10% of dogs has clinical implications. ... We have shown that previously published upper reference limits for LA:AoMAX might be slightly low and that LA:Ao obtained at different time-points or from different views are not interchangeable."
(18) Stack, J.P., et al., Reference Intervals and Echocardiographic Findings in Leonberger Dogs. J. Vet. Cardiol. 2020; doi: 10.1016/j.jvc.2020.03.006:
"Currently, the normal echocardiographic variables of Leonbergers are unknown. Although general canine reference ranges have been published, the large number of studies evaluating breed-specific data supports the notion that the general reference ranges have limitations due to the marked phenotypic variations across canines."
(19) Gerhard Wess, et al., Echocardiographic reference intervals for volumetric measurements of the left ventricle using the Simpson's method of discs in 1331 dogs. J. Vet. Intern. Med. March 2021; doi: 10.1111/jvim.16089:
"Veterinary cardiologists face the problem of dealing with many different breeds and therefore a wide range of different body and BWs [body weights]. ... The optimal situation would be to have breed-specific RIs, generated from a large healthy population."
(20) Dutton, E., et al., Echocardiographic reference intervals in healthy UK Deerhounds and prevalence of preclinical dilated cardiomyopathy: a prospective, longitudinal study. J. Vet. Cardiol. April 2021; doi: 10.1016/j.jvc.2021.04.001:
"Healthy Deerhounds have higher LVDd, LVDs and EDVI compared with other breeds. This study provides ECHO RIs [reference intervals] for Deerhounds; sex or BW [body weight] RIs should be used when screening."
(21) Tommaso Vezzosi, et al. Reference intervals for transthoracic echocardiography in the American Staffordshire Terrier. J. Vet. Med. Sci. April 2021; doi: 10.1292/jvms.20-0622:
"Regarding echocardiographic variables, the mean LVIDDn in our AST population was significantly higher than values reported in a range of canine breeds. ... Regarding the LA/Ao, the upper reference limit in our AST population was 1.75, with 6/57 (10%) dogs with a LA/Ao >1.6. ... The LA/Ao is the most widely used echocardiographic index to evaluate left atrial dimension in dogs, and several studies have used the upper reference limit of 1.6 to define left atrial enlargement. However, our results are in line with a study demonstrating that in around 10% of dogs, in particular in Boxers and Beagles, a small aortic root is present, which leads to an increase in the LA/Ao up to an upper reference limit of 1.73."
"These breed-specific echocardiographic features should be taken into consideration for an accurate echocardiographic interpretation and screening in the AST."
(22) Patata, V., et al., Echocardiographic parameters in 50 healthy English Bulldog: Preliminary Reference Intervals. J. Vet. Cardiol. May 2021; doi: 10.1016/j.jvc.2021.04.010:
"In our sample of EB [English bulldogs], the LA:Ao ratio in the short axis plane exceeded the previous upper reference limit of <1.6 in a significant number of dogs (12%). ... Thus, the use of breed-specific echocardiographic reference intervals is ideal for appropriate structural and functional assessment. ... Additionally, breed-specific reference intervals offer the possibility to develop better echocardiographic screening programs in the EB. ... Further studies comparing indexed cardiac dimensions and geometry among canine breeds with different thoracic somatotype may be useful."
(23) Oktawia Szpinda, et al. Impact of selected individual dog traits on echocardiographic parameters obtained in 1-dimensional (M-mode) and 2-dimensional (2D) imaging. Canadian J. Vet. Res. April 2021;85(2):112-118:
"It is important to establish echocardiographic values for individual dog breeds, not only for primary measurements such as left ventricular dimension or left atrial dimension, but also for secondary measurements. ...
"Due to the wide variety of dog breeds and inhomogeneous research groups, echocardiographic measurements should be established individually for each breed based on a population study. This will allow for a more accurate interpretation of the results obtained in the echocardiographic examination and lead to earlier diagnosis of heart disease. ...
"The great variety of dog breeds means that echocardiographic findings should be individually interpreted rather than establishing reference ranges for each breed in population studies. This will allow for a more accurate interpretation of the results obtained in the echocardiographic examination and consequently lead to earlier diagnosis of changes in myocardial morphology."
(24) Murat Vurucu, et al. An echocardiographic study of breed-specific reference ranges in healthy French Bulldogs. Vet. Radiol. Unltrasound. May 2021; doi: 10.1111/vru.12997:
"Reference values obtained from breed-specific echocardiographic studies have been reported to have a significant difference compared to the general population of healthy different dog breeds. Therefore, breed-specific echocardiographic reference ranges may be more helpful in avoiding the misinterpretation of echocardiographic findings. During an evaluation without considering the breed-specific echocardiographic reference values, a normal heart structure and/or measurement could end up being falsely interpreted as either large or small or increased or decreased when compared to the general non-breed-specific reference ranges. These misinterpretations could lead to a misdiagnosis or an underdiagnosis of an underlying cardiac problem resulting in unnecessary/wrong treatment and/or no treatment."
"An echocardiographic evaluation of French Bulldogs based on general or different dog breed population reference ranges may result in misdiagnosis (such as an early phase of dilated cardiomyopathy or heart failure) because this breed has a different chest structure, cardiac silhouette, and left ventricular internal dimensions compared to other breeds. ... Normal heart sizes and shapes show substantial variation based on dog breed. Breed-specific reference ranges should be taken into consideration when evaluating the heart."
(25) Liva Vatne, et al. The effects of activity, body weight, sex and age on echocardiographic values in English setter dogs. J. Vet. Cardiol. August 2021; doi: 10.1016/j.jvc.2021.08.003:
"Our study provides transthoracic echocardiographic values for English setter dogs, showing that they have larger hearts than many other breeds and fall outside of generic reference intervals for dogs. ... Breed specific reference intervals improve echocardiographic interpretation and thereby reduce misdiagnoses. ... The study provides breed specific transthoracic echocardiographic values for English setter dogs, thereby contributing to improve diagnostic assessment of cardiac health in this breed."
(26) Mark Rishniw, Donald J. Brown. The ACVIM consensus statement definition of LV enlargement in myxomatous mitral valve disease does not always represent LV enlargement. J. Vet. Cariol. June 2022; doi: 10.1016/j.jvc.2022.06.004:
"The EPIC study employed an essentially arbitrary value of LVIDDN to dogs subsequently randomized to treatment with pimobendan or placebo and showed that dogs with LVIDDN>1.7 (and LA:Ao>1.6 and a VHS>10.5V) generally do better with the drug than without. ... The criterion for left ventricular enlargement used by the EPIC investigators for study inclusion has never been critically evaluated as indicative of left ventricular enlargement. ...
"We should note, however, that the definition of LV enlargement proposed by both the EPIC trial and, subsequently, by the ACVIM Consensus panel, is not a reference value, but a somewhat arbitrarily chosen threshold for inclusion in the EPIC trial. Therefore, clinicians adhering to these guidelines should be cautious in ascribing LVIDDN that exceed the threshold value of 1.7 as being indicative of LV enlargement. Furthermore, clinicians should note that the ACVIM Stage B2 classification requires enlargement of both the left atrium (to a LA:Ao>1.6) and enlargement of the left ventricle. How many dogs with mild left atrial enlargement, but without LV enlargement, might consequently be misclassified as having cardiomegaly remains unknown. ...
"For example, if a dog has a LVIDDN that consistently oscillates around 1.3 (within 0.1 units), an increase to 1.6 could indicate left ventricular enlargement for that dog, despite being within the population-based reference interval."
(27) Noriko Isayama, Yusuke Uchimura, Kenta Sasaki, Erika Maeda, Toshihisa Takahashi, Megumi Watanabe. Reference Values of M-mode Echocardiographic Parameter in Adult Toy Breed Dogs. Front. Vet. Sci. June 2022; doi: 10.3389/fvets.2022.918457:
"The upper limit of the prediction interval for breeds weighing <5 kg was much lower than the value currently applied. ... Taking all 86 dogs into account, when we calculated LVIDDN as measured LVIDD/BW0.294, according to the ACVIM consensus statement, the median LVIDDN value was 1.3215 and the mean value was 1.3204, the observed minimum and maximum were 0.9214 and 1.6072, respectively, while in the first and third quartiles, the values were 1.2472 and 1.4140, respectively. Notably, none of these values approached 1.7, the threshold value proposed previously, and was clinically followed by the ACVIM consensus statement. A natural corollary of this observation is that since the normal range for dogs <5 kg is <1.7, the possibility is high that by the time these toy breed dogs start receiving treatment, according to the current guidelines of diagnosis criteria of stage B2 of MMVD, they already reach a very advanced stage of the disease. Previous reports, including the EPIC study, focused mainly on dogs with BW >4 kg, and the diagnostic criteria for toy breed dogs remain mostly unexplored. Therefore, along with diagnostic criteria, we should consider starting treatment as B2 for dogs weighing <5 kg with an LVIDDN of >1.6."
(28) M. Brloznik, et al. Echocardiographic parameters in French Bulldogs, Pugs and Boston Terriers with brachycephalic obstructive airways syndrome. BMC Vet. Res. February 2023; doi: 10.1186/s12917-023-03600-9:
"The results of this study showed significant differences in echocardiographic parameters between the dogs of the three brachycephalic breeds and non-brachycephalic dogs. In addition, there were significant differences in echocardiographic parameters between dogs with and without signs of BOAS. ... We found significant differences in echocardiographic parameters between dogs of the three brachycephalic breeds and non-brachycephalic dogs, implying that breed-specific echocardiographic reference values should be used in clinical practice. In addition, significant differences were observed between brachycephalic dogs with and without signs of BOAS. The observed echocardiographic differences suggest higher right heart diastolic pressures affecting right heart function in brachycephalic dogs with and without signs of BOAS, and several of the differences are consistent with findings in OSA patients. Most of the changes of the heart morphology and function can be attributed to brachycephaly alone and not to the symptomatic stage."
(29) Oktawia Szpinda, et al., Cardiological Reference Intervals in Adult American Staffordshire Terrier Dogs. Animals. July 2023; doi: 10.3390/ani13152436:
"The echocardiographic examination performed on the AST dogs showed that this breed is characterized by a symmetrical enlargement of the cardiac silhouette compared to generally accepted RIs. AST dogs had larger LVDd, LVDs, and LA, which were similar to those measured in larger dog breeds of 30-40 kg, such as the Doberman Pincher, with a ranging BW of 26-53 kg, as well as Boxers, and German Shepherds. ... AST dogs also had smaller Ao diameters; similar sizes of the Ao were examined in Labrador Retrievers and Golden Retrievers. ...
"Due to the great variety of dog breeds subjected to echocardiography examination, RIs for echocardiographic examination for individual dog breeds have been increasingly published in the literature. The authors of these publications have indicated that creating standards for individual breeds based on specific studies of entire populations of dogs of one breed is much more accurate, because it takes into account their breed characteristics--body structure, conformation, and natural physical activity, not only BW. ...
"Our study indicates that dogs of the AST breed should be individually approached and the condition of their heart should be assessed against breed-specific RI. Such action will increase the chance to detect even minor deviations from the breed-specific RI and prevent misdiagnosis."
(30) Maria Cerbu. et al. M-Mode Echocardiography in Canine Veterinary Practice: A Comprehensive Review of Left Ventricular Measurements in 44 Different Dog Breeds. Animals. September 2023; doi: 10.3390/ani13182986:
"To ensure accurate interpretation of echocardiographic examinations in dogs, it is crucial to consider breed-specific reference values. Failing to do so can lead to misinterpretations, falsely indicating heart enlargement or altered activity when compared with general reference ranges, potentially resulting in misdiagnosis and inappropriate treatment."
(31) D. Dickson, et al. Differences in Left Ventricular Enlargement Secondary to Chronic Volume Loading Between English Springer Spaniels and Two Similar Sporting Breeds. August 2023; doi: 10.1016/j.jvc.2023.06.001:
"We found that English springer spaniels develop more pronounced left ventricular eccentric hypertrophy when exposed to chronic mitral regurgitation compared with two similarly sized athletic breeds. ... English springer spaniels have greater left ventricular dimensions when exposed to chronic mitral regurgitation, compared with Border collies and Labrador retrievers. ... English springer spaniels differ in their left ventricular morphology from two other sporting breeds, supporting previous studies that they have a unique cardiac morphotype."
(32) Valerie Chetboul, et al. Volumetric quantification identifies some left atrial dilations undetected by left atrium:aorta ratio measurements: A prospective echocardiographic study in 155 Cavalier King Charles Spaniels with and without degenerative mitral valve disease. PLoS One. March 2024; doi: 10.1371/journal.pone.0300827. eCollection 2024:
"[T]hese multibreed echocardiographic ACVIM cut-offs do not correctly fit with the CKCS breed regarding both LA and LV sizes. Therefore, in the present study, CKCS breed-specific reference intervals (instead of the ACVIM multi-breed cut-offs) were used to define LA and LV enlargement, as explained above. ... Regarding LA and LV dilation criteria, there is now scientific evidence that the proposed multibreed echocardiographic ACVIM cut-offs do not perfectly fit for several specific breeds, and the use of breed-specific reference intervals would be more appropriate. As recently demonstrated by Rishniw and Brown, approximately 10% of healthy CKCSs would be misclassified as having LV enlargement using the ACVIM-recommended scaling exponent (0.294) and the cut-off of 1.7 for normalized end-diastolic LV internal diameter. The study published by Misbach et al dedicated to the establishment of echocardiographic reference intervals in a large population of healthy CKCSs also demonstrated the discrepancy between their LV breed-specific reference intervals (assessed according to the Clinical Laboratory and Standard Institute recommendations) and the predictive reference intervals obtained in the same population using Cornell's formula. ... Regarding LA size, CKCS dogs seem to have smaller end-diastolic and end-systolic LA dimensions than most other breeds. ... Based on these data, the end-systolic LA:Ao ratio cut-off value of 1.6 proposed by the 2019 consensus ACVIM statement to detect end-systolic LA enlargement in all-breed dogs appears inappropriate (i.e., too high) for CKCSs, with a risk of missing some mild LA dilations. ... [A] sub-population [31 -- 37%] of ACVIM B1 dogs with normal LA/Ao ratios actually showed LA dilation detected by LA volume calculation, which was not apparent when applying end-diastolic and end-systolic LA:Ao ratios. ... Additionally, among the 31 CKCSs with normal end-systolic LA:Ao ratio but increased LASvol/BW volume (Fig 3), 19/31 (61%) showed increased end-diastolic LV diameter. In other words, these 19 dogs were characterized by mitral valve regurgitation severe enough to have induced both LA and LV dilation (with a median RF value of 38%). Thus, according to the 2019 ACVIM classification, these dogs may actually belong to ACVIM stage B2. ... LA volumetric quantification should the method of first choice for assessing LA size particularly to stratify ACVIM stage B dogs. Additionally, the early identification of LA enlargement in stage B dogs is of practical interest, as these dogs at risk for decompensation may benefit from a closer longitudinal follow-up than others."
(33) Paolo Savarino, et al. Left atrial volume and function in Cavalier King Charles spaniels at different ACVIM stages. Res. Vet. Sci. September 2024; doi: 10.1016/j.rvsc.2024.105428:
"Dogs in stage A had a smaller LA/Ao ratio than dogs in stage B2 or stage C/D, but not smaller than dogs in stage B1. ... Our study revealed a notable difference in the left atrial function between the ACVIM A and B1 stages. ... In conclusion, this study demonstrates that CKCS dogs with MMVD in class ACVIM B1 have increased LADn and left atrial volumes, suggesting the presence of atrial remodelling at a very early stage of the disease."
(34) Mara Bagardi, et al. Transthoracic echocardiographic reference intervals in 214 adult Golden retrievers. J. Vet. Med. Sci. February 2025; doi: 10.1292/jvms.24-0268:
"Golden retrievers in our study had larger diastolic left ventricular internal diameters (absolute and normalized to body weight) than those reported by Esser for the population of all non-sighthound dogs. Similarly, dogs in our study had higher systolic diameters normalized to body weight than those reported by Esser and Cornell for both the general canine population and all non-sighthound dogs. These differences are likely due to breed-specific cardiac morphology. This confirms the recent literature reporting that the LVIDDn is breed-dependent. The observed difference for LVIDd is in line with Esser: Golden retriever was found to be a "deviant breed" (more than 10% of the measurements of dogs of this breed were above or below the corresponding prediction interval) for this specific parameter. The existence of specific reference limits for breeds that do not conform to allometric models of the general population should reduce the misclassification of healthy dogs as having left ventricular enlargement. ... These breed-specific echocardiographic features should be taken into consideration for an accurate echocardiographic interpretation and screening every time the cardiologist must evaluate a Golden retriever."
In arriving at the arbitrary species-wide definitions of enlarged and normal hearts, this ACVIM Consensus Statement panel also has ignored the vast body of veterinary literature on scientifically establishing reference intervals and decision thresholds denoting the cutpoints between healthy and diseased dogs. See, for example, Friedrichs, K.R., et al., ASVCP reference interval guidelines: determination of de novo reference intervals in veterinary species and other related topics. Vet. Clin. Pathol. 2012;41(4):441-453:
"Interpreting clinical data using inappropriate RI [reference intervals] may lead to misclassification of results and misdiagnosis, improper treatment, or both. ... Published RI should be used with caution and only when sufficient information is available to determine their applicability. If published RI are adopted for extended use, appropriate validation procedures as described above should be performed. ...
"Unlike RI that are descriptive of a population, decision limits discriminate between populations, typically those with and without disease. ... True disease status should be established by comprehensive examination and testing procedures that may include standardized staging, grading, or scoring schemes or common outcome assessments."
Of course, neither the ACVIM Consensus Statement panel nor the rest of the EPIC Study investigators bothered at all to do any scientific research to arrive at their arbitrary reference intervals and decision limits. They simply made them up. It is a classic example of ipsedixitism -- pure conjecture.
With all of this previous research available to the 2019 ACVIM Consensus
Statement panel, and especially panelist Haggstrom's own categorical admission that
echocardiographic measurements may vary based upon breed, the
 panelists
have no excuse for what they have done. They
necessarily will be putting MVD-affected dogs at risk by either (a) causing
dogs of some breeds without any heart enlargement to be prematurely
prescribed pimobendan (i.e., intentional false-positives) or (b) causing dogs of other breeds which do have enlarged
hearts to not be prescribed pimobendan. In view of the history of widespread
reliance placed upon ACVIM consensus statements by cardiologists and general
practitioners alike, this consensus panel will have a lot to answer for in
the future.
panelists
have no excuse for what they have done. They
necessarily will be putting MVD-affected dogs at risk by either (a) causing
dogs of some breeds without any heart enlargement to be prematurely
prescribed pimobendan (i.e., intentional false-positives) or (b) causing dogs of other breeds which do have enlarged
hearts to not be prescribed pimobendan. In view of the history of widespread
reliance placed upon ACVIM consensus statements by cardiologists and general
practitioners alike, this consensus panel will have a lot to answer for in
the future.
RETURN TO TOP
April 19, 2019:
ACVIM's new definition of Stage B2
mitral valve disease will include
dogs
with normal-sized hearts
The EPIC Study report is this
ACVIM consensus panel's opium
The "B" in Stage B now stands for "Bogus"
 On April 11, 2019, the American College of Veterinary Internal
Medicine's (ACVIM) Specialty of Cardiology consensus panel (consisting
of ten board certified veterinary cardiologists) published
revised
guidelines for the diagnosis and treatment of mitral valve disease (MVD)
in dogs. The ACVIM's
initial set of MVD guidelines was published
in 2009 and
included the creation of the stages of MVD which have been used ever
since. They consisted of Stages A, B1, B2, C, and D. At that time, Stage
B1 applied to any MVD-affected dog which had only a mitral valve murmur
and did not also have any enlargement of the heart or symptoms of
congestive heart failure (CHF). Stage B2 in the 2009 guidelines included
left-sided heart enlargement in addition to a murmur but no CHF.
(See image below.)
On April 11, 2019, the American College of Veterinary Internal
Medicine's (ACVIM) Specialty of Cardiology consensus panel (consisting
of ten board certified veterinary cardiologists) published
revised
guidelines for the diagnosis and treatment of mitral valve disease (MVD)
in dogs. The ACVIM's
initial set of MVD guidelines was published
in 2009 and
included the creation of the stages of MVD which have been used ever
since. They consisted of Stages A, B1, B2, C, and D. At that time, Stage
B1 applied to any MVD-affected dog which had only a mitral valve murmur
and did not also have any enlargement of the heart or symptoms of
congestive heart failure (CHF). Stage B2 in the 2009 guidelines included
left-sided heart enlargement in addition to a murmur but no CHF.
(See image below.)
These new ACVIM 2019 guidelines redefine Stages B1 and B2. From now on, according to this new Consensus Statement, an MVD-affected dog classified as Stage B1 either has only a murmur or also has some left-sided enlargement but less than the three new minimum echocardiographic and x-ray parameters for both the left atrium and the left ventricle in the new definition of Stage B2, or the dog has any amount of enlargement in only one of those two heart chambers and not in the other.
The new Stage B1:
• mitral valve murmur of any intensity; and
• no enlargement; or
• enlargement in either the left atrium or left ventricle, but not both; or
• some enlargement in both, but less than the measurements of the new Stage B2.
For example, an MVD-affected dog with a severely enlarged left atrium but only a slightly enlarged left ventricle which measures less than the minimum left ventricle parameter of the new Stage B2, would be classified as Stage B1. Under these new guidelines, a dog in Stage B1 would not treated with any medications for MVD even though one of its two left chambers of its heart may be even severely enlarged, as long as the other left chamber is not sufficiently enlarged.
The ACVIM's 2009 version of diagnosing Stage B2 left the decision-making to the examining clinical cardiologist to determine if the dog's left atrium or left ventricle of its heart was enlarged and to what degree. Specifically, the 2009 consensus for diagnosing heart enlargement was:
"Thoracic radiography [chest x-rays] is recommended in all patients to assess the hemodynamic significance of the murmur and also to obtain baseline thoracic radiographs at a time when the patient is asymptomatic for CVHD [MVD].
"In small breed dogs with typical murmurs, echocardiography is recommended to answer specific questions regarding either cardiac chamber enlargement or the cause of the murmur if those questions are not answered adequately by auscultation and thoracic radiography.
"Echocardiography generally is indicated in larger breed dogs because the murmur of MR is more likely to be related to other causes (eg, dilated cardiomyopathy)."
In other words, the 2009 Consensus Statement recommended relying upon the size and shape of the heart on x-rays to determine whether it has enlarged, and especially compare two sets of those x-rays - one taken before enlargement and the other taken after enlargement is suspected. This is called "qualitative assessment" or "subjective analysis" by cardiologists and is the gold standard for diagnosing heart enlargement. Under the 2009 Consensus Statement, the use of echo exams was to be reserved if the examining veterinarian still had any doubts remaining after reviewing the x-rays.
The 2019 definition of Stage B2 actually specifically defines the left-sided heart enlargement in terms of arbitrary, species-wide, minimum echocardiographic measurements of the sizes of both the left atrium and left ventricle, plus a minimum overall size - the vertebral heart score (VHS) - of the heart as measured from an x-ray, and a minimum murmur loudness. No longer is the examining cardiologist expected to use his clinical knowledge, judgment, and expertise when classifying an individual MVD-affected dog as either having or not having an enlarged heart.
The new Stage B2:
• mitral valve murmur intensity >3/6; and
• left atrium (LA) dimension divided by aorta (Ao) dimension (LA:Ao) ratio >1.6; and
• left ventricular diameter, normalized for body weight (LVIDDN) >1.7; and
• breed-adjusted radiographic (x-ray) vertebral heart score (VHS) >10.5.
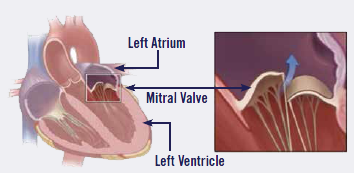 According to the
ACVIM's 2019 consensus panel, for a dog to fall into the new
Stage B2 classification and be treated with pimobendan, its heart condition must meet or exceed
all four of these parameters. No single one of them (or two or three
of them) - not even an exceptionally high LA:Ao ratio indicating severe left
atrial enlargement - qualifies the dog for Stage B2. If the dog does not meet all four parameters, then it would be
in Stage B1, and no medication is recommended.
According to the
ACVIM's 2019 consensus panel, for a dog to fall into the new
Stage B2 classification and be treated with pimobendan, its heart condition must meet or exceed
all four of these parameters. No single one of them (or two or three
of them) - not even an exceptionally high LA:Ao ratio indicating severe left
atrial enlargement - qualifies the dog for Stage B2. If the dog does not meet all four parameters, then it would be
in Stage B1, and no medication is recommended.
This totally unsubstantiated assumption (that any MVD-affected dog must have both an enlarged LA and an enlarged LV to be classified has having an enlarged heart) is directly contradicted by all previous research on this subject. For example, in this 2008 multi-breed study of 558 MVD-affected dogs which focused upon the left atrium, they reported: "However, when only cardiac-related deaths were included only the LA/Ao ratio maintained statistical significance."
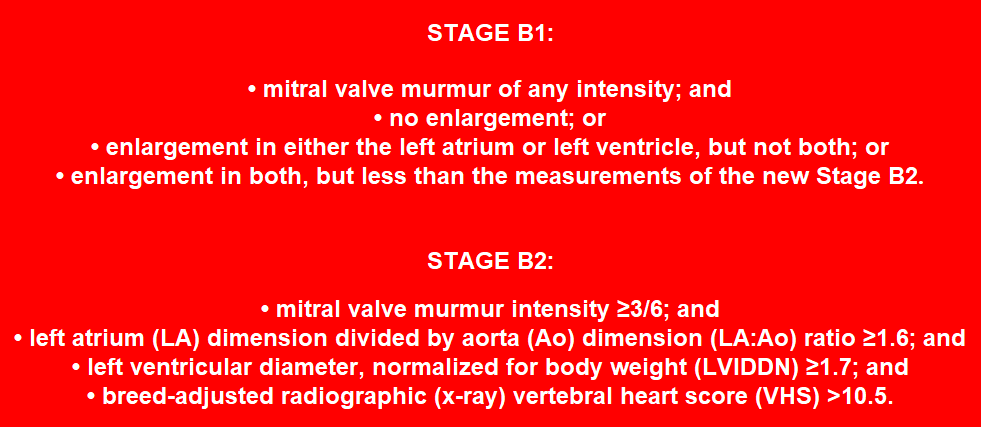
"Turning a Blind Eye" should be the subtitle for this 2019 ACVIM Consensus Statement, because its panelists either ignore or mis-state so many previously established facts about MVD and heart enlargement and even about pimobendan itself, that there can be no better explanation for what they have written.
For starters, previously published studies have shown that if pimobendan is administered prematurely, it can cause MVD to progress more rapidly in some dogs, and otherwise damage the dogs' hearts. This 2019 Consensus Statement ignores those reported risks to prescribing the drug prior to congestive heart failure.
The EPIC Study was this ACVIM consensus panel's opium
Where and how did the 2019 consensus panel come up with these LA:Ao and LVIDDN minimum dimensions? The answer is that this new definition of Stage B2 is the same as that used in the 2016 EPIC Study (which was fully financed by Boehringer Ingelheim, the manufacturer and exclusive patent holder for Vetmedin/ pimobendan), with the exception that the VHS >10.5 was not "breed-adjusted" in the EPIC Study. "Breed-adjusted" VHS in this new consensus article is defined as "cases where breed-specific VHS normal values are available", presumably in published research articles.
Oddly, while the 2019 consensus makes breed-adjustment allowances for the VHS calculations from x-rays, it strictly adheres to the EPIC Study's set of precise, species-wide minimums for the echocardiographic measurements of the two left heart chambers and the minimum grade of murmur. Consensus panelist (and EPIC Study lead investigator) Dr. Jens Haggstrom ironically debunked this new dumbed-down concept when he stated in another recently published article:
"Many common echocardiographic variables are presumed to be influenced by breed, and breed-specific reference ranges are likely to be more accurate than ranges generated from dogs of all-breeds."
Since there exist no cited published research studies of species-wide minimum measurements of enlarged left atriums and left ventricles, the next question is: How did the EPIC Study investigators arrive at these minimums, and why not rely upon the examining cardiologist's tried-and-true clinical means of determining if an MVD-affected dog's heart is enlarged or not?
Let's start with the left atrium ÷ aorta ratio (LA:Ao) of > 1.6:
As for the LA:Ao parameter, according to the footnotes in both the EPIC
Study report and the 2019 ACVIM consensus article, 1.6 was selected solely based
upon
one article, published in 2002, which studied echos of 166
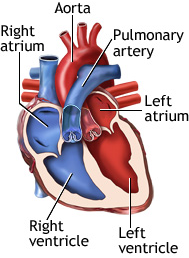 cavalier
King Charles spaniels and no other breed. According to that article, while
the dogs were divided into two categories - 56 without MVD and 110 with MVD
- the authors did not further sub-divide the MVD-affected cavaliers into
those with enlargement and those without enlargement. All we know about
those dogs is that they had mitral valve regurgitation. The purpose of the
2002 research was not to determine the breed range of LA:Ao ratios of CKCSs
with enlarged left atriums. It's sole purpose was to compare and evaluate
two different echocardiographic methods for measuring the left atrium (LA), the
aorta (Ao), and the resulting LA:Ao ratio. So, even
though this 2002 article is the only one relied upon by both the EPIC Study
and the 2019 ACVIM consensus report to justify using the minimum LA:Ao ratio
of 1.6 for all breeds, the 2002 report did not even provide a breed minimum
LA:Ao ratio for enlarged hearts in even one breed. In
fact, the reported range of LA:Ao ratios for the 110 cavaliers with MVD
varied from 0.95 to 3.17, a totally uphelpful range when trying to determine
a minimum for enlarged left atriums. Coincidentally, the mean LA:Ao was 1.61
for all of the MVD-affected dogs, regardless of whether their left atriums
were enlarged or not.
cavalier
King Charles spaniels and no other breed. According to that article, while
the dogs were divided into two categories - 56 without MVD and 110 with MVD
- the authors did not further sub-divide the MVD-affected cavaliers into
those with enlargement and those without enlargement. All we know about
those dogs is that they had mitral valve regurgitation. The purpose of the
2002 research was not to determine the breed range of LA:Ao ratios of CKCSs
with enlarged left atriums. It's sole purpose was to compare and evaluate
two different echocardiographic methods for measuring the left atrium (LA), the
aorta (Ao), and the resulting LA:Ao ratio. So, even
though this 2002 article is the only one relied upon by both the EPIC Study
and the 2019 ACVIM consensus report to justify using the minimum LA:Ao ratio
of 1.6 for all breeds, the 2002 report did not even provide a breed minimum
LA:Ao ratio for enlarged hearts in even one breed. In
fact, the reported range of LA:Ao ratios for the 110 cavaliers with MVD
varied from 0.95 to 3.17, a totally uphelpful range when trying to determine
a minimum for enlarged left atriums. Coincidentally, the mean LA:Ao was 1.61
for all of the MVD-affected dogs, regardless of whether their left atriums
were enlarged or not.
Although the EPIC and ACVIM authors failed to mention it, a the only major multi-breed study of the relationship between LA:Ao measurements and heart enlargement, which involved 558 dogs, concluded that LA:Ao > 1.7 (and not > 1.6) was a significant variable in connection with cardiac-related deaths.
Presumably, if either the EPIC Study investigators or the 2019 Consensus panel knew of any more pertinent research articles to support their species-wide LA:Ao selection of 1.6, they would have bothered to list them as citations.
An example of breed-specific scientific evidence which both the EPIC Study and ACVIM Consensus authors chose to ignore is that of the April 2016 study of the LA:Ao ratios of healthy Dachshunds, in which the LA:Ao range for normal sized hearts among as few as 40 dogs was as high as 1.66. The EPIC and ACVIM authors would arbitrarily classifiy these healthy Dachshunds as having MVD with enlarged hearts and medicate them with pimobendan for the rest of their lives. In that 2016 Dachshund article, those authors also pointed out breed differences among LA:Ao measurements, nothing that:
"The mean LA:Ao for the clinically normal Dachshunds of the present study was markedly different from the mean LA:Ao for clinically normal CKCSs in another study, even though the body weights for the Dachshunds and CKCSs were similar."
So, it appears that both the EPIC Study authors and the 2019 ACVIM consensus panel picked the minimum "all-breed" LA:Ao of 1.6 without any scientific research at all to support it and ignored the research which does exist.
Moving on, the left ventricular internal diameter in diastole,
normalized
for body weight (LVIDDN) ≥ 1.7
The LVIDDN >1.7 has an even shadier background. As noted, the EPIC Study authors and the 2019 ACVIM consensus panel have selected 1.7 as the minimum measurement to define an enlarged left ventricle, species-wide. But at the time the EPIC Study authors picked 1.7, they knew that 1.7 was in the range of normal-sized hearts for most dogs. Here is how EPIC lead investigator Dr. Adrian Boswood explained (in a recorded interview) his choice of LVIDDN = 1.7 as the minimum for all-breed left ventricle enlargement:
"Now interestingly, if you look in the literature, a normalized left ventricular diameter of 1.7 is in the normal range. The abnormal is above about 1.85, 1.9 depending upon how you read it. So, that's nudging the top of the normal range but still normal."
Yes, "interestingly", indeed, Dr. Boswood. He could have picked 1.85 or 1.9 if he really wanted to limit the EPIC Study's recruitment to dogs with actually enlarged left ventricles, but instead he picked a measurement of normal-sized ventricles and applied it to all dogs in the study.
Perhaps Dr. Boswood was referring to the normal LVIDDN range as high as 1.85 reported in this widely-cited 2004 article, in which its authors stated:
"If the result is between 1.27 and 1.85, the value is within the normal [95%] prediction interval for this study." (Emphasis added.)
EPIC lead investigator Sonya Gordon made a similar admission in a 2017 article when she and her co-authors wrote:
"In addition, all dogs with stage B2 MMVD were required to have a left ventricular internal dimension (LVID) in diastole normalized to body weight 1.7. The selected cutoff value for normalized LVID in diastole was based on a study that found higher values, although technically within the normal reported range (<1.85), predicted increased risk of death in dogs with MMVD." (Emphasis added.)
So, to Dr. Gordon, Stage B2 has nothing to do with heart enlargement.
Despite the fact that two of the EPIC Study's lead investigators admit that 1.7 is in the normal range for left ventricles, the ACVIM's 2019 consensus panel insists that it is in the enlargement range. The panel specifically and unconditionally states that LVIDDN >1.7 constitutes "cardiac remodeling".
And, finally, the VHS > 10.5:
This truly is a most interesting choice of minimum species-wide measurement for the vertebral heart scores of MVD-affected dogs with enlarged hearts. EPIC Study's lead investigator Dr. Boswood has confessed that the average VHS of cavaliers with normal-sized hearts is way above 10.5 (indeed, one researcher reports a healthy cavalier with normal-sized heart having a VHS of 11.9). And Dr. Boswood's co-lead-investigator Dr. Sonya Gordon also has confirmed that 10.5 is in the normal range. Dr. Boswood stated in that recorded interview:
"A vertebral heart score of 10.5 is in the normal range for some dogs, particularly cavaliers, actually."
Dr. Gordon also admitted in a later published article:
"There are known breed-related differences in normal VHS reference ranges with much higher normal VHS ranges reported in some breeds, including the CKCS."
So, here we have two of the three lead investigators of the EPIC Study confirming that their specified minimum enlarged heart VHS parameter of 10.5 cannot possibly be species-wide and that, for cavaliers (which made up 45.5% of all of the dogs in the entire EPIC Study), it definitely is in the normal range. Nevertheless, three years later, along comes the ACVIM consensus panel and blindly accepts EPIC Study's 10.5 as the all-breed minimum VHS for defining enlarged hearts. Of course, ACVIM's consensus panel hedges a bit since, as noted above, it suggests that the minimum VHS can be "breed-adjusted" depending upon "cases where breed specific VHS normal values are available". They even conveniently offer citations to six published articles in which the authors have reported a handful of breed-specific ranges of VHS values. Why they did not apply a "breed-adjusted" standard for the echo ranges for LA:Ao and LVIDDN is, unfortunately, unexplained.
ACVIM's panelists must know
that their Stage B2 definition is bogus
"Pseudo-science" is defined as the assertions of alleged scientific data but which are unsupported by empirical evidence. By any standard, the definition of an enlarged heart in the EPIC Study is a textbook example of pseudo-science. Surely these ten ACVIM consensus panelists must realize that their Stage B2 definition of species-wide heart enlargement is bogus. With all of their training, experience, and expertise, how could they not recognize that dogs - especially cavaliers - with normal-sized hearts necessarily will be mis-diagnosed as having enlarged hearts and will be given pimobendan for the rest of their lives? Considering that nearly half of all of the dogs recruited for the EPIC Study were cavaliers (161/354 = 45.5%), when these sham echo and x-ray minimum parameters were applied, there was a very real possibility that few or none of them had enlarged hearts at all at the start of the study, and therefore that the EPIC Study was not about dogs with enlarged hearts but just about dogs with MVD murmurs at grade 3 or above.
Now that we know the 2019 ACVIM consensus panel has just mimicked the definition of heart enlargement used in the EPIC Study, let us examine why the EPIC Study investigators chose those parameters. First of all, the goal of the EPIC Study was to recruit 360 MVD-affected dogs with enlarged hearts. Here is how Dr. Boswood described the drafting of those enlargement parameters, in his recorded interview:
"When we sat down and wrote this protocol in two thousand and nine, two thousand and ten, when we were drafting it, what we wanted to do was to insure that the dogs going into the study had big hearts, and we sat around and we said, 'How can we judge that?' And the thing that we really agreed on, the three of us as lead investigators, was a big left atrium - left atrial to aortic ratio. But we didn't want just one criterion. And the reason we didn't want just one criterion is, everyone knows you can get an inaccurate single measurement on left atrial to aortic ratio over-estimated, the dog goes on to treatment it didn't need. So what we had effectively was a belt and braces approach. The left atrial to aortic ratio is kind of the clincher, but in order to make sure that we didn't recruit unsuitable dogs, we needed their left ventricular size to be above a certain level and their vertebral heart score to be above a certain level."
To sum up Dr. Boswood's explanation, the EPIC Study investigators claim that they would have been satisfied if the only enlarged part of the study's dogs was the left atrium. The reason they did not settle upon dogs with just enlarged left atriums was because they lacked confidence that their 33 fellow participating cardiologists would perform the echo exams correctly and instead would over-estimate the size of the left atrium. So, they added the left ventricle (LVIDDN) parameter and the vertebral heart score (VHS) parameter and required that the candidate dogs meet all three of those parameters before qualifying for recruitment.
Of course, Dr. Boswood's quoted reasoning is nonsense, because if he really was concerned that his fellow research cardiologists were going to over-estimate the sizes of left atriums, why did he choose normal-sized ventricle and VHS measurements?
Now, aside from the fact that the EPIC Study lead investigators screwed up royally by (a) falsely assuming they could use minimum measurements on a species-wide basis without any scientific evidence to support such a thing, and (b) picking three minimum measurements which, for several of the breeds in the study, were of normal-sized hearts rather than enlarged ones, nonetheless their goal was commendable - to recruit only dogs with enlarged hearts. So, as Dr. Boswood put it, they used a "belt and braces approach". The belt-and-braces approach makes sense when conducting a large clinical trial. If their three echo and x-ray parameters had actually defined enlarged hearts, their study at least would have been off to a good start. But since what they did was choose a below-the-belt-and-braces approach, unfortunately, their study was off to a really bad start, and things got worse as it moved on to its conclusion.
The next mistake the EPIC Study investigators made was to conclude in their report that their initial set of four recruitment parameters were proved to be correct and should also become their recommendations to all of the clinicians who would follow in their wake. In essence, the only proof they provide is their God-like bald statement that 'it was so'. The study investigators wrote:
"The conclusions of this study are only relevant to dogs with cardiac enlargement secondary to preclinical MMVD (stage B2) as all dogs entering the study met or exceeded 3 different heart size criteria (LA/Ao > 1.6, LVIDDN > 1.7, and VHS > 10.5) and no dogs without cardiac enlargement were recruited to the study. Similarly, the conclusions are only relevant to dogs with a murmur of at least a grade 3/6 in intensity."
They failed to tailor their recommendations to the clinical setting. The most they could claim to have shown from the EPIC Study's findings was that, for the average MVD-affected dogs (with and without heart enlargement) prior to CHF, pimobendan could delay the onset of CHF longer than dogs receiving a placebo.
These conclusions make no scientific sense
for at least three reasons:
• First, as shown above, their three (echo and x-ray) parameters do not come close to defining enlargement on a species-wide basis. Dog breeds come in varying sizes, and so do their hearts. Until there is published a peer-reviewed clinical study of a scientifically-sufficient number of MVD-affected dogs with enlarged hearts in each of the 200+ recognized breeds, the EPIC Study investigators and these ACVIM consensus panelists have no legs to stand upon when it comes to claiming that any single measurement can define heart enlargement in any dog of any breed. Obviously none exists thus far because they have cited none.
• Second, if an MVD-affected dog really does have an enlarged left atrium, it should not matter that the dog's left ventricle is not yet enlarged, because typically the atrium enlarges first, ahead of the ventricle. And it should not matter that the dog's VHS value is in the normal range for that dog's breed, or that the dog's murmur grade is less than 3 out of 6. A dog can have a bulbously-enlarged left atrium and still have a normal VHS value, as this image (at right) confirms. And the dog's murmur intensity could be muted below a grade 3 due to non-cardiac reasons, depending upon the dog's chest cavity volume or the proximity and position of the heart to other organs in the cavity. Some MVD-affected breeds, such as the German Shepherd dog, commonly have no detectable murmur at all.
Now, perhaps the EPIC Study authors did not really intend that their minimum measurement for the left ventricle to actually be enlarged, or that the VHS value actually be enlarged, or that the murmur grade actually indicate enlargement. Maybe, as Dr. Boswood suggested in his interview, all they were doing was adding these below-the-belt-and-braces measurements to an assumedly enlarged left atrium to be sure that no future clinicians mistakenly classify as Stage B2 a dog with an incorrectly measured normal-sized left atrium. But that is not what they wrote in their report, and that certainly is not what the 2019 ACVIM consensus panel adopted and included in its article.
• Third, the EPIC Study trial was limited to dogs weighing between 4.1 kg (9 lbs.) and 15 kg (33 lbs.). The EPIC Study investigators produced no evidence whatsoever applicable to dogs outside of that weight range. They admitted as much when they stated (speculated, actually), "It is ... likely, although not proven, that the conclusions of this study can be extrapolated to dogs of any bodyweight with stage B2 MMVD." (Emphasis added.) They give no reason for that likelihood.
To the obvious contrary, in a 2019 study of the hearts of 5,190 dogs of various weights and sizes, using computed tomography (CT) -- mind you, a serious scientific study, unlike the unscientific assumption made by the EPIC authors and swallowed whole by the ACVIM Consensus panel -- the researchers found that both dog breed and size significantly determined heart size and volume.
So, the 2019 ACVIM Consensus panel has unthinkingly embraced these obviously defective conclusions of the EPIC Study and has rewarded them with the ACVIM's dubious seal of approval. The new Stage B2, which will determine if and when pimobendan should be prescribed to an MVD-affected dog prior to heart failure, requires (a) that the dog have at least a grade 3 murmur, and (b) that the dog have a left atrium LA:Ao ratio of at least 1.6, and (c) that the dog have a left ventricle normalized dimension LVIDDN of at least 1.7, and (d) that the dog's VHS value be over 10.5. No longer does it matter whether the dog's heart really is enlarged. All that matters from now on is if the dog's heart measurements equal or exceed all four of these arbitrary parameters.
As a consequence, clearly some MVD-affected dogs without any enlargement will be classified as Stage B2 and given pimobendan (i.e., intentional false-positives). We know from prior studies that doing so could put dogs at serious risk of acceleration of their MVD and other damage to their hearts. Clearly, also, some other MVD-affected dogs with significant left atrial enlargement will remain in Stage B1 and not prescribed pimobendan. But one thing is for sure, when our cardiologists tell us that our cavaliers are in Stage B2, we really will not know for sure whether their hearts are enlarged or not, or whether they really should be prescribed pimobendan or not.
And finally, by recommending that all MVD-affected dogs be treated with pimobendan if their heart measurements meet these arbitrary, untested, and unproven low-ball, species-wide minimums, the 2019 ACVIM consensus panel also ignores published studies which show that as many as 70% to 80% of MVD-affected dogs with mild enlargement will never progress to congestive heart failure (CHF) whether they are medicated or not. Since the purpose of starting pimobendan before CHF is to delay the onset of CHF, as many as 80% of these dogs will never need to be treated with this extremely expensive drug at all, much less for the rest of their lives.
Examples of how the new Stage B2 will mis-diagnose dogs
with or without
heart enlargement:
• Example 1: A cavalier with these measurements: Grade 3 murmur; LA:Ao = 1.6; LVIDDN = 1.7; VHS = 11.0, will be placed in Stage B2 and prescribed pimobendan even though the dog actually has a normal-sized heart.
• Example 2: A cavalier with these measurements: Grade 6 murmur; LA:Ao = 2.0; LVIDDN = 1.65; VHS = 12.0, will be placed in Stage B1 and not prescribed pimobendan even though the dog actually has a severely enlarged left atrium, a loud murmur, and an abnormally high VHS value, because despite all of those things, the dog's left ventricle measurement is below 1.7.
• Example 3: A Boston terrier with these measurements: Grade 3 murmur; LA:Ao = 1.6; LVIDDN = 1.7; VHS = 11.7, will be placed in Stage B2 and prescribed pimobendan even though the dog actually has a normal-sized heart.
• Example 4: A Dachshund with these measurements: Grade 5 murmur; LA:Ao = 1.9; LVIDDN = 1.65; VHS = 10.4, will be placed in Stage B1 and not prescribed pimobendan even though the dog actually has a severely enlarged left atrium, a loud murmur, and an abnormally high VHS value for its breed, because despite all of those things, the dog's left ventricle measurement is below 1.7.
What could the ACVIM panelists have done
to revise Stage B2?
Assuming a revision to the 2009 definition of Stage B2 is in order, the 2019 ACVIM consensus panelists would have been wise to stick to the published scientific research. For example, the 2009 Consensus Statement recommended these methods for diagnosing heart enlargement:
"Thoracic radiography [chest x-rays] is recommended in all patients to assess the hemodynamic significance of the murmur and also to obtain baseline thoracic radiographs at a time when the patient is asymptomatic for CVHD [MVD].
"In small breed dogs with typical murmurs, echocardiography is recommended to answer specific questions regarding either cardiac chamber enlargement or the cause of the murmur if those questions are not answered adequately by auscultation and thoracic radiography.
"Echocardiography generally is indicated in larger breed dogs because the murmur of MR is more likely to be related to other causes (eg, dilated cardiomyopathy)."
In essence, the 2009 Consensus Statement recommended relying upon the size and shape of the individual dog's heart on x-rays to determine whether it has enlarged, and especially compare two sets of those x-rays - one taken before enlargement and the other taken after enlargement is suspected. The use of echo exams was to be reserved if the examining veterinarian still had any doubts remaining after reviewing the x-rays.
In other words, let the examining cardiologist use his education, training, experience, and expertise, and practice his skills to determine if and how much his patient's heart is enlarged, and not follow an arbitrary, species-wide, minimum set of measurements. Typically, cardiologists classify left atrial enlargement as "mild, moderate, or severe". The 2019 Consensus Statement does not even mention these terms to describe enlargement. Instead, LA:Ao = 1.6 is all or nothing. This is not the practice of veterinary cardiology in the least. Even in other veterinary literature which speculates that LA:Ao =1.6 may suggest an enlarged atrium, that extent of enlargement is considered the minimum border-line, or very "mild".
Conflicts of financial interest or dysfunctional group-think?
Now, why would any (much less ten) experienced, board certified veterinary cardiologists sign off on such an obviously sham species-wide definition of heart enlargement as they have in this new ACVIM Consensus Statement? On the one hand, we could write it off to their admitted conflicts of financial interest. You see, all but one of them were financially compensated for participating in the EPIC Study trial (which was funded 100% by Boehringer Ingelheim, the manufacturer and exclusive patent holder for Vetmedin/pimobendan). And, in the 2019 ACVIM Consensus Statement, all ten of them also have confessed to having "consulted for Boehringer Ingelheim". If the only consequence of this revision to Stage B2 was to assure that more dogs are prescribed pimobendan, then the conflict-of-interest explanation would make sense.
But these ten authors have also imposed three totally unnecessary conditions precedent to prescribing pimobendan, which are that, in addition to the MVD-affected dog having just an enlarged left atrium, (1) it also must have an enlarged left ventricle and (2) its VHS value also must show enlargement and (3) its murmur must be at least a grade 3. So if their intent was to enable Boehringer Ingelheim to sell more Vetmedin, they have totally screwed that goal up by compounding the hurdles required to classify dogs with even severely enlarged left atriums in the new Stage B2. Their consensus smacks of dysfunctional group-think -- too many cooks stirring the same pot can reach a totally irrational decision-making outcome.
Whatever their motivations may have been, in view of their conflicts of interest with
Boehringer Ingelheim,
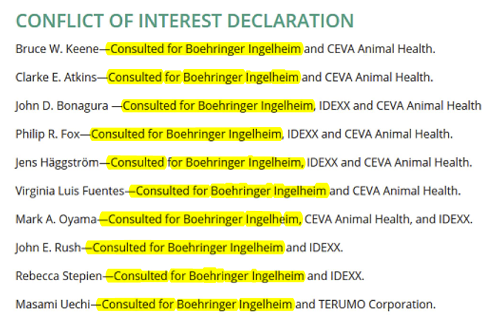 none of them should have been selected by the ACVIM
for this Consensus panel, and all of them should have declined their
selection. The ACVIM pretty much has soiled itself by knowingly choosing
a consensus panel consisting totally of authors who have been paid
consultants to the sole manufacturer of the drug which they unanimously
advocate for treating pre-CHF MVD-affected dogs.
none of them should have been selected by the ACVIM
for this Consensus panel, and all of them should have declined their
selection. The ACVIM pretty much has soiled itself by knowingly choosing
a consensus panel consisting totally of authors who have been paid
consultants to the sole manufacturer of the drug which they unanimously
advocate for treating pre-CHF MVD-affected dogs.
In 2011, the National Academy of Medicine issued a report,
"Clinical
Practice Guidelines We Can Trust", which provided recommendations for
reducing the influence of Conflicts of Interest (COI) among panels of
practice guidelines, such as this ACVIM Consensus Statement, by managing the
composition of the members of the panels. The seven recommendations (see
box at right below) included three which the ACVIM flat out has ignored in picking all ten
of these panelists: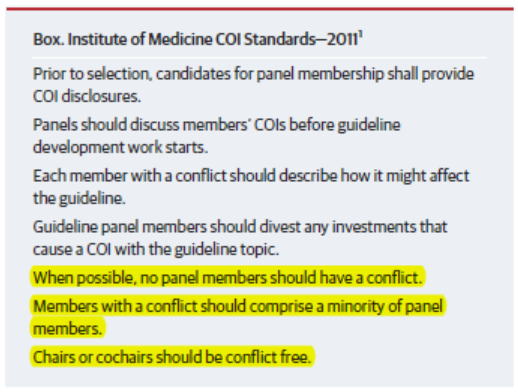
• When possible, no panel members should have a
conflict.
• Members with a conflict should comprise a
minority of panel members.
• Chairmen or
co-chairmen should be conflict free.
Now, of course, the ACVIM is a veterinary association and not a medical association, but it would be interesting to hear how the ACVIM justifies picking only panel members who have clear conflicts of interest by having direct contractual relationships with the only manufacturer of the only drug which they unanimously recommend administering to MVD-affected dogs prior to heart failure. But, alas, the ACVIM also accepts funds from this same manufacturer as a sponsor of its annual forums. So, ACVIM's conflicts of interest appear to be rooted deep within its bloodline, and its concern about them ... nonexistent. Maybe there is a difference in the ethics of the medical and veterinary societies, after all.
UPDATE: October 2023. We now have an answer from the ACVIM to how it "justifies picking only panel members who have clear conflicts of interest by having direct contractual relationships with the only manufacturer of the only drug which they unanimously recommend administering to MVD-affected dogs prior to heart failure."
On October 3, 2023, the ACVIM's editorial board published a new policy statement regarding Consensus Statement panelists and conflicts of interest. It states:
"One of the roles of the ACVIM is to identify appropriate topics and to ensure that these Consensus Statements are uniformly reliable and of high quality. To achieve this purpose, the ACVIM must ensure that topics are timely and relevant, panels are appropriately comprised of experts who are free of conflicts of interest, ...
"Guidelines should have a consistent and transparent method of development, be of uniformly high quality, and be free of bias or conflict of interest by the developers of the guidelines. ...
"It is critically important that such conflicts be identified and managed, and the Chair of the panel and the ERC [Education and Research Committee], with support from ACVIM Staff, should be charged with this responsibility. ... Those with a COI [conflict of interest] are expected to recuse themselves from (ie, abstain from) decisions where such a conflict exists. ...
"Optimally, AES [ACVIM Endorsed Statement] panels would only include members who are free of COIs relevant to the topic of the statement."
Unfortunately, that answer is four years too late for all of the MVD-affected dogs being mis-diagnosed with or without heart enlargement due to the 2019 ACVIM's Consensus Statement's dumbed-down bastardization of the definition of cardiomegaly on a species-wide basis. And, we seriously doubt that the ACVIM will do anything to correct this nonsensical 2019 Consensus Statement. So, these mis-diagnoses may be expected to continue.
From now on, the B in Stage B might as well stand for Bogus, because from now on, when a cardiologist tells you that your cavalier is in Stage B1 or B2, that really will not tell you anything accurate about your dog's heart.
RETURN TO TOP
February 2, 2019:
EPIC Study lead investigator admits
that EPIC's species-wide
"definition"
of heart enlargement is inaccurate
 In a
January 2019 veterinary journal article, EPIC Study lead investigator
Dr. Jens Haggstrom (right, center) has finally admitted that the study's
species-wide definition of heart enlargement in MVD-affected dogs is
inaccurate. Or, as he couches it, "breed-specific reference ranges are
likely to be more accurate than ranges generated from dogs of all-breeds".
In a
January 2019 veterinary journal article, EPIC Study lead investigator
Dr. Jens Haggstrom (right, center) has finally admitted that the study's
species-wide definition of heart enlargement in MVD-affected dogs is
inaccurate. Or, as he couches it, "breed-specific reference ranges are
likely to be more accurate than ranges generated from dogs of all-breeds".
The EPIC Study, which was sponsored by Vetmedin's manufacturer, Boehringer Ingelheim Vetmedica, Inc., concluded in its 2016 report that Vetmedin (generic name: pimobendan) could be prescribed to any dog, of any breed (hence, species-wide), diagnosed with mitral valve disease (MVD) if the left atrium and left ventricle of the dog's heart are enlarged, based upon two minimum echocardiogram measurements (LA/Ao >1.6; LVIDDN >1.7), and a set of x-rays showed that the dog's heart had a Vertebral Heart Sum (VHS) value >10.5. "Pseudo-science" is defined as the assertions of alleged scientific data but which are unsupported by empirical evidence. By any standard, the definition of an enlarged heart in this study is a textbook example of pseudo-science.
EPIC's enlargement parameters never were scientific
The EPIC Study included 36 board certified veterinary cardiologists from around the world and was led by three lead investigators, Drs. Adrian Boswood, Jens Haggstrom, and Sonya Gordon. These three cardiologists agreed that the species-wide definition for heart enlargement should be applied to all 360 MVD-affected dogs to be recruited for the study, and they also concluded in their report that the same definition should be applied to define heart enlargement in all dogs subsequently to be treated with pimobendan. They intentionally ignored any breed-specific heart measurements when they "defined" a canine species-wide definition of heart enlargement. Specifically, they defined heart enlargement in all dogs as:
"To be eligible for inclusion, a dog had to ... have echocardiographic evidence of left atrial and left ventricular dilatation, defined as a left atrial-to-aortic root ratio (LA/Ao) = 1.6 and body weight normalized left ventricular internal diameter in diastole (LVIDDN) = 1.7, in addition to radiographic evidence of cardiomegaly (vertebral heart sum (VHS) > 10.5)."
And, in their conclusion, they re-affirmed their minimum species-wide criteria, as follows:
"The conclusions of this study are only relevant to dogs with cardiac enlargement secondary to preclinical MMVD (stage B2) as all dogs entering the study met or exceeded 3 different heart size criteria (LA/Ao > 1.6, LVIDDN > 1.7, and VHS > 10.5) and no dogs without cardiac enlargement were recruited to the study. Similarly, the conclusions are only relevant to dogs with a murmur of at least a grade 3/6 in intensity."
The EPIC Study's conclusions were a ground-breaking advance for the administration of pimobendan, because previously the drug was not to be prescribed to MVD-affected dogs before their hearts reached congestive heart failure (CHF). One of the reasons for limiting the use of pimobendan to dogs in heart failure before the EPIC trial had been due to previous studies showing that for dogs not yet in CHF, pimobendan could accelerate the progression of MVD and also damage their hearts in other ways. (In view of that history, it is interesting that the EPIC Study investigators refused to examine in any detail the 8.4% of the pimobendan group dogs which suffered sudden, cardiac-related deaths during the study.)
Drs. Boswood and Gordon have already confessed
Despite the lead investigators' strong endorsement of these three minimum measurements for heart enlargement, soon after publication of the EPIC Study report in 2016, two of the lead investigators admitted that their definition of heart enlargement was inaccurate. Dr. Boswood contradicted two of the three minimum measurements. He said in a 2016 interview:
"A vertebral heart score of 10.5 is in the normal range for some dogs, particularly cavaliers actually."
Dr. Gordon concurred with him when she wrote in a September 2017 article:
"However, given the potential low accuracy of depending solely on a radiographic VHS greater than 10.5, ... and that there are known breed-related differences in normal VHS reference ranges with much higher normal VHS ranges reported in some breeds, including the CKCS, ... ."
It is interesting that both Drs. Boswood and Gordon singled out the cavalier King Charles spaniel (CKCS) as a dog for which their definition of heart enlargement included dogs with normal sized hearts. Note that of the 354 dogs in the EPIC Study, 161 of them (45.5%) were CKCSs. So, applying their own definition of enlargement, potentially nearly half of all dogs in the study really did not have enlarged hearts at all.
Dr. Boswood also criticized his minimum measurement of the left ventricle, stating in that same interview:
"Now interestingly, if you look in the literature, the normalized left ventricular diameter of 1.7 is in the normal range. The abnormal is above about 1.85, [1.]9, 1.9 depending upon how you read it, so that's nudging the top of the normal range but still normal."
EPIC lead investigator Sonya Gordon made a similar admission in a 2017 article when she and her co-authors wrote:
"In addition, all dogs with stage B2 MMVD were required to have a left ventricular internal dimension (LVID) in diastole normalized to body weight 1.7. The selected cutoff value for normalized LVID in diastole was based on a study that found higher values, although technically within the normal reported range (<1.85), predicted increased risk of death in dogs with MMVD." (Emphasis added.)
So, to Dr. Gordon, Stage B2 has nothing to do with heart enlargement. Nevertheless, in March 2018, Dr. Boswood reaffirmed his adherence to the EPIC Study's definition, stating in a March 2018 article sponsored by the manufacturer of Vetmedin:
"On the basis of the results of the EPIC study I now routinely recommend the use of pimobendan in dogs with preclinical MMVD and evidence of cardiac enlargement (sufficient to meet the EPIC inclusion criteria) at a dose of approximately 0.5 mg/kg/day divided into two doses (0.25 mg/kg twice a day).." (Emphasis added.)
And, since the EPIC Study report was published, this universal "definition" has been applied throughout the world to determine when to start administering pimobendan to MVD-affected dogs of any and all breeds, thereby putting thousands of dogs at potential risk of rapid progression of mitral valve disease. See, as examples, the algorithm produced by the Cardiac Education Group (at right), and this "boiler-plate" clause inserted in an echocardiogram report made by an Australian cardiologist who had just examined an MVD-affected dog, (below).
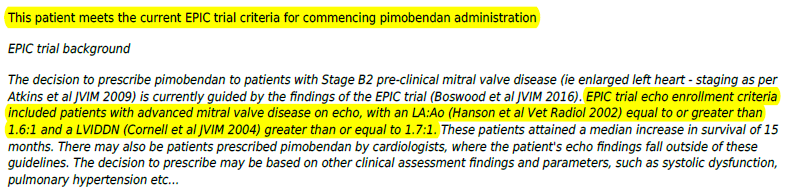
Dr. Haggstrom finally admits the obvious
Until now, the third lead investigator of the EPIC Study had remained publicly mute with respect to the accuracy of the EPIC Study's species-wide definition of heart enlargement. But in his January 2019 article in the Journal of Small Animal Practice, Dr. Haggstrom sought to establish the breed-specific range for standard echocardiographic heart measurements for Saluki dogs, based upon examining 75 healthy, purebred Salukis in 2012 and 2013. He stated:
"Well-established echocardiographic diagnostic criteria are important for the identification and early diagnosis of cardiac disease in dogs (Dukes-McEwan et al. 2003, Meurs 2010, Chetboul & Tissier 2012, Birkegård et al. 2016, Wess et al. 2017). Many common echocardiographic variables are presumed to be influenced by breed, and breed-specific reference ranges are likely to be more accurate than ranges generated from dogs of all-breeds (Bavegems et al. 2007, Wess et al. 2010, Stephenson et al. 2012, Misbach et al. 2014, Dickson et al. 2016). In salukis, a larger left ventricle (LV) might be the result of cardiac disease, such as myxomatous mitral valve disease or dilated cardiomyopathy (DCM), causing volume overload, but might also be an example of athletic heart typical for sighthounds (Page et al. 1993, Della Torre et al. 2000, Cornell et al. 2004, Bavegems et al. 2007, Seckerdieck et al. 2015)." (Emphasis added.)
Now we have the admission by Dr. Haggstrom that "breed-specific reference ranges are likely to be more accurate than ranges generated from dogs of all-breeds". Note that he cited articles as old as 12 years ago as published authorities for that obvious observation. So, why he and the other two lead investigators did not point out this vital and well-known fact in their EPIC Study report remains to be explained. Whatever their reasoning, clearly the EPIC Study report needs to be withdrawn and its definition of heart enlargement needs to be re-written before re-publication.
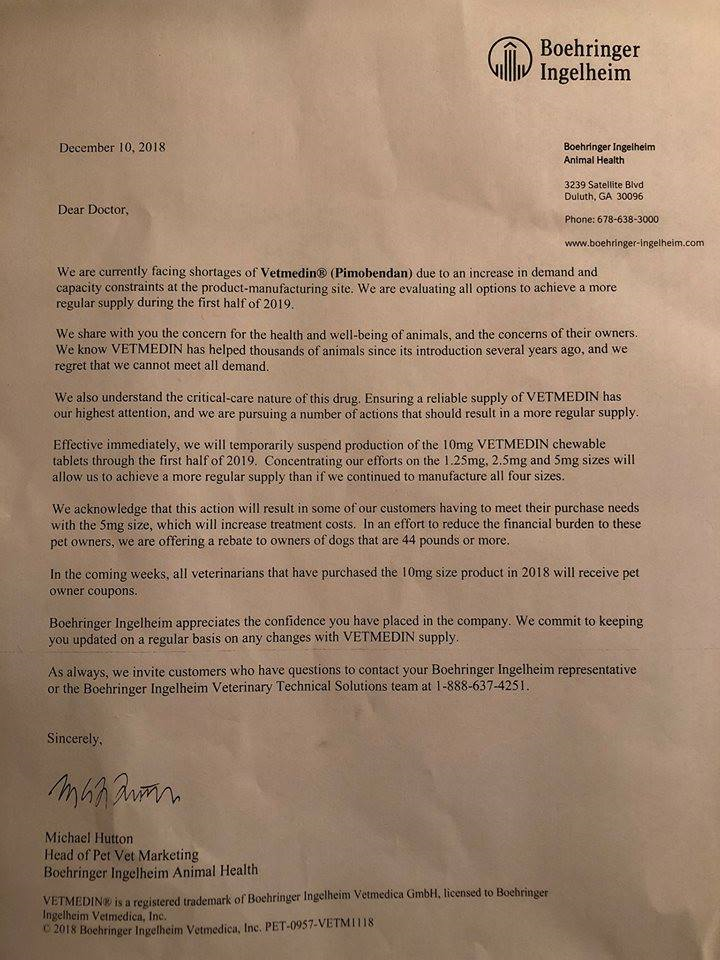 We have directly asked Dr. Haggstrom this question, which he has refused
to answer:
We have directly asked Dr. Haggstrom this question, which he has refused
to answer:
"If, as you state in the Saluki article, 'breed-specific reference ranges are likely to be more accurate than ranges generated from dogs of all-breeds', why in the EPIC Study did the investigators choose the less accurate species-wide definition with minimum measurements (VHS > 10.5 and LVIDDN > 1.7) which are known to include normal-sized hearts in CKCSs and some other breeds?"
We know that Vetmedin's manufacturer got what it was seeking all along. Beginning in late 2018, demand to fill Vetmedin prescriptions became so great that its worldwide supply ran out. MVD-affected dogs which really needed the drug could not be treated with it because no one had an inventory of it. (Click on December 10, 2018 letter at right.) And as of this writing, the manufacturer still has not caught up with this voluminous demand.
RETURN TO TOP
January 1, 2019:
What Cavalier Health news
may we expect in 2019?
 In the areas of
mitral valve disease (MVD) and
Chiari-like malformation,
2019 may bring to fruition some ground-breaking discoveries for cavalier
King Charles spaniels in the fields of diagnosis and treatment. Here are our
predictions:
In the areas of
mitral valve disease (MVD) and
Chiari-like malformation,
2019 may bring to fruition some ground-breaking discoveries for cavalier
King Charles spaniels in the fields of diagnosis and treatment. Here are our
predictions:
• Of course, open-heart mitral valve surgery is coming to the University of Florida, but at the outset at the enormous price of $40,000.00 per dog.
• Since pimobendan now is being prescribed for MVD-affected dogs with enlarged left atriums (LA), radiologists are focusing on how to objectively measure LA enlargement with x-rays alone, skipping the more expensive echocardiograms. Two recent publications have devised objective methods of measuring LA size from x-rays. Comparing an old and current pair of x-rays, using these measurement formulas, would be far more accurate than following the corrupt, species-wide definition of enlargement recommended by the EPIC Study authors.
• Speaking of the EPIC Study, we expect more and more serious-minded cardiologists will publicly reject the EPIC Study's bogus all-breed definition of heart enlargement, and instead recommend that enlargement be determined on a dog-by-dog basis, ideally relying upon baseline measurements instead of making the fictitious assumption that any dog of any breed with a minimum VHS measurement of 10.5v, or a minimum LA/Ao measurement of 1.6, or a minimum LVIDDN measurement of 1.7 necessarily must have an enlarged heart and therefore must be prescribed pimobendan. These species-wide minimum measurements are, on their face, irresponsible and encourage veterinarians to commit malpractice by prematurely prescribing pimobendan to dogs -- especially cavaliers -- with normal sized hearts.
• Another consequence of the EPIC Study is that the American College of Veterinary Internal Medicine (ACVIM) just might revise its 2009 classification system of stages of MVD. In ACVIM's 2009 ConsensusStatement, it listed the basic stages of MVD (See the chart). Now, there is a proposal, as a consequence of the EPIC Study, to slip another stage in between B2 and C. It likely will be labeled either B3 or B2e, and it is intended to designate those dogs with sufficiently enlarged hearts to warrant prescribing pimobendan for treatment. Hopefully, the veteran cardiologists authoring the new Consensus Statement (Drs. Keene, Atkins, Bonagura, Fox, Haggstrom, Luis Fuentes, Oyama, Rush, Stepien, and Uechi) will not just default to the EPIC Study's sham, species-wide definition of an enlarged heart when distinguishing between Stage B2 and the new Stage B3/B2e.
• We should find out whether spironolactone really can delay the onset of heart failure (Stage C) in MVD-affected dogs currently in Stage B.
• Many vets, including cardiologists, will continue prescribing ACE-inhibitors (like, enalapril) to MVD-affected cavaliers in Stage B2, even though the peer-reviewed studies all show they are worthless in delaying the onset of Stage C. They count on a placebo effect kicking in, to satisfy, as they put it, dog owners' needs to "do something".
•The bogus vendor-and-kibble-manufacturer-sponsored rage to avoid heart disease, by supplementing cavaliers' diets with taurine and avoiding "boutique" dog foods, should finally peter out.
• One of the two national cavalier breed clubs in the USA may be shamed into suggesting that its breeders follow the MVD Breeding Protocol. The other national USA club has been a hopeless cause from its mid-1990s get-go when it comes to encouraging healthful breeding practices.
• On the Chiari-like malformation (CM) and syringomyelia (SM) front, a surprise may be that CM is more of a cause of affected dogs' pain than is SM. This should turn the tables on those know-it-all neurologists we've run into (you know who you are) who insist CM does not cause any pain. They simply don't know what they don't know and proudly refuse to admit it.
• Research might just prove that ingested pesticides and herbicides - be they to kill fleas and ticks or just having worked their way into the dogs' food - really do cause epileptic seizures in cavaliers. But do not expect many general practitioner veterinarians to stop pushing these money-makers, what with advertisement posters and bags of infected dog food stacked in their waiting rooms.
• Hopefully, more and more general practitioner vets will learn that low platelet counts and oversized platelets in cavaliers' blood do not mean the dogs are about bleed to death, or that they have "thick blood". Reports of veterinarians' ignorance about cavaliers' "idiopathic asymptomatic thrombocytopenia" and unwarranted diagnoses of "immune-mediated thrombocytopenia" (IMT) continue to crop up, despite 25 years of published research on the topic.
Let us all hope for the best for our cavalier King Charles spaniels in 2019!
RETURN TO TOP
October 16, 2018:
Anecdotally Speaking:
Many General Practice Vets
are MVD-Quacks!
 Before publication of the EPIC Study in late 2016, the veterinary
decision as to when to start medically treating mitral valve disease (MVD)
in small breed dogs was pretty cut-and-dried. Wait until evidence of
congestive heart failure (CHF). Once fluid invades the dog's lungs, the
accepted consensus was to prescribe an MVD "cocktail" of a diuretic (Lasix)
and pimobendan (Vetmedin) and an ACE-inhibitor (Enalapril) and maybe even
one or two others, like spironolactone.
Before publication of the EPIC Study in late 2016, the veterinary
decision as to when to start medically treating mitral valve disease (MVD)
in small breed dogs was pretty cut-and-dried. Wait until evidence of
congestive heart failure (CHF). Once fluid invades the dog's lungs, the
accepted consensus was to prescribe an MVD "cocktail" of a diuretic (Lasix)
and pimobendan (Vetmedin) and an ACE-inhibitor (Enalapril) and maybe even
one or two others, like spironolactone.
The EPIC Study completely changed that paradigm, but only for one of those drugs, pimobendan. Instead of waiting for heart failure to occur, the threshold for pimobendan became left-side heart enlargement, an event which normally precedes CHF. And that prescription is contingent upon x-rays and echocardiograph scans to assure that there really is any significant left-sided enlargement.
Briefly, to refresh our memories:
The EPIC Study, which was sponsored by Vetmedin's manufacturer, Boehringer Ingelheim Vetmedica, Inc., concluded that Vetmedin (generic name: pimobendan) could be prescribed to any dog affected with mitral valve disease (MVD or MMVD) if the left atrium and left ventricle of the dog's heart are enlarged, based upon two minimum echocardiogram measurements, and a set of x-rays showed that the dog's heart had a Vertebral Heart Sum (VHS) value greater than (>) 10.5.
The EPIC Study's conclusions were a ground-breaking advance for the administration of pimobendan, because previously the drug was not to be prescribed to MVD-affected dogs before their hearts reached congestive heart failure (CHF). One of the reasons for limiting the use of pimobendan to dogs in heart failure before the EPIC trial had been due to previous studies showing that for dogs not yet in CHF, pimobendan could accelerate the progression of MVD and also damage their hearts in other ways.
The EPIC Study's report concluded:
"Chronic oral administration of pimobendan to dogs with echocardiographic and radiographic evidence of cardiomegaly [enlargement] secondary to MMVD, in the absence of concurrent cardiovascular medication, results in the prolongation of the preclinical period, and is safe and well tolerated."
Note that, as big a step as the EPIC Study took for promoting pimobendan, its investigators still emphasized the necessity of both "echocardiographic and radiographic [x-ray] evidence" that the dog's heart is enlarged due to MVD.
Even since the EPIC Study's publication, no competent cardiologist would seriously consider starting an MVD-affected dog on a diuretic before diagnosing CHF. The purpose of the diuretic is to remove fluid from the lungs. If the dog does not yet have any fluid in the lungs, there is no merit in prescribing a diuretic. Indeed, the premature dosing of diuretics can do much more harm than any imagined good. And every cardiologist knows that the published studies have shown that ACE-inhibitors do not delay the onset of heart failure in MVD-affected dogs, especially the cavalier King Charles spaniel (CKCS), the poster child for canine mitral valve disease. The same is true of spironolactone - it is scientifically worthless before heart failure.
But for some inexplicable reason, the EPIC Study's conclusion to start
pimonbendan treatment before CHF was
 like the bursting of a pent up dam for many
general practice veterinarians (GPs). Now, prescribing post-heart-failure
drugs to MVD-affected dogs prior to heart failure has become a blood sport.
like the bursting of a pent up dam for many
general practice veterinarians (GPs). Now, prescribing post-heart-failure
drugs to MVD-affected dogs prior to heart failure has become a blood sport.
Even EPIC Study chief investigator Dr. Adrian Boswood has speculated, in an October 2018 veterinary journal article, about the possibility that "some dogs without CHF might have inappropriately received diuretics."
Perhaps it is because, before the EPIC Study, GPs could detect a mitral valve murmur and lung congestion just as easily as could any cardiologist, and so the GPs also knew when and what to prescribe to treat CHF in MVD-affected dogs. Perhaps the GPs felt that the EPIC Study's recommendation of medicating once heart enlargement is detected has impinged upon the power of their prescription pads when it comes to writing scripts for the MVD cocktail.
Whatever the reason, we have heard report after report after report of general practice vets prescribing all sorts of MVD drugs to cavaliers before heart failure, and in some cases even before any heart enlargement has been diagnosed. In fact, we are talking about some GPs not even bothering to find out if the heart is enlarged once they think they have heard a murmur over the mitral valve, before treating cavaliers with, not only pimobendan, but also with diuretics and ACE-inhibitors. In a few cases, we have heard of GPs starting cavaliers with no enlargement on the high-powered diuretic, torasemide.
There is only one word to describe what is going on here: malpractice! These GP vets are turning into MVD-quacks.
 Remember, you CKCS owners: you need to know as much as possible about
mitral valve disease, because there is no better advocate for your dog than
you. Do not let any MVD-quacks treat your cavaliers before
congestive heart failure, with the exception of pimobendan, but only that
drug if x-rays and echo exams show that the dogs' hearts are significantly
enlarged due to the MVD.
Remember, you CKCS owners: you need to know as much as possible about
mitral valve disease, because there is no better advocate for your dog than
you. Do not let any MVD-quacks treat your cavaliers before
congestive heart failure, with the exception of pimobendan, but only that
drug if x-rays and echo exams show that the dogs' hearts are significantly
enlarged due to the MVD.
RETURN TO TOP
August 26, 2018:
There is no better advocate for your dog,
than YOU!
Don't let ignorant but proud veterinarians
intimidate you
 A
recent peer-reviewed study showed that 80% of veterinarians in the
District of Columbia do not know the rabies quarantine protocol for
unvaccinated pets bitten by high-risk wildlife. This is but one example
of the knowledge gaps of many of the doctors who are supposed to be
keeping our dogs healthy. Whether it is intellectual laziness or willful
ignorance, it is very possible that your cavalier's veterinarian does
not know how to recognize or diagnose or treat disorders which are
common to cavalier King Charles spaniels.
A
recent peer-reviewed study showed that 80% of veterinarians in the
District of Columbia do not know the rabies quarantine protocol for
unvaccinated pets bitten by high-risk wildlife. This is but one example
of the knowledge gaps of many of the doctors who are supposed to be
keeping our dogs healthy. Whether it is intellectual laziness or willful
ignorance, it is very possible that your cavalier's veterinarian does
not know how to recognize or diagnose or treat disorders which are
common to cavalier King Charles spaniels.
Take cavaliers' blood platelets for example. Over half of all totally healthy CKCSs likely will have extremely low blood platelet counts when their blood is analyzed by machines at vet offices. This is a purely harmless disorder in the breed, due mainly because cavaliers' platelets tend to clump and appear much larger than the normal size of platelets in blood samples. Veterinarians have been taught in school that low platelet counts could mean that the dog is suffering from "immune-mediated thrombocytopenia (IMT)" and that it needs an immediate intraveneous transfusion of steroids. In a healthy CKCS with a low platelet count, this totally inappropriate procedure is so dangerous that it would kill the dog, and unfortunately it has killed healthy cavaliers in the past.
When many vets are confronted with their ignorance about cavalier-specific disorders which may be second nature to long-time cavalier owners, the vets' reactions often are hostile. As in, "I have a doctorate in veterinary medicine, and I take 20 hours of continuing education per year. So, I know what I'm talking about, and you don't!" They might accuse you of being an 'instant Internet expert' after perusing Google for a couple of hours.
But the fact is, they very probably don't know everything they need to know to adequately treat your cavaliers. Here is a list of the main hereditary disorders which either are unique to CKCSs or are more common in them than most other breeds (researcher veterinarians call these "pre-disposed to"):
Mitral valve disease (MVD)
Chiari-like malformation (CM)
Syringomyelia (SM)
Low blood platelets (idiopathic asymptomatic
thrombocytopenia)
Primary secretory otitis media (PSOM) - glue ear
Pneumocystis pneumonia
Episodic falling syndrome
Curly coat syndrome
Dry eye syndrome
Fly catchers syndrome
Deafness - progressive
hereditary hearing loss
Cerebellar infarcts - strokes
Xanthinuria
Eosinophilic stomatitis
Masticatory muscle myositis (MMM)
Obesity
Chronic pancreatitis
Exocrine pancreatic insufficiency (EPI)
Brachycephalic airway obstruction syndrome (BAOS)
Intervertebral disk
disease (IVDD)
Diabetes mellitus
 Hip
dysplasia (HD)
Hip
dysplasia (HD)
Idiopathic epilepsy
Chronic kidney disesase
Muscular
dystrophy
Patellar luxation
Temporomandibular joint dysplasia
The bottom half of the above list may be fairly common in several breeds, but the top half are either uniquely or particularly common in the CKCS. If your veterinarian is not familiar with all of these disorders, you need to be -- at least with their symptoms. You need to know enough to recognize when your cavalier needs veterinary care and to ask the vet, "What about this disease?" or "Could it be that disease?" You need to be your dog's primary advocate.
And if you get silence and a blank (or cold) look in return, you and your dog need a vet who will at least admit his ignorance and express his willingness to look into it and find out the answers. Don't let ignorant but proud veterinarians intimidate you when it comes to your dog's health.
RETURN TO TOP
May 7, 2018:
D-ribose can boost the energy in MVD-affected hearts
D-ribose nutritional supplement replenishes
adenosine triphosphate
(ATP) faster than the heart can itself
D-ribose can prevent heart enlargement
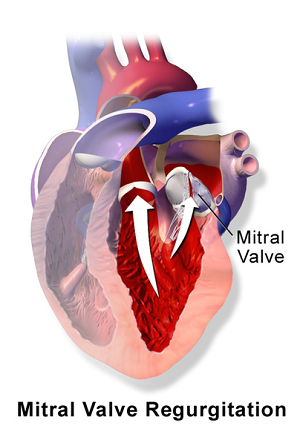 As
mitral valve disease (MVD) progresses in the cavalier King Charles
spaniel, and more and more blood backflows (regurgitates) through the
mitral valve, the volume overload of blood in the heart stresses the
heart's walls and drains the heart of its two main sources of energy --
adenosine triphosphate (ATP) and oxygen.
As
mitral valve disease (MVD) progresses in the cavalier King Charles
spaniel, and more and more blood backflows (regurgitates) through the
mitral valve, the volume overload of blood in the heart stresses the
heart's walls and drains the heart of its two main sources of energy --
adenosine triphosphate (ATP) and oxygen.
ATP is essential for the heart to function properly. It is an energy-carrying molecule found in all cells of the body, including in particular, the dog's heart. When energy is needed by the cell, it is converted from storage molecules into ATP. ATP then delivers energy to places within the cell where energy-consuming activities are taking place. ATP is essential for the heart to function properly. When the heart is stressed and over-worked, as it is during volume overload due to mitral valve regurgitation, the process of maintaining necessary levels of the supply of ATP do not meet the demand, and the walls of the heart weaken due to the stress of the volume overload, causing them to stretch and enlarge.
D-ribose is a primary component of ATP. It is the only compound used by the dog's body to replenish diminished ATP energy stores.
D-ribose
as a nutritional supplement provides needed added energy to the heart
muscle and walls. It is a natural sugar which the canine body produces
on its own but which can be depleted when the stressful forces of mitral
valve disease (MVD)
begin to drain the heart of its ability to compensate for the affects of
mitral valve regurgitation.
 The dog's heart and skeletal muscles can
only make enough D-ribose to manage their day-to-day needs when those
cells are not under stress. When dogs are in heart failure or are
approaching it, the heart cells cannot make enough D-ribose.
The dog's heart and skeletal muscles can
only make enough D-ribose to manage their day-to-day needs when those
cells are not under stress. When dogs are in heart failure or are
approaching it, the heart cells cannot make enough D-ribose.
When the MVD-affected left atrium (LA) and left ventricle (LV) of the heart are stressed and over-worked during volume overload due to mitral valve regurgitation, the heart consumes greater quantities of ATP. At that point, the process of the heart maintaining necessary levels of ATP does not meet the demand, and the walls of the LA and LV weaken due to the stress of the volume overload, causing them to stretch and enlarge. The dog's natural replenishment of necessary levels of ATP can take a considerable amount of time in the hearts of dogs affected with MVD. D-ribose, when taken as a nutritional supplement, bypasses the slow conversion steps needed to recreate ATP and rapidly replenishes the supply of ATP which the heart needs to offset the stresses of mitral regurgitation.
D-ribose is available on-line and at health food stores. All holistic supplements should be taken only if advised to do so by an holistically trained, licensed veterinarian. Search engine webpages for finding holistic veterinarians in the United States and Canada are located here, and in the United Kingdom, here.
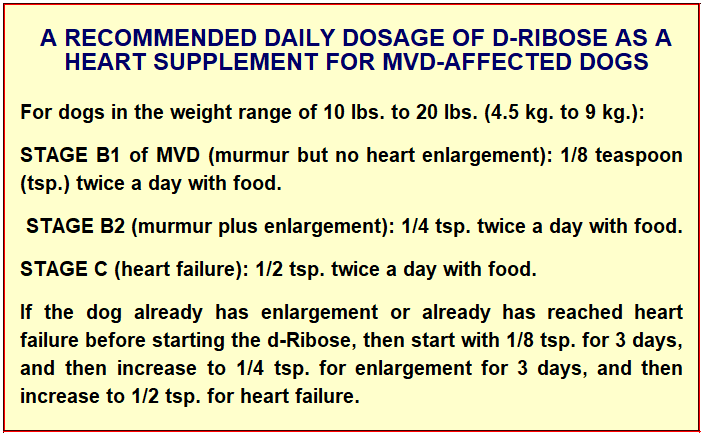
See these articles for more information:
• February 1989: "No significant ATP recovery occurred after 24 hr in the control dogs, but in the ribose-treated animals, ATP levels rebounded to 85% of control by 24 hr. Total myocardial adenine nucleotide content and energy charge also recovered in the ribose group but not in the control animals. The ribose infusion, therefore, significantly enhanced the recovery of energy levels in the postischemic myocardium in the intact animals."
• Summer 2004: "Patients with congestive heart failure often experience fatigue despite intensive pharmacological therapy. Ribose can aid the recovery of ATP levels and, hence, diastolic function. Clinical trials have shown that ribose supplementation improves ischemic threshold and enhances diastolic function in congestive heart failure."
• July 2007: "We then turned our attention to ribose. Ribose is made in your body in a slow, laborious process and cannot be found in food. ... Not having ribose would be like trying to build a fire without kindling--nothing would happen. ... I am now recommending ribose for ... heart problem patients ... . In fact, one patient in our study had atrial fibrillation that resolved with ribose, and most practitioners using it are finding it to be simply outstanding for their cardiac patients in general."
• May 2009: "The preservation of ATP is vital in the heart as a reduction in ATP level corresponds to a loss of diastolic function. The administration of ribose supports purine synthesis and salvage pathways promoting diastolic function. ... Cardiovascular function depends on the operational capacity of myocardial cells to generate the energy to expand and contract. Insufficient myocardial energy contributes significantly to CHF. Literally, heart failure is an "energy-starved heart." ... In simple terms, sick hearts leak out and lose vital ATP, and the endogenous restoration of ATP cannot keep pace with this insidious deficit and relentless depletion. When ATP levels drop, diastolic function -- the most important precursor of congestive heart failure -- deteriorates. D-ribose, L-carnitine, and CoQ10 act to promote cardiac energy metabolism and help normalize myocardial adenine nucleotide concentrations. These naturally occurring compounds exert a physiological benefit that directly affects heart function. As the rate-limiting compound, supplemental ribose supports ATP quantity in the synthesis of new ATP. CoQ10 and carnitine enhance the turnover of ATP in the inner mitochondrial chain. All are recommended as adjunctive metabolic therapies in the treatment of heart failure."
• June 2015: " Previous studies have demonstrated that diastolic function is energy dependent and supplemental D-ribose has shown to improve diastolic dysfunction. This study investigated what role D-ribose might play in congestive heart failure patients with preserved systolic function and diastolic dysfunction. ... Results: An improvement in their tissue Doppler velocity (E′), which was maintained at 9 weeks, was demonstrated in 64% of the patients."
• June 2016: "Myxomatous mitral valve disease (MMVD) is the most common cause of mitral valve regurgitation (MVR) in small animals, with a prevalence of approximately 30% in small breed dogs over the age of 10 years. The time course of the disease influences the clinical symptoms. If MVR occurs slowly, there is time for compensation and the animal may be asymptomatic; if MVR develops acutely, the clinical signs can be very severe. With MVR there is a decrease in stroke volume because part of the outflow of the left ventricle (LV) is directed back to the left atrium (LA). The regurgitant fraction causes volume overload of the LA and LV, according to Laplace's law. Volume overload increases wall stress, which in turn requires greater adenosine triphosphate (ATP) and O2 consumption. As a compensatory mechanism, myocardial hypertrophy occurs. The chronic volume overload of the LA can lead to dilation of the atrium, with increased pressure and pulmonary congestion, resulting in pulmonary oedema and congestive heart failure (CHF). Possible complications of MMVD are right-sided CHF, due to direct involvement of the tricuspid valve or as a consequence of pulmonary hypertension (PH), and arrhythmias, such as atrial fibrillation (AF), due to atrial enlargement."
• May 2017: "D-ribose is a carbohydrate (sugar) that is important for the body's cellular metabolism through the production of a substance known as ATP (adenosine trisphosphate). Patients suffering from severe heart disease, especially heart diseases such as dilated cardiomyopathy, may have severely depleted stores of ATP within heart muscle tissue. A small study in humans with congestive heart failure suggested that supplementation with ribose may improve heart muscle function."
• January 2018: " Mitochondria are important organelles referred to as cellular powerhouses for their unique properties of cellularenergy production. With many pathologic conditions and aging, mitochondrial function declines, and there is a reduction in the production of adenosine triphosphate. The energy carrying molecule generated by cellular respiration and by pentose phosphate pathway, an alternative pathway of glucose metabolism. D-ribose is a naturally occurring monosaccharide found in the cells and particularly in the mitochondria is essential in energy production. Without sufficient energy, cells cannot maintain integrity and function. Supplemental D-ribose has been shown to improve cellular processes when there is mitochondrial dysfunction. When individuals take supplemental D-ribose, it can bypass part of the pentose pathway to produce D-ribose-5-phosphate for the production of energy. In this article, we review how energy is produced by cellular respiration, the pentose pathway, and the use of supplemental D-ribose."
• March 2018: "Cardiovascular disease still remains the leading cause of deaths worldwide. ... All cells require adequate adenosine triphosphate (ATP) levels to maintain their integrity and function. ... D-ribose, a naturally occurring pentose carbohydrate, has been shown to increase cellular energy levels and improve function following ischemia in pre-clinical studies and have demonstrated potential benefits in clinical evaluations. This review paper presents an overview of ischemic cardiovascular disease and the potential role that D-ribose could play in improving myocardial energy levels and function in the area of ischemic cardiovascular diseases."
RETURN TO TOP
December 22, 2017:
Did the EPIC Study investigators intentionally enroll
Stage B1
cavaliers in their Stage B2 trial?
Sadly, the evidence points to "YES!"
The consequences invalidate the results of the EPIC Study trial
EPIC's bogus enrollment criteria have become the treatment parameters
 The
EPIC Study was an effort by the manufacturer of Vetmedin (brand
name for pimobendan) to justify selling that very expensive drug to
owners of small-breed dogs diagnosed with myxomatous mitral valve
disease (MVD) prior to the onset of heart failure (CHF). Up until then,
pimobendan was approved in Europe and the United States only for
MVD-affected dogs already in CHF. *
The
EPIC Study was an effort by the manufacturer of Vetmedin (brand
name for pimobendan) to justify selling that very expensive drug to
owners of small-breed dogs diagnosed with myxomatous mitral valve
disease (MVD) prior to the onset of heart failure (CHF). Up until then,
pimobendan was approved in Europe and the United States only for
MVD-affected dogs already in CHF. *
* Technically speaking, in the USA, pimobendan remains approved by the FDA only for MVD-affected dogs already in heart failure.
A reason for limiting administering pimobendan to dogs in CHF was that previously published veterinary research reported evidence that the drug could accelerate the progression of the MVD in dogs not yet in heart failure.
For the EPIC Study, the manufacturer hired thirty-six board certified veterinary cardiologists from around the world, led by a team of three lead investigators, to conduct a pimobendan/placebo trial on 360 MVD-affected dogs, all at the manufacturer's expense.
The announced intention was that all of those dogs would have enlarged
hearts due to their MVD. In other
 words, we were led to believe that the
dogs were supposed to be in ACVIM Stage B2 (defined as: "asymptomatic patients that have
hemo-dynamically significant valve regurgitation, as evidenced by
radiographic or echocardiographic findings of left-sided heart enlargement").
However, in the EPIC Study criteria, the ACVIM's definition of Stage B2 was
ignored. Instead, the term "enlargement" was peculiarly defined by the lead
investigators as "echocardiographic and radiographic evidence of cardiac
enlargement by 3 different heart size criteria." Note that the EPIC Study
investigators ignored ACVIM's term, "findings of left-sided heart
enlargement", and substituted
"heart size criteria". "Enlargement" necessarily means increasing in size
over time. A one-off measurement of "heart size" does not measure whether
the heart has increased in size, because there is no previous measurement
for comparison. This is particularly true when the one-time heart size measurement is
species-wide, as the EPIC Study measurements are.
words, we were led to believe that the
dogs were supposed to be in ACVIM Stage B2 (defined as: "asymptomatic patients that have
hemo-dynamically significant valve regurgitation, as evidenced by
radiographic or echocardiographic findings of left-sided heart enlargement").
However, in the EPIC Study criteria, the ACVIM's definition of Stage B2 was
ignored. Instead, the term "enlargement" was peculiarly defined by the lead
investigators as "echocardiographic and radiographic evidence of cardiac
enlargement by 3 different heart size criteria." Note that the EPIC Study
investigators ignored ACVIM's term, "findings of left-sided heart
enlargement", and substituted
"heart size criteria". "Enlargement" necessarily means increasing in size
over time. A one-off measurement of "heart size" does not measure whether
the heart has increased in size, because there is no previous measurement
for comparison. This is particularly true when the one-time heart size measurement is
species-wide, as the EPIC Study measurements are.
What were the "3 different heart size criteria"?
• Radiographic measurement of the vertebral heart score (VHS) > 10.5
• Echocardiographic measurement of the left atrial-to-aortic ratio (LA/Ao) >1.6
• Echocardiographic measurement of the normalized left ventricular internal diameter in diastole (LVIDDN) > 1.7.
These minimum criteria are an example of what veterinary researchers call "quantitative measurement methods", which are designed to dumb-down the level of professionalism which one otherwise would expect from both investigative and clinical veterinarians in performing their examinations.
The most striking thing about the three criteria is that, when applied to the average cavalier King Charles spaniel (CKCS), two of them are measurements of dogs with normal sized hearts and not enlarged ones. Since cavaliers comprised nearly half of all of the dogs in the trial (45.5% to be precise), these criteria essentially assured that a very substantial number of the dogs would have started the trial with no heart enlargement at all. In other words, they probably were in ACVIM Stage B1 and not in Stage B2. No one knows for certain because no independent, subjective examinations of the dogs' hearts were performed, such as comparing current and baseline radiographs and echo scans, or eyeballing the shapes of the dogs' hearts on radiographs to find classic bulging left atriums and rounded left ventricles. But it is reasonable to infer as the best explanation that many dogs with normal-sized hearts were enrolled, based upon the empirical evidence regarding the three criteria, discussed in some detail below.
VHS > 10.5 -- The radiographic VHS value > 10.5 as a definition of enlargement is laughable for the average cavalier. Even the March 2005 veterinary journal article footnoted in the EPIC Study report, to justify selecting that VHS value, found that a VHS value of 10.8 ± 0.49 in cavaliers was "normal", meaning that those dogs' hearts were not enlarged at all. In that 2005 article, researchers* studied 50 sets of heart radiographs of cavaliers and stated:
"The mean VHS for normal cavalier King Charles spaniels was 10.8 ± 0.49 v (10.0-11.4). ... The use of breed-specific VHS values is needed for the VHS method to have a high specificity for normal heart size."
* One of the authors of the 2005 article was Dr. Jens Haggstrom, who also was one of the three lead investigators in the EPIC Study.
So, obviously, the EPIC Study investigators had to know that potentially as many as 45.5% of the dogs in the trial did not have enlarged hearts at the start, based upon the trial's VHS value criterion.
Not only did they have to have known it, but two of the lead investigators actually admitted it. In an audio interview (at time 31:24) in November 2016, lead investigator Dr. Adrian Boswood said:
"A vertebral heart score of 10.5 is in the normal range for some dogs, particularly cavaliers actually."
Another of the three lead investigators, Dr. Sonya Gordon, wrote in a June 2017 article:
"However, given the potential low accuracy of depending solely on a radiographic VHS greater than 10.5, ... and that there are known breed-related differences in normal VHS reference ranges with much higher normal VHS ranges reported in some breeds, including the CKCS, ... ."
Dr. Anna Beber tidily sums up this emperor-has-no-clothes situation in her March 2018 master's thesis when she writes:
"Using the vertebral heart score cut off of 10.5v in the EPIC study, all of the 'normal' Cavalier King Charles Spaniels in this study (defined by subjective impression consensus opinion) would have been considered to have cardiomegaly and therefore potentially received treatment unnecessarily. ... Therefore, to ensure that a VHS is of value, the author suggests that large numbers of breed 'normals' need to be used to establish a more reliable reference range."
LVIDDN > 1.7 - In that same November 2016 audio interview (at time 31:06), Dr. Boswood admitted that the LVIDDN of 1.7 also is below the range for enlargement. He said:
"Now interestingly, if you look in the literature, the normalized left ventricular diameter of 1.7 is in the normal range. The abnormal is above about 1.85, [1.]9, 1.9 depending upon how you read it, so that's nudging the top of the normal range but still normal."
Perhaps Dr. Boswood was referring to the normal LVIDDN range as high as 1.85 reported in this widely-cited 2004 article, in which its authors stated:
"If the result is between 1.27 and 1.85, the value is within the normal [95%] prediction interval for this study." (Emphasis added.)
EPIC lead investigator Sonya Gordon made a similar admission in a 2017 article when she and her co-authors specifically cited that 2004 article, writing:
"In addition, all dogs with stage B2 MMVD were required to have a left ventricular internal dimension (LVID) in diastole normalized to body weight 1.7. The selected cutoff value for normalized LVID in diastole was based on a study that found higher values, although technically within the normal reported range (<1.85), predicted increased risk of death in dogs with MMVD." (Emphasis added.)
So, to Dr. Gordon, Stage B2 has nothing to do with heart enlargement. So much for the "validity" of the LVIDDN measurement as evidence of enlargement.
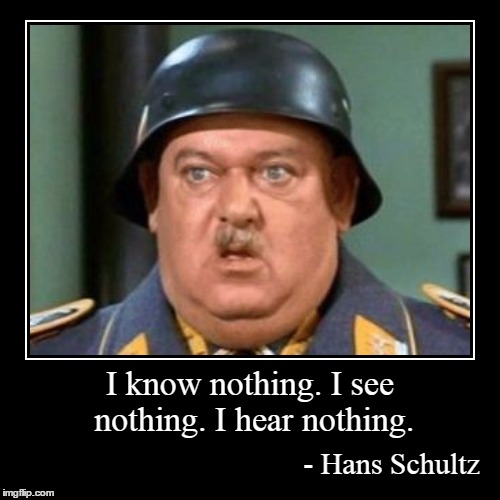 So it appears from this empirical evidence, rather conclusively, that the investigators knew that
the criteria had to encompass Stage B1 dogs in addition to Stage B2 dogs,
and it is a reasonable inference that they fully intended that several of the 360 dogs
start the trial with normal-sized hearts.
The most charitable conclusion to draw from this evidence is that
the investigators chose to not try to find out what they knew that they did not
know. In other words, they opted for willful ignorance, in order to
meet a pre-determined number of patients. A severe consequence of using these normal-sized-heart
criteria was to put possibly over a hundred Stage B1 cavaliers at a serious health
risk during the trial just for the sake of the EPIC Study's full sponsor
being able to brag about 360 dogs being in the study.
So it appears from this empirical evidence, rather conclusively, that the investigators knew that
the criteria had to encompass Stage B1 dogs in addition to Stage B2 dogs,
and it is a reasonable inference that they fully intended that several of the 360 dogs
start the trial with normal-sized hearts.
The most charitable conclusion to draw from this evidence is that
the investigators chose to not try to find out what they knew that they did not
know. In other words, they opted for willful ignorance, in order to
meet a pre-determined number of patients. A severe consequence of using these normal-sized-heart
criteria was to put possibly over a hundred Stage B1 cavaliers at a serious health
risk during the trial just for the sake of the EPIC Study's full sponsor
being able to brag about 360 dogs being in the study.
Another significant consequence of including Stage B1 dogs in the
trial was to totally nullify the validity of the EPIC Study's findings and
conclusions.
 Since the investigators did not identify which dogs
were in Stage B1, they had no assurance that the two groups - the pimobendan
group and the placebo group - had equal numbers of dogs with normal sized
hearts at the start of the trial.
Since the investigators did not identify which dogs
were in Stage B1, they had no assurance that the two groups - the pimobendan
group and the placebo group - had equal numbers of dogs with normal sized
hearts at the start of the trial.
If a greater number of dogs without enlarged hearts was placed in the pimobendan group, then the median time to primary endpoint for that group necessarily would have been artificially extended beyond that of the placebo group. Because of the unscientific manner in which heart enlargement was "defined" by the lead investigators, there would be no data for determining now whether an even number of Stage B1 dogs were placed in each group.
But
the worst consequence of all about these bogus inclusion criteria is
that thoughless cardiologists have made them the species-wide parameters
for prescribing pimobendan to any and all MVD-affected dogs, regardless of
whether the dogs actually have enlarged hearts or not.
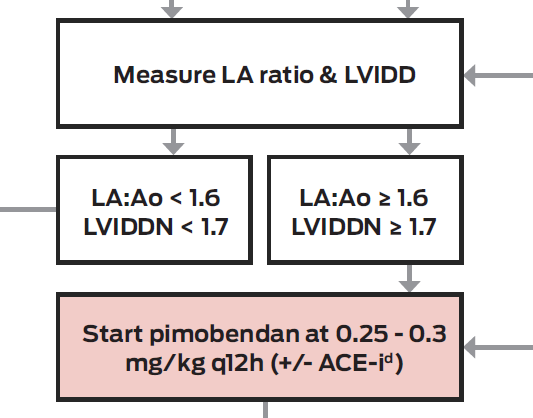 See, for example, at right, this segment of a treatment "algorithm"
published by the Cardiac Education Group
(CEG), a group of seven board certified veterinary cardiologists in the
United States, in their December 2016
"Recommendation".
Observe that CEG's chart recommends that if the dog's heart measurements are
LA/Ao > 1.6 and LVIDDN > 1.7, then ipso facto, the dog is presumed
to be in Stage B2 and needs to start the pimobendan.
See, for example, at right, this segment of a treatment "algorithm"
published by the Cardiac Education Group
(CEG), a group of seven board certified veterinary cardiologists in the
United States, in their December 2016
"Recommendation".
Observe that CEG's chart recommends that if the dog's heart measurements are
LA/Ao > 1.6 and LVIDDN > 1.7, then ipso facto, the dog is presumed
to be in Stage B2 and needs to start the pimobendan.
Below are a couple of "boilerplate" paragraphs in a typical cardiologist's typical post-EPIC report following a CKCS's echocardiograph examination. This is evidence that the sham EPIC Study inclusion criteria are being used as diagnositic parameters for determining that cavaliers are in Stage B2 despite the fact that the parameters only measure normal-sized cavalier hearts.
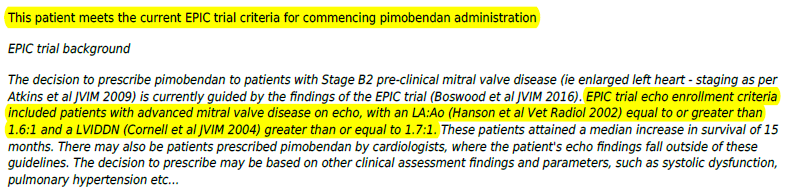
Even Dr. Boswood, despite his confessed awareness that the EPIC parameters for "enlarged" hearts actually are for normal-sized hearts of cavaliers (and a few other breeds), applies those bogus parameters when prescribing pimobendan to his patients. He states, in a March 2018 article sponsored by the manufacturer of Vetmedin:
"On the basis of the results of the EPIC study I now routinely recommend the use of pimobendan in dogs with preclinical MMVD and evidence of cardiac enlargement (sufficient to meet the EPIC inclusion criteria) at a dose of approximately 0.5 mg/kg/day divided into two doses (0.25 mg/kg twice a day).."
Far too many cardiologists in this post-EPIC world have begun to ignore their specialized education in cardiomegaly. They no longer use their cardiac training to determine whether the patient before them really does have an enlarged heart. Instead, they have suspended their better judgment and allowed the EPIC Study authors to re-define enlargement to being a set of arbitrary one-time measurements of size. They opt for the dumbed-down quantitative measurement method. Even though two of those EPIC Study authors have ridiculed one of their own measurements (VHS > 10.5) and one of the authors has mocked another of their measurements (LVIDDN > 1.7), and none of the three measurements have any peer-reviewed research to support them, these practitioner cardiologists mindlessly accept EPIC's size dimensions as the new definition of species-wide heart enlargement. And more than any other breed, the cavalier King Charles spaniel is the big loser, the breed put at greatest risk.
RETURN TO TOP
November 7, 2017:
Why are cardiology researchers inventing bogus definitions of species-wide heart enlargement to test risky drugs?
Arbitrary, species-wide measurements defining heart enlargement
endanger CKCSs the most
What motivates cardiologists to put MVD-affected dogs at risk?
• Only old-fashioned, hands-on, subjective exams will accurately
determine if enlargement exists.
• Species-wide parameters used to
define
heart enlargement in six recent studies are bogus.
• These researchers have no
species-wide research to support their enlargement parameters.
• Many
veterinarians either cannot take or read heart x-rays
accurately.
• Why do researchers define species-wide heart
enlargement without any
research to determine what that definition should be?
 Recently, veterinary cardiologists researching dogs diagnosed with
myxomatous mitral
valve disease (MVD) have turned their focus from the point of congestive
heart failure (CHF) - ACVIM Stage C - to an earlier event, enlargement of
the left side of the dogs' hearts - ACVIM Stage B2. For at least the past decade and a half, CHF has been the
dividing line between medicating and not medicating MVD. For example, in
2007, pimobendan was approved by the
US Food and Drug Administration to
treat MVD-affected dogs once they have reached CHF, but not before heart
failure.
Research completed in 2002 established that ACE-inhibitors do not
delay the onset of CHF in cavalier King Charles spaniels (CKCS) and
therefore should be reserved for dogs in Stage C. Diuretics,
of course, would not be appropriate prior to congestive heart failure,
because their purpose is to remove retained fluids from the lungs, a
situation which does not exist until CHF occurs.
Recently, veterinary cardiologists researching dogs diagnosed with
myxomatous mitral
valve disease (MVD) have turned their focus from the point of congestive
heart failure (CHF) - ACVIM Stage C - to an earlier event, enlargement of
the left side of the dogs' hearts - ACVIM Stage B2. For at least the past decade and a half, CHF has been the
dividing line between medicating and not medicating MVD. For example, in
2007, pimobendan was approved by the
US Food and Drug Administration to
treat MVD-affected dogs once they have reached CHF, but not before heart
failure.
Research completed in 2002 established that ACE-inhibitors do not
delay the onset of CHF in cavalier King Charles spaniels (CKCS) and
therefore should be reserved for dogs in Stage C. Diuretics,
of course, would not be appropriate prior to congestive heart failure,
because their purpose is to remove retained fluids from the lungs, a
situation which does not exist until CHF occurs.
In the past year, veterinary research publications have been focusing their medication advice upon MVD-affected dogs with enlarged hearts rather than those in CHF. Research into the efficacy of pimobendan and other drugs in treating MVD-affected dogs with enlarged hearts but prior to CHF - in other words, in Stage B2 - has prompted this change of focus.
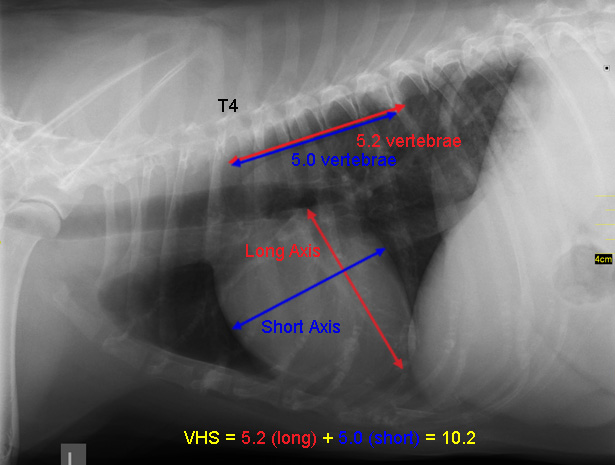 The point at which a dog reaches CHF has been relatively clear-cut, based
upon constant rapid breathing, x-rays showing pulmonary congestion, and
other physically observable signs. Most primary care veterinarians have been
trained to recognize the symptoms of CHF. However, detecting heart
enlargement - which customarily occurs before CHF - calls for a totally
different approach.
The point at which a dog reaches CHF has been relatively clear-cut, based
upon constant rapid breathing, x-rays showing pulmonary congestion, and
other physically observable signs. Most primary care veterinarians have been
trained to recognize the symptoms of CHF. However, detecting heart
enlargement - which customarily occurs before CHF - calls for a totally
different approach.
Since at least the mid-1990s, there have been widely accepted, accurate means of determining whether a dog's heart has enlarged or not. The most accurate has been the vertebral heart score (VHS) method proposed by Dr. James Buchanan of PennVet in 1995. The VHS method relates the long and short axis dimensions of the dog's heart on x-rays to the distance between vertebrae starting at vertebra T4 and extending towards the dog's tail. Since these vertebrae conveniently appear on x-rays of the dogs' hearts, all the clinician needs is a set of calipers to measure the distances on the heart and then apply them to the vertebrae.
Enlargement means getting larger - not just being large
Of course, one set of x-rays
will provide only one set of measurements. Enlargement means that the size
of the
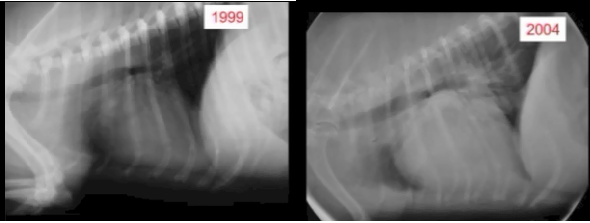 heart
has gotten bigger over time. Therefore, one set of measure-ments on a single
day does not tell the clinician that the dog's heart is enlarged, because
the clinician does not know whether or not the heart ever was smaller than
it is on the single day it was measured. To determine if a dog's heart is
enlarged, the VHS system works only if there also is an earlier, baseline
set of x-rays taken before any enlargement has been suspected. (The x-rays
above,
left show the increase in heart size of one cavalier over 5 years. --
Courtesy of the Royal Veterinary College.)
heart
has gotten bigger over time. Therefore, one set of measure-ments on a single
day does not tell the clinician that the dog's heart is enlarged, because
the clinician does not know whether or not the heart ever was smaller than
it is on the single day it was measured. To determine if a dog's heart is
enlarged, the VHS system works only if there also is an earlier, baseline
set of x-rays taken before any enlargement has been suspected. (The x-rays
above,
left show the increase in heart size of one cavalier over 5 years. --
Courtesy of the Royal Veterinary College.)
If a baseline comparison is not an option, another method for determining if the dog's heart is enlarged is to compare the shape of the heart -- the cardiac silhouette -- as it appears in an x-ray with the known shapes of normal hearts for that breed. This is considered a more "subjective" means of diagnosing enlargement and usually is left to the experts - the cardiologists and radiologists who are most familiar with the shape of the normal and enlarged canine heart. They look for a more rounded appearance, bulging, and other deviations from the typical normally shaped heart, and whether the heart is impacting the trachea, in addition to the size of the heart. (To the practiced eye of a cardiologist, the heart in the 2004 x-ray above will clearly show enlargement.)
Indeed, the very definition of ACVIM Stage B2, in the 2009 Consensus Statement which introduced the Stages A through D of MVD, compels veterinarians to examine each heart subjectively. It calls for x-rays (both baseline and current), echocardiographic examinations if necessary, plus blood pressure measurement, basic bloodwork and urinalysis, and a specific determination of a "clearly enlarged" left atrium, and/or left ventricle. It states:
"Diagnosis for Stage B Consensus recommendations:
• Thoracic radiography is recommended in all patients to assess the hemodynamic significance of the murmur and also to obtain baseline thoracic radiographs at a time when the patient is asymptomatic for CVHD.
• Blood pressure measurement is recommended for all patients.
• In small breed dogs with typical murmurs, echocardiography is recommended to answer specific questions regarding either cardiac chamber enlargement or the cause of the murmur if those questions are not answered adequately by auscultation and thoracic radiography.
• Echocardiography generally is indicated in larger breed dogs because the murmur of MR is more likely to be related to other causes (eg, dilated cardiomyopathy).
• Basic laboratory work (a minimum of hematocrit, total protein concentration, serum creatinine concentration, and urinalysis) is indicated in all patients. ...
• Stage B2: Hemodynamically significant MR with cardiac remodeling (defined as clearly enlarged LA, LV, or both); normotensive."
Recent veterinary articles ignore enlargement and rely only upon heart size
But now, it appears that those careful, cautious means of determining if a dog's heart is enlarged or not are being ignored. Instead, some researchers are turning to what they call more "objective" devices - "parameters" - for diagnosing enlarged hearts. They use the VHS value method primarily, and they might throw in a couple of echocardiographic measurements, if an ultrasound device is available and the dog's owner is willing to pay for its use. But oddly, the measurements now are species-wide - not even limited to breed-specific, much less the individual canine patient.
These researchers contend, in their published articles, that these species-wide parameters are the precise measurements of the thresholds of enlarged hearts. In other words, anything less than their minimums define a normal heart and anything above their minimums is necessarily an enlarged heart in any dog of any breed. They use these ad hoc definitions of enlargement both as inclusion criteria in their testing and as recommendations to clinicians in their conclusions.
The researchers also have bastardized the definition of Stage B2 in that they use the term but ignore its meaning. The ACVIM's Stage B2 definition is of the Enlarged heart. But these current researchers, while using the label "Stage B2", have re-defined it to describe only the Large heart.
One thing the researchers neglect to do is include any citations to prior research or other peer-reviewed justification for their minimum parameters. Oh, they might throw in a footnote or two with a cited article when they list their inclusion criteria, but those cited articles are either irrelevant to the subject matter or even expressly contradict those parameters. The obvious reason they do not - and cannot - cite any peer-reviewed research justifying their species-wide minimum heart enlargement measurements is, because none exists.
The first of these studies discussed below, the EPIC Study, defines heart enlargement for all dogs by three minimum measurements - a VHS value and two echo measurements. Its VHS minimum value is 10.5. Other studies discussed below define species-wide heart enlargement by arbitrary VHS values alone, varying from minimum values of 11.0 to 11.5.
We will address the EPIC Study's arbitrary echo measurements herein later. But regarding minimum VHS values, keep in mind that there is at least one peer-reviewed publication which expressly contradicts the notion that all cavaliers with a VHS value of 10.5 or 11.0 or even 11.5 must have heart enlargement. In "Use of breed-specific ranges for the vertebral heart scale as an aid to the radiographic diagnosis of cardiac disease in dogs", the researchers found a cavalier with a normal sized (meaning, unenlarged) heart having a VHS value as high as 11.7. The authors stated:
"There were significant differences between the mean values of the scale for the different breeds; the normal boxer dogs had a significantly higher mean value than the normal dogs of all the other breeds, and the labrador retrievers had a significantly higher mean value than all the other breeds except the boxer and the cavalier King Charles spaniel. ... Cavalier King Charles spaniel: Normal ranges: 9.9-11-7."
In "Interobserver Variability of Vertebral Heart Size Measurements in Dogs with Normal and Enlarged Hearts", the VHS range for cavaliers was as high as 11.4. Other breeds reportedly have normal sizes as high as above 14.0. Those authors wrote:
"The mean VHS for normal cavalier King Charles spaniels was 10.8 ± 0.49 v (10.0-11.4) ... The use of breed-specific VHS values is needed for the VHS method to have a high specificity for normal heart size. ... Individual variations in actual heart size and vertebral length between dogs need to be considered as well as narrowed disc spaces."
That last sentence is key. Even breed-specific VHS measurements are unreliable. The only way to determine if a dog has an enlarged heart is to thoroughly examine that dog - be "patient-specific" - and not assume that even a breed-specific VHS value is accurate for that dog.
Now to review the six recent articles:
The EPIC Study's "enlargement" parameters = normal-sized hearts
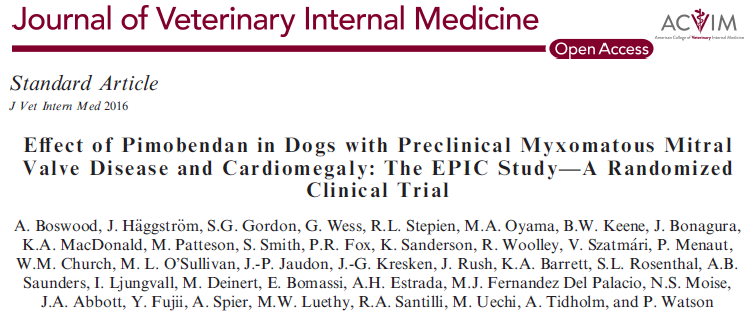
1. The EPIC Study. The earliest of these recent reports using species-wide minimum parameters for determining heart enlargement is the EPIC Study report, published in the November 2016 issue of the Journal of Veterinary Internal Medicine by three lead investigators (A. Boswood, J. Haggstrom, S.G. Gordon) and 33 other cardiologists. How this article's inclusion criteria slipped past peer review is beyond comprehension. But keep in mind that the study was funded in full, including research, travel, speaking fees, consultancy fees, and preparation of educational materials, even down to matching windbreaker jackets for each of the 36 participating cardiologists, by Boehringer Ingelheim Vetmedica, Inc., the manufacturer of Vetmedin (a brand name for pimobendan).
Now this was to be a very delicate study, because much of the prior published evidence about administering pimobendan to dogs before they reached heart failure was that it could drastically accelerate the progression of MVD, and there have been reports of pre-CHF dogs suddenly dropping dead shortly after starting on pimobendan. The USA's Food and Drug Administration had warned against prescribing pimobendan before heart failure, and even its manufacturer included such warnings on the packaging.
So, recognizing the vital importance of a study on the safety and efficacy of administering pimobendan before heart failure, one would hope that the EPIC Study's parameters would assure that the 360 dogs actually had enlarged hearts. No such luck.
It's authors selected three parameters, applied to all 360 MVD-affected dogs of numerous breeds (including 161 cavaliers - 45.5%) in the study and thereafter recommended for all small MVD-affected dogs in the future. Its parameters are:
• Radiographic measurement of the vertebral heart score (VHS) > 10.5
• Echocardiographic measurement of the normalized left ventricular internal diameter in diastole (LVIDDN) > 1.7
• Echocardiographic measurement of the left atrial-to-aortic ratio (LA/Ao) >1.6
Starting with the VHS parameter of 10.5, not only do the authors fail to cite any authority for that minimum measurement, but one of the study's three lead investigators, Dr. Adrian Boswood, stated in a November 2016 audio interview (at time 31:24) that:
"A vertebral heart score of 10.5 is in the normal range for some dogs, particularly cavaliers actually."
As stunningly dismissive of the authenticity of the EPIC Study's VHS parameter as Dr. Boswood is in this quote, this is not the only mocking comment he made about its parameters in just this one interview. More to come later. One can only imagine what he may have to say about the study off-mic.
Another of the EPIC Study's three lead investigators, Dr. Sonya Gordon, wrote in a June 2017 article:
"However, given the potential low accuracy of depending solely on a radiographic VHS greater than 10.5, ... and that there are known breed-related differences in normal VHS reference ranges with much higher normal VHS ranges reported in some breeds, including the CKCS, ... ."
Note that both comments indicate the lead investigators' complete lack of concern about possibly placing our breed, the cavalier King Charles spaniel, at great risk by administering pimobendan to several CKCSs prematurely for several years. Nearly half of the 360 dogs were cavaliers.
So that amounts to two out of three lead investigators who pooh-pooh their study's own VHS parameter. (We have not heard from Dr. Haggstrom yet.) When a study's lead investigators do not control their study's inclusion parameters, you must wonder who really is in charge of the study. Could it be the sponsor?
Interestingly, the EPIC Study authors do provide a footnote at the point they announce this VHS value of >10.5, but it cites only a March 2005 study of 50 sets of heart x-rays of only one breed - ironically our breed, the cavalier King Charles spaniel - which found that a mean VHS value of 10.8 ± 0.49 in cavaliers was "normal", meaning that those dogs' hearts were not enlarged at all. So, we have the EPIC Study investigators declare that any dog with a VHS value of >10.5 must have enlargement, while citing as authority for that declaration an article which found that CKCSs with a significantly higher VHS value of 10.8 (and up to 11.29) had no enlargement at all. This is a flagrant act of citation bluffing, a ruse in which the EPIC Study authors engage more than just once. Right there is proof positive of contempt for the health and welfare of the cavalier King Charles spaniel!
On to the echo parameter of LVIDDN of 1.7. The EPIC authors attribute their LVIDDN parameter of > 1.7 to a May 2004 article which in no way states that > 1.7 signifies heart enlargement. In fact, the 2004 article does not deal with MVD at all.
Furthermore, in that same audio interview (at time 31:06) in November 2016 that is noted above, Dr. Boswood admitted that the LVIDDN of 1.7 also is below the range for enlargement. He said:
"Now interestingly, if you look in the literature, the normalized left ventricular diameter of 1.7 is in the normal range. The abnormal is above about 1.85, [1.]9, 1.9 depending upon how you read it, so that's nudging the top of the normal range but still normal."
Perhaps Dr. Boswood was referring to the normal LVIDDN range as high as 1.85 reported in this widely-cited 2004 article, in which its authors stated:
"If the result is between 1.27 and 1.85, the value is within the normal [95%] prediction interval for this study." (Emphasis added.)
So much for the "validity" of the LVIDDN measurement. Dr. Boswood has demonstrated by his own words that these inclusion parameters were never intended to bear any relationship to dogs which actually had enlarged hearts.
That leaves the LA/Ao parameter of >1.6. The EPIC Study's authors'
footnote for that choice cites a
November 2002 report of another study of
solely cavaliers, in this case 166 of them.
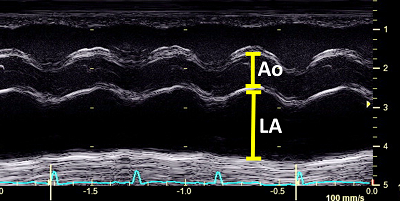 That study divided the dogs into two
groups - 56 cavaliers with no MVD and 110 cavaliers with mitral regurgitation (MR).
The study did not distinguish between MVD-affected CKCSs with and without
heart enlargement. In fact, enlargement was not even a topic of this study.
The cavaliers in the MR group had a mean LA/Ao ratio of 1.61 ± 0.57. That
range of measurements included cavaliers which had no heart enlargement at
all.
That study divided the dogs into two
groups - 56 cavaliers with no MVD and 110 cavaliers with mitral regurgitation (MR).
The study did not distinguish between MVD-affected CKCSs with and without
heart enlargement. In fact, enlargement was not even a topic of this study.
The cavaliers in the MR group had a mean LA/Ao ratio of 1.61 ± 0.57. That
range of measurements included cavaliers which had no heart enlargement at
all.
The authors of the 2002 study warned against applying these measurements for cavaliers to any other breeds, much less species-wide. They stated:
"The 2-D method can be used for any breed, but direct extrapolation of our normal values should not be made to other breeds, because the heart has a slightly different appearance in various breeds reflecting variability in size, shape, and position within the thorax."
The 2002 study's authors also were careful to exclude any findings comparing LA/Ao ratios of dogs with and without enlarged hearts. Since the 2002 article made no distinction between MVD-affected dogs with and without enlargement, that LA/Ao ratio data was irrelevant to the EPIC Study. The 2002 article authors stated:
"In this study, we have deliberately refrained from introducing index ranges for mild, moderate, and severe enlargement, because the grading would be arbitrary and was not included in the study design."
The EPIC Study authors ignore all of those cautions against applying the 2002 study's findings to any other breed. Thus, what would be "arbitrary" to the authors of the 2002 study (and therefore should be excluded) now, in the EPIC Study report, is "top tier" (as Dr. Boswood immodestly has described it in an intervew). More citation bluffing. So, again, since the EPIC Study authors did not cite any other article or data to support a minimum LA/Ao ratio of >1.6 for concluding that all dogs of all breeds had enlarged hearts, the EPIC Study authors apparently had no source for this parameter.
In addition, in that previouly referenced audio interview, Dr. Boswood raised the prospect of clinicians frequently mis-calculating the LA/Ao ratio. He said (at 30:40):
"Everyone knows you can get an inaccurate single measurement of left atrium to aortic ratio -- over-estimated. The dog goes on to treatment it didn't need."
Even more glaring is that, while the EPIC Study concludes that its minimum enrollment parameters (LA/Ao > 1.6, LVIDDN > 1.7, and VHS > 10.5) should also define enlarged hearts for prescribing Vetmedin in the future, the fact is that none of the dogs in the EPIC Study had heart measurements as low as any of those parameters. The lowest LA/Ao ratio for any dog in the EPIC Study was 1.72 (not 1.6), and the lowest LVIDDN measurement was 1.8 (not 1.7), and the lowest VHS value was 10.9 (not 10.5).
Final thoughts on the EPIC Study: Notwithstanding the fact that the EPIC Study's inclusion parameters for enlargement were really in the normal-sized heart range, the authors recommended that their parameters be followed by clinicians in determining when to start dosing pimobendan. They concluded:
"The conclusions of this study are only relevant to dogs with cardiac enlargement secondary to preclinical MMVD (stage B2) as all dogs entering the study met or exceeded 3 different heart size criteria (LA/Ao > 1.6, LVIDDN > 1.7, and VHS > 10.5) ... ."
Because the EPIC Study's inclusion criteria were irrelevant to Stage B2, and no independent, subjective determinations of heart enlargement were performed, no one will ever know how many - or if any at all - of the 360 dogs in that study had enlarged hearts when the testing commenced. All that is known for certain is that all of the dogs in the study started out somewhere in Stage B, and based upon the study's liberal inclusion criteria, many of them very well could have been Stage B1 dogs.*
Since no effort was made to determine which of the 360 dogs in the study actually had any enlargement and actually were in Stage B2, likewise no effort was made to determine how many of those Stage B2 dogs were in the pimobendan group and how many in the placebo group. Presumably it would take a dog without enlargement a significantly longer time to reach heart failure than it would a dog with enlargement. If a higher percentage of the dogs without enlargement were in the pimobendan group than in the placebo group, then the median times for the dogs to reach heart failure would be skewed and the results meaningless. This is an obvious, fundamental flaw in this so-called "top tier" study.
But the worst thing about the EPIC Study is that, since its inclusion parameters -- ipso facto -- have also become its recommended treatment protocol, many MVD-affected dogs only at Stage B1 will be prescribed pimobendan from now on.
* The incredible disconnect between the EPIC Study's inclusion parameters and dogs which may actually have had any heart enlargement makes us wonder whether these were not the original parameters selected by the lead investigators. Could they have started out with some realistic parameters which they subsequently felt the need to abandon because they had fallen several months behind their two-year recruitment phase goal to enlist 360 dogs with enlarged hearts?
The Cardiac Education Group's baseless "Recommendation" is nonsense
2. The Cardiac Education Group "Recommendation". The Cardiac Education Group
(CEG) is a team of seven board certified veterinary cardiologists in the
United States:
 Drs.
John D. Bonagura, Rebecca L. Stepien, Brian A. Scansen, Barret Bulmer, Whit
M. Church, Alan W. Spier, and Sonya G. Gordon. As noted above, Dr. Gordon is
one of the three lead investigators of the EPIC Study. Four of the other CEG
members were participating investigators in the EPIC Study.
Drs.
John D. Bonagura, Rebecca L. Stepien, Brian A. Scansen, Barret Bulmer, Whit
M. Church, Alan W. Spier, and Sonya G. Gordon. As noted above, Dr. Gordon is
one of the three lead investigators of the EPIC Study. Four of the other CEG
members were participating investigators in the EPIC Study.
In December 2016, a month after the EPIC Study report was published, the CEG, which ironically also is sponsored by a grant from Vetmedin's manufacturer, issued a "Recommendation" that EPIC's two echo parameters could be skipped. They wrote:
"If an echocardiogram is not available and only thoracic radiographs are performed, the CEG recommends starting pimobendan in dogs with heart murmurs of grade 3/6 or louder only when the VHS exceeds 11.5 vertebral bodies or an incremental increase of greater than 0.5 vertebral bodies per 6 months is accurately documented."
The CEG members go on to actually admit that their x-ray-only recommendation is not based upon the EPIC Study and is not based upon any other evidence, at all. They write:
"ACVIM guidelines recommend both imaging methods for optimal evaluation of a dog with suspected MMVD. The EPIC trial did not investigate a cutoff for cardiac enlargement by VHS alone at which to start pimobendan therapy. This algorithm represents the consensus of the CEG to initiate therapy when echocardiography is not available, but is not based on evidence." (Emphasis added.)
What nonsense! Granted, the CEG upped the minimum VHS value from > 10.5 to > 11.5, but as we have noted above, what the CEG ignores is that, for some breeds, especially the cavalier, even a VHS value of >11.5 still may mean that the heart is not enlarged at all. So, why does the CEG insist upon using a "one size fits all" set of parameters, which means that the cavalier is put at greater risk, and without any supporting evidence whatsoever? Well, CEG fails to provide any explanation.
But apparently the CEG members expect their audience of primary care vets to unquestionably accept this advice despite the fact that it is not based upon any evidence, and more importantly, despite the fact that it expressly contradicts peer-reviewed, evidence-based, published research to the contrary.
As egregious as CEG's December 2016 recommendation of using only a VHS value of > 11.5 as a species-wide minimum for prescribing pimobendan is, the group shoved the cavaliers even farther out on that risky limb in July 2017 when it issued a leaflet stating:
"Pimobendan treatment should be initiated in dogs with ... a VHS >11.5."
The CEG's July 2017 leaflet likewise provides no explanation for this recommendation. It cites no veterinary journal articles or other published research. It does not even suggest that its own unpublished research warrants such advice. The CEG just substitutes an arbitrary number - 11.5 - for any professional veterinary determination of whether the patient does or does not have an enlarged heart. CEG's sole justification that 11.5 "represents the consensus of the CEG to initiate therapy" is totally unimpressive. The use of "consensus" by the CEG is giving that word a whole new (and meaningless) meaning. "Gasbagging" comes to mind.
June 2017 article's arbitrary x-ray-only Stage B2 parameter = Stage B1
3."Asymptomatic Canine Degenerative Valve Disease: Current and Future Therapies". In this June 2017 article, EPIC Study report lead investigator Dr. Sonya G. Gordon and Drs. Ashley B. Saunders and Sonya R. Wesselowski, all cardiologists at Texas A&M University's veterinary school, advise prescribing pimobendan to pre-CHF MVD-affected dogs using only a VHS value of 11.5 to determine if the dogs' hearts are enlarged. They state:
"The EPIC inclusion criteria required both radiographic and echocardiographic evidence of cardiomegaly. The requirement for an echocardiogram may in some cases exclude the recommendation for initiation of pimobendan. However, given the potential low accuracy of depending solely on a radiographic VHS greater than 10.5, ... and that there are known breed-related differences in normal VHS reference ranges with much higher normal VHS ranges reported in some breeds, including the CKCS, it is prudent to use a higher VHS size if recommendations for treatment are based solely on history, physical examination, and thoracic radiographs. ... In addition, the median VHS of dogs in the EPIC study was approximately 11.5 ... . Use of a VHS of >11.5 will improve the specificity (positive predictive value) of significant heart enlargement and guard against overtreatment of possible stage B1 dogs." (Emphasis added.)
What these cardiologists know full well but ignore is that, for some breeds, especially the cavalier, even a VHS value of 11.5 may mean that the heart is not enlarged at all. While they describe using the species-wide 11.5 VHS value for prescribing pimobendan as "prudent" and to "guard against overtreatment of possible stage B1 dogs", in fact it is arbitrary, risky, and unsupported by any research, and they know it! So, why do they, too, insist upon using a "one size fits all" set of parameters, which means that the cavalier is put at greater risk? At the very least, they should pay attention to the advice given in the article they cite in their report's footnote 15, which expressly states:
"The use of breed-specific VHS values is needed for the VHS method to have a high specificity for normal heart size."
We would prefer using a patient-specific VHS value, rather than just breed-specific, but either one is better than a reckless, species-wide "median" VHS value.
Why the good doctors ignored this advice is perplexing. Could the reason be connected to their article's "Disclosure Statement", about two of them having "received funding from Boehringer Ingelheim Animal Health GmbH.", the manufacturer of Vetmedin?
Surely they are aware that the 2009 ACVIM Consensus Statement, of which Dr. Gordon was one of the authors, specifically emphasized the importance of obtaining baseline x-rays. Here is what they (she) wrote back in 2009:
"Diagnosis for Stage B: Consensus recommendations: Thoracic radiography is recommended in all patients to assess the hemodynamic significance of the murmur and also to obtain baseline thoracic radiographs at a time when the patient is asymptomatic for CVHD [chronic valvular heart disease]." (Emphasis added.)
Now, Dr. Gordon and her cohorts may reply by saying that, in many instances, no baseline x-rays have been taken, and it is too late now. Apart from the fact that they never mention the baseline option at all, our response to that situation is for the authors to recommend not relying solely upon a current x-ray, and to require that the dog undergo a thorough patient-specfic examination, including echocardiography. What does Dr. Gordon think "assess the hemodynamic significance of the murmur" means? As is demonstrated in some detail below, to advise primary care vets to waive echo exams for cavaliers, when there is no baseline x-ray for confirming if any enlargement has occurred, is, frankly, encouraging malpractice.
Oddly enough, we have found that, at the authors' own cardiology clinic at Texas A&M, they advise the owners of their cavalier patients to skip echocardiograms and to rely upon annual auscultations (stethoscopic examinations) and annual x-rays to detect heart enlargement instead of echos. Here is a typical paragraph included in their patient reports:
"Mitral valve disease tends to progress slowly, over the course of months to years. Monitoring for [dog's name] can involve annual auscultation (listening with a stethoscope) and chest x-rays. Consider getting [dog's name] a set of baseline chest x-rays in the near future. Then her future annual x-rays can be compared to this set. Should heart enlargement be detected in [dog's name] at some point in the future, a recheck cardiology appointment should be considered at that time."
July 2017 article's"enlargement" parameters are bogus
4. "Treatment of dogs with compensated myxomatous mitral valve disease with spironolactone--a pilot study". This new propensity for relying upon species-wide parameters for determining heart enlargement has not been limited to determining when to treat MVD with pimobendan. This article was published in July 2017 by authors M.J. Hezzell, A. Boswood, J. López-Alvarez, N. Lotter, and J. Elliott. As noted previously, Dr. Boswood also had been one of the three lead investigators in the EPIC Study.
While this July 2017 study dwelt upon another medication for MVD - spironolactone - its authors followed the lead of the EPIC Study by creating their own unique definition of enlargement of MVD-affected dogs' hearts. In this case, they stated:
"To be eligible for inclusion in the present study, a dog had to have echocardiographic evidence of MMVD, defined as above, and demonstrate at least one risk factor for disease progression (evidence of cardiomegaly, defined as left atrial to aortic ratio, [LA:Ao] > 1.5 and/or left ventricular end-diastolic dimension, normalized for body weight [LVIDdN]) > 1.6, ... .." (Emphasis added.)
Note that they specifically "defined" cardiomegaly (vet-speak for heart enlargement). It included:
• LA:Ao > 1.5 and/or
• LVIDdN > 1.6.
As for the LA:Ao threshold of 1.5, that is even lower than the bogus 1.6 minimum in the EPIC Study. In this instance, however, the authors cite a different authority for that parameter. Here they cite a July 2000 report. But, that article provides no justification for concluding that an LA:Ao ratio of 1.5 means that the dog's heart is enlarged. In that July 2000 report, the investigators studied only dogs with normal hearts. They found dogs with normal sized hearts with LA/Ao ratios as high as 1.59, which is higher than this July 2017 article's arbitrary minmum measurement of 1.5 for dogs with enlarged hearts. They also stated:
"Finally, we have not examined dogs with left-heart disease. However, even in dogs with left-heart disease, atria that measure within the limits we have described would be considered normal sized. Further studies in dogs with left-heart disease are needed to qualify degrees of LA enlargement."
So, once again, the article cited to justify the criterion provides no justification at all. In this case, it expressly contradicts the measurement which the July 2017 authors intended that it support.
Turning to the July 2017 article's threshold LVIDdN > 1.6, we already know
what Dr. Boswood really thinks about that LVDdN measurement.
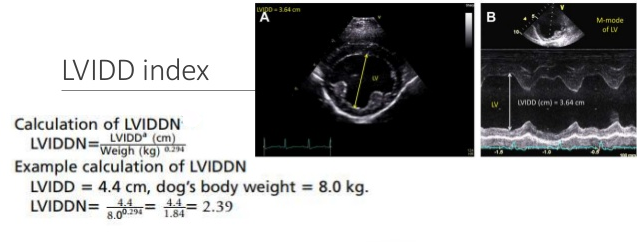 It is smack in
the normal heart-size range. To repeat, he
said this about an even higher enlargement threshold measurement, 1.7:
It is smack in
the normal heart-size range. To repeat, he
said this about an even higher enlargement threshold measurement, 1.7:
"Now interestingly, if you look in the literature, the normalized left ventricular diameter of 1.7 is in the normal range. The abnormal is above about 1.85, [1.]9, 1.9 depending upon how you read it, so that's nudging the top of the normal range but still normal."
From these contradictory citations, we can see a pattern of using footnoted citations as meaningless window-dressing. To the extent that actual heart enlargement was relevant to this testing of spironolactone, the researchers wasted their time.
October 2017 article's definition of "enlargement" is fictitious
5. "Angiotensin-converting enzyme activity and inhibition in dogs with cardiac disease and an angiotensin-converting enzyme polymorphism". In an October 2017 article, a team of mostly USA cardiologists (Kathryn M. Meurs, Joshua A. Stern, Clarke E. Atkins, Darcy Adin, Brent Aona, Julia Condit, Teresa DeFrancesco, Yamir Reina-Doreste, Bruce W. Keene, Sandy Tou, Jessica Ward, Kathleen Woodruff) report the results of a study of angiotensin-converting enzyme (ACE) activity in dogs with mitral valve disease. Of 31 MVD-affected dogs, including 10 cavalier King Charles spaniels, 11 dogs (6 CKCSs) were found to have a variant (single nucleotide polymorphism) of the intron 16 gene, which is associated with ACE activity in MVD-affected dogs. The ACE polymorphism was most common in the cavalier. They found that, before any ACE-inhibitor treatment, median ACE activity was significantly lower for ACE polymorphism dogs than in the control group. However, following treatment with enalapril, ACE activity was significantly reduced in both groups. They conclude:
"An ACE polymorphism is associated with lower levels of ACE activity. Dogs with the polymorphism still experience suppression of ACE activity in response to an ACE inhibitor. It is possible that the genetic status and ACE activity of dogs may impact the response of dogs with this variant to an ACE inhibitor."
Whether the presence of heart enlargement in these dogs was meaningful to the researchers or not, we also notice that they state that:
"All dogs were required to have a grade 4/6 left apical systolic murmur and radiographically evident cardiac enlargement (defined as a vertebral heart scale (VHS) >11)." (Emphasis added.)
While they cite two footnoted publications at the end of that sentence, presumably to justify their selection of a minimum VHS parameter of 11.0 as their arbitrary, species-wide "definition" for heart enlargement, neither of those cited articles support the selection of that VHS value. In fact, the cited articles do not support the selection of any vertebral heart scale values, at all.
Interestingly, the first of the two cited articles stated that the study's means of determining if the dogs had enlarged hearts was to carefully examine x-rays of the dogs' hearts - a previously routine veterinary procedure which this October 2017 study's cardiologists seem intent to avoid. The authors of the cited article stated:
"Thoracic radiographs in left lateral and ventrodorsal projections were made for all dogs. All radiographs were evaluated for signs of cardiomegaly [heart enlargement]... . The radiographic examinations were reviewed at annual evaluation meetings to ensure uniform film readings."
The second of the two articles cited in this October 2017 report as justification for the VHS value of >11 does not even discuss that topic.
So, in this October 2017 article, we have several board certified veterinary cardiologists intentionally failing to determine if the dogs' hearts actually are enlarged and instead artificially defining heart enlargement by an arbitrary minimum VHS value. If they had peer-reviewed, published evidence that a VHS value of 11.0 is conclusive proof that all dogs of all species with at least that VHS value had enlarged hearts, surely they would have cited those publications. They have cited nothing of the sort. As a result, the researchers in this article were flying blind when it came to whether the dogs' hearts were enlarged or not. They ended up studying the VHS measurement instead of heart enlargement. So, to the extent that heart enlargement was an important factor in this study, the researchers failed to make that determination.
September 2017 abstract's data prove the other studies' parameters are farcical
6. "Utility of VHS to Predict Echocardiographic EPIC Trial
Inclusion Criteria in Dogs with Myxomatous Mitral Valve Disease: a
Retrospective Multicentre Study".
 In this
September 2017 abstract presentation to the European Society of
Veterinary Internal Medicine's 27th ECVIM-CA Congress in Malta, a group
of USA cardiologists (J.P. Vitt, S. Gordon, R.C. Fries, J.D. Rhinehart,
S.E. Achen, I. Sosa, A.H. Estrada, J.A. Carlson, R.L. Winter, S.
Kadotani, K.E. Lamb) examined the radiographic and echocardiographic records
of 247 MVD-affected dogs at 8 locations to attempt to identify a minimum
VHS value that would also predict EPIC's
echocardiography inclusion criteria without having to perform
echocardiographic examinations. They report that of the 247 dogs which
met EPIC's minimum VHS value of 10.5, only 126 (51%) met EPIC's two
minimum echo parameters (LVIDDN >1.7 and LA:Ao >1.6). They found that
MVD-affected dogs with a VHS > 11.7 had an 85% likelihood of also
meeting the echo parameters, and that roughly 34% of dogs with VHS
values between 10.6 and 11.7 may meet those two echo measurements. They
conclude:
In this
September 2017 abstract presentation to the European Society of
Veterinary Internal Medicine's 27th ECVIM-CA Congress in Malta, a group
of USA cardiologists (J.P. Vitt, S. Gordon, R.C. Fries, J.D. Rhinehart,
S.E. Achen, I. Sosa, A.H. Estrada, J.A. Carlson, R.L. Winter, S.
Kadotani, K.E. Lamb) examined the radiographic and echocardiographic records
of 247 MVD-affected dogs at 8 locations to attempt to identify a minimum
VHS value that would also predict EPIC's
echocardiography inclusion criteria without having to perform
echocardiographic examinations. They report that of the 247 dogs which
met EPIC's minimum VHS value of 10.5, only 126 (51%) met EPIC's two
minimum echo parameters (LVIDDN >1.7 and LA:Ao >1.6). They found that
MVD-affected dogs with a VHS > 11.7 had an 85% likelihood of also
meeting the echo parameters, and that roughly 34% of dogs with VHS
values between 10.6 and 11.7 may meet those two echo measurements. They
conclude:
"These results may help veterinarians apply the results of the EPIC Trial to dogs with preclinical MMVD when an echocardiogram is not readily available."
Imagine that! Not even a VHS value of 11.7 will predict heart enlargement 100% of the time! This study unintentionally highlights the fact that the EPIC Study's inclusion criteria are fatally flawed and put some MVD-affected dogs, particularly cavaliers, at greater risk of suffering the harmful effects which pimobendan has been shown to cause in some instances of its premature administration.
If we assume (an assumption which already has been disproven) that EPIC's two echo parameters will always predict heart enlargement regardless of breed, then this study tells us that if the clinician relies only upon an x-ray showing a VHS value of >11.7, then 15% of the dogs still will not have enlarged hearts. It also proves that there can be no such thing as a species-wide minimum measurement for heart enlargement, without forcing dogs with normally smaller hearts to have to reach enlargement measurements so big that they would practically guarantee the dogs' deaths before being treated.
Like putting lipstick on a pig, here we have one of the EPIC Study three lead investigators - Dr. Sonya Gordon - and a few other cardiologists trying to salvage the study's totally discredited parameters from the trash heap. What they are telling us is that MVD-affected dogs with an VHS value above 11.7 have a better than average chance of also having echo measurements within the range of the EPIC Study's echo parameters. And, they report that dogs with VHS values from 10.6 to 11.7 have a much worse than average likelihood of meeting those echo minimums.
What this study shows with certainty is that the EPIC Study parameters do not equate to heart enlargement and were never intended to. Furthermore no effort was made either in the EPIC Study trial or in this reported retrospective file review, to determine if any of the dogs actually had enlarged hearts. All that these cardiologists are doing is measuring distances within the dogs' hearts. Those measurements do not mean the dogs' hearts are enlarged. As noted previously, enlargement means that the size of the heart has gotten bigger over time. One set of measurements on a single day does not tell the clinician that the dog's heart is enlarged, because the clinician does not know whether or not the heart ever was smaller than it is on the single day it was measured.
There are - as there have been, for decades in the field of veterinary cardiology - professional ways to accurately determine if an MVD-affected dog's heart is enlarged or not. As noted above, examples include (a) careful examination of x-rays showing the shape of the dog's heart, with emphasis upon the left atrium and left ventricle, looking for bulges and roundness; (b) comparison of current x-rays with earlier baseline x-rays. That professionalism is one of the reasons board certified veterinary cardiologists are board certified. For some inexplicable reason, the EPIC Study investigators and the authors of this report do not want have to bother to perform that professional veterinary service. They prefer to urge primary care veterinarians to rely upon arbitrary measurements which this report proves are not reliable, and end up putting our cavaliers at risk by prematurely prescribing pimobendan, a drug which as been shown to rapidly accelerate the progression of MVD in dogs which do not yet need it.
We can only imagine how much pressure some hidden force must be putting upon these cardiologists for them to waive their professionalism and contort their brains to come up with a way to enable more primary care veterinarians to prescribe more Vetmedin pills to dogs which may, but very likely would not, need those pills.
Conclusion: large hearts ≠ enlarged hearts
CONCLUSION: (a) These arbitrary echo and x-ray parameters do not measure heart enlargement. If heart enlargement - meaning MVD-dogs in ACVIM Stage B2 - is an important aspect of these six research articles, then these arbitrary parameters make the results of the research worthless, because there can be no assurance that any of the dogs in the studies really had enlarged hearts.
(b) Only article #6 bases its minimum VHS value upon any evidence. Notice that in four of the articles before #6, the authors confidently tell us that their minimum VHS value equates with enlargement. In #1, it is >10.5. In #2 and #3, it is 11.5. In #5, it is 11.0. All of those unsubstantiated VHS values are low ball figures. Article #6 at least has attempted to back up its VHS value with documentation, and (Surprise! Surprise!) that value is >11.7! Does this mean the authors of the other articles are going to revise their now totally discredited advice? We doubt it.
(c) A current set of chest x-rays without a baseline set is asking for trouble. In each of these five recent examples of relying upon arbitrary species-wide VHS measurements, what is most disturbing is that the cardiologists do not acknowledge the dirty little secret about primary care veterinarians: many of them cannot determine whether a dog's heart is enlarged or not, simply by looking at one set of x-rays.
Even experienced board certified cardiologists will argue over whether a single set of x-rays (they call them "chest rads") shows left atrium enlargement or not, and if so, its degree. This usually is due to poor positioning of the dog during the x-rays, which is not uncommon. See e.g., "Why Is Cardiac Radiology So Difficult?" by Dr. Christopher R. Lamb. He wrote:
"In a recent study two experienced observers examined the radiographs of 57 dogs with common congenital cardiac anomalies without access to any clinical information in order to avoid biasing their interpretations. Under these conditions, the observers reached the correct diagnosis in less than 40% cases. This poor result reflects the difficulty observers had identifying shape changes that can occur in radiographs of dogs with enlarged cardiac chambers. Radiographic signs of specific cardiac chamber enlargement (or pulmonary vascular abnormalities) were recognised by both observers in only 20% instances in which they might be expected."
As a result, primary care vets - and even some cardiologists - often tend to find enlargement when there really is none at all. When that leads to prematurely prescribing pimobendan, severe heart damage can occur, based upon prior peer-reviewed studies. To remedy this hazard, all they had to do was also recommend that the primary care vets make baseline x-rays of their MVD patients before any enlargement takes place, so that the vet will be able to compare the normal size of the patient's heart in the baseline x-ray to the later x-ray which may (or may not) show enlargement. This is what we mean by using a patient-specific VHS value.
Granted, even with baseline x-rays for comparison purposes, relying upon the x-rays alone and their VHS values only tell the clinician that the heart as a whole is enlarged, and not whether the left atrium (LA) and/or the left ventricle (LV) are enlarged. Maybe a board certified cardiologist can tell from x-rays (rads) alone that the LA or LV is enlarged, but as we noted above, even they will disagree from time to time, and especially if the positioning of the dog (even flexing the neck can cause misleading shadowing) and quality of the films are less than perfect, or the dog was inhaling in one view and exhaling in another or sedated in one and not in the other. This list could go on and on.
(d) Summary: The most disturbing thing about these echo and x-ray parameters for enlarged hearts, is that the authors had to know that their minimum measurements were fictitious. As an example, Dr. Boswood confessed that two of the three parameters for the EPIC Study were for normal-sized hearts, and that the third one was prone to frequent over-estimations. In none of the first five articles did the authors provide a single citation to any previous published research which substantiated the choices. Instead, in some cases they seem to have tried to mislead readers into thinking such authorities exist by citing articles which were either irrelevant to the parameters or expressly contradicted them.The CEG even admitted that its recommendation "is not based on evidence."
It clearly appears that as far as administering pimobedan to MVD-affected dogs is concerned, the researchers authoring articles ##1, 2, 3, and 6 are not the least bit concerned about including Stage B1 dogs in that category. If a lack of heart enlargement really disturbed their consciences (as well it should), they surely would have drafted their recommendations much, much more cautiously.
The nature of specialized veterinary cardiology care used to emphasize individualized diagnosis and treatment. But if these six articles are in any way representative of the current state of cardiology, the nature has become an intellectually lazy, cookie-cutter style of practice.
Why? Why? Why?
The questions remain:
• Why are they doing this?
• Why do they even attempt to define heart enlargement on a species-wide basis without first performing any research to determine what that definition should be?
RETURN TO TOP
October 21, 2017:
The EPIC Study's three heart "enlargement" parameters are arbitrary and unsupported by their cited authorities!
EPIC's investigators treated heart size instead of heart enlargement
 The
EPIC Study trial, which was sponsored by Vetmedin's manufacturer, Boehringer
Ingelheim Vetmedica, Inc., allegedly concludes that Vetmedin (generic name:
pimobendan) could be prescribed to any dog affected with mitral valve
disease (MVD) if the left atrium and left ventricle of the dog's heart are
enlarged. But that was not the real conclusion of
the EPIC Study report, published in November 2016.
The
EPIC Study trial, which was sponsored by Vetmedin's manufacturer, Boehringer
Ingelheim Vetmedica, Inc., allegedly concludes that Vetmedin (generic name:
pimobendan) could be prescribed to any dog affected with mitral valve
disease (MVD) if the left atrium and left ventricle of the dog's heart are
enlarged. But that was not the real conclusion of
the EPIC Study report, published in November 2016.
What the report really concluded was that pimobendan could be prescribed if the MVD-affected dog's heart size met a set of three minimum measurements, regardless of whether the dog's heart actually was enlarged. Two of those measurements were determined from an echocardiograph examination:
(1) the left atrial-to-aortic ratio (LA/Ao) equal to or greater than (>) 1.6; and
(2) the normalized left ventricular internal diameter in diastole (LVIDDN) > 1.7.
The third measurement, taken from x-rays of the dog's heart, was a vertebral heart score (VHS) greater than (>) 10.5.
Those three measurements were the parameters for including MVD-affected dogs in the study, and they also became the recommended parameters for treating dogs with pimobendan in the study's conclusion.
The Study's initial "enrollment criteria" were:
"To be eligible for inclusion, a dog had to ... have echocardiographic evidence of left atrial and left ventricular dilatation, defined as a left atrial-to-aortic root ratio (LA/Ao) > 1.6 and body weight normalized left ventricular internal diameter in diastole (LVIDDN) > 1.7, in addition to radiographic evidence of cardiomegaly (vertebral heart sum (VHS) > 10.5)."
And the final recommended parameters remained the same:
"The conclusions of this study are only relevant to dogs with cardiac enlargement secondary to preclinical MMVD (stage B2) as all dogs entering the study met or exceeded 3 different heart size criteria (LA/Ao > 1.6, LVIDDN > 1.7, and VHS > 10.5) ... ."
Now, considering that the premise of the EPIC Study was to determine whether dogs with enlarged hearts due to MVD should be treated with pimobendan, one would likely assume that those three parameters - LA/Ao > 1.6; LVIDDN > 1.7; VHS >10.5 - necessarily meant that the hearts of all 360 dogs in the study were, in fact, enlarged. Unfortunately, that assumption would be false.
The fact is that none of the dogs in the EPIC Study had heart measurements as low as any of those parameters. The lowest LA/Ao ratio for any dog in the EPIC Study was 1.72 (not 1.6), and the lowest LVIDDN measurement was 1.8 (not 1.7), and the lowest VHS value was 10.9 (not 10.5).
Footnotes to EPIC's parameters are meaningless window-dressing
It is not just customary, but really professionally mandatory, that when veterinary researchers select a particular measurement as the minimum or maximum parameter for qualifying candidate dogs for a study of a new medication (or the new application of an existing drug), the researchers state their reasoning for choosing that measurement and cite the prior published authorities for relying upon it.
In the EPIC Study report, each of the parameters has a footnoted citation to a single previous veterinary research article, leading the reader to assume that the cited article in the footnote for each parameter surely must more than adequately support the EPIC Study investigators' selection of that specific parameter as conclusively establishing heart enlargement, species-wide. But alas, none of the cited articles provide any such support at all. It is as if the footnotes are simply meaningless window dressing to make the selection of parameters look like some peer-reviewed, published research actually exists to warrant them. This is known as citation bluffing.
VHS > 10.5 - For example, the Study's species-wide x-ray parameter of the vertebral heart score (VHS), "radiographic evidence of cardiomegaly (vertebral heart sum (VHS) > 10.5)" is attributed only to a March 2005 article of a study of 50 sets of heart x-rays of only one breed - ironically our breed, the cavalier King Charles spaniel - and found that a mean VHS value of 10.8 ± 0.49 in cavaliers was "normal", meaning that those dogs' hearts were not enlarged at all. So, we have the EPIC Study investigators declare that any dog with a VHS value of >10.5 must have enlargement, while citing as authority for that declaration an article which found that CKCSs with a significantly higher VHS value of 10.8 (and up to 11.29) had no enlargement at all. The authors of the cited 2005 article ironically stated:
"The mean VHS for normal cavalier King Charles spaniels was 10.8 ± 0.49 v (10.0-11.4). ... The use of breed-specific VHS values is needed for the VHS method to have a high specificity for normal heart size. ... The VHS values for heart size can be affected by several factors. Individual variations in actual heart size and vertebral length between dogs need to be considered as well as narrowed disc spaces."
Since the EPIC Study authors did not cite any other article or data to support a minimum VHS value of >10.5, they apparently had no better source for this parameter, which in this case means they had no justification whatsoever for choosing >10.5 as being conclusive VHS evidence of enlargement for all breeds. Not only that, but the 2005 article concludes by emphasizing the importance of using breed-specific VHS values, and even individual dog variations in heart size and vertebral length, in order for the VHS method to work at all - two things that the EPIC Study investigators clearly never had any intention of taking into account.
Not only that, but we find that the EPIC Study's lead investigator, Dr. Adrian Boswood, admitted in a November 2016 audio interview (at time 31:24) that:
"A vertebral heart score of 10.5 is in the normal range for some dogs, particularly cavaliers actually."
As stunningly dismissive of the authenticity of the EPIC Study's VHS parameter as Dr. Boswood is in this quote, this is not the only mocking comment he made about its parameters in just this one interview. More to come later. One can only imagine what he may have to say about the study off-mic.
Another of the EPIC Study's three lead investigators, Dr. Sonya Gordon, wrote in a June 2017 article:
"However, given the potential low accuracy of depending solely on a radiographic VHS greater than 10.5, ... and that there are known breed-related differences in normal VHS reference ranges with much higher normal VHS ranges reported in some breeds, including the CKCS, ... ."
Note that both comments indicate the lead investigators' complete lack of concern about possibly placing our breed, the cavalier King Charles spaniel, at great risk by administering pimobendan to several CKCSs prematurely for several years. Nearly half of the 360 dogs were cavaliers.
So that amounts to two out of three lead investigators who pooh-pooh their study's own VHS parameter. (We have not heard from Dr. Haggstrom yet.) When a study's lead investigators do not control their study's inclusion parameters, you must wonder who really is in charge of the study. Could it be the sponsor?
Dr. Anna Beber tidily sums up this emperor-has-no-clothes situation in her March 2018 master's thesis when she writes:
"Using the vertebral heart score cut off of 10.5v in the EPIC study, all of the 'normal' Cavalier King Charles Spaniels in this study (defined by subjective impression consensus opinion) would have been considered to have cardiomegaly and therefore potentially received treatment unnecessarily. ... Therefore, to ensure that a VHS is of value, the author suggests that large numbers of breed 'normals' need to be used to establish a more reliable reference range."
Why would 36 board certified veterinary cardiologists choose a species-wide VHS parameter of > 10.5 for enlarged hearts, while knowing that some breeds have normal hearts with substantially higher VHS values?
LA/Ao > 1.6 -The EPIC Study's authors attribute their choice of the "left atrial-to-aortic root ratio (LA/Ao)" parameter of > 1.6 to a November 2002 article. Ironically, again, this reports a study of solely cavaliers, in this case 166 of them. It divided the dogs into two groups - 56 dogs with no MVD and 110 dogs with mitral regurgitation (MR). The study did not distinguish between MVD-affected CKCSs with and without heart enlargement. In fact, enlargement was not even a topic of this study. The cavaliers in the MR group had a mean LA/Ao ratio of 1.61 ± 0.57. That range of measurements included cavaliers which had no heart enlargement at all.
The authors of the 2002 study warned against applying these measurements for cavaliers to any other breeds, much less species-wide. They stated:
"The 2-D method can be used for any breed, but direct extrapolation of our normal values should not be made to other breeds, because the heart has a slightly different appearance in various breeds reflecting variability in size, shape, and position within the thorax."
The 2002 study's authors also were careful to exclude any findings comparing LA/Ao ratios of dogs with and without enlarged hearts. Since the 2002 article made no distinction between MVD-affected dogs with and without enlargement, that LA/Ao ratio data was irrelevant to the EPIC Study. The 2002 article authors stated:
"In this study, we have deliberately refrained from introducing index ranges for mild, moderate, and severe enlargement, because the grading would be arbitrary and was not included in the study design."
The EPIC Study authors ignore all of those cautions against applying the 2002 study's findings to any other breed. Thus, what would be "arbitrary" to the authors of the 2002 study (and therefore should be excluded) now, in the EPIC Study report, is "top tier" (as one of the EPIC Study authors immodestly has described it). So, again, since the EPIC Study authors did not cite any other article or data to support a minimum LA/Ao ratio of > 1.6 for concluding that all dogs of all breeds had enlarged hearts, the EPIC Study authors apparently had no better source for this parameter.
In addition, in that previouly referenced audio interview, Dr. Boswood raised the prospect of clinicians frequently mis-calculating the LA/Ao ratio. He said (at 30:40):
"Everyone knows you can get an inaccurate single measurement of left atrium to aortic ratio -- over-estimated. The dog goes on to treatment it didn't need."
Why would 36 board certified veterinary cardiologists choose a species-wide LA/Ao ratio parameter of > 1.6 for enlarged hearts, without being able to cite any authorities for that parameter?
LVIDDN > 1.7 - The EPIC authors attribute their "body weight normalized left ventricular internal diameter in diastole (LVIDDN)" parameter of > 1.7 to a May 2004 article which in no way states that > 1.7 signifies heart enlargement. In fact, the 2004 article does not deal with MVD at all. This is the weakest citation of all three.
In that same audio interview (at time 31:06) in November 2016 that is noted above, Dr. Boswood admitted that the LVIDDN of 1.7 also is below the range for enlargement. He said:
"Now interestingly, if you look in the literature, the normalized left ventricular diameter of 1.7 is in the normal range. The abnormal is above about 1.85, [1.]9, 1.9 depending upon how you read it, so that's nudging the top of the normal range but still normal."
Perhaps Dr. Boswood was referring to the normal LVIDDN range as high as 1.85 reported in this widely-cited 2004 article, in which its authors stated:
"If the result is between 1.27 and 1.85, the value is within the normal [95%] prediction interval for this study." (Emphasis added.)
EPIC lead investigator Sonya Gordon made a similar admission in a 2017 article when she and her co-authors wrote:
"In addition, all dogs with stage B2 MMVD were required to have a left ventricular internal dimension (LVID) in diastole normalized to body weight 1.7. The selected cutoff value for normalized LVID in diastole was based on a study that found higher values, although technically within the normal reported range (<1.85), predicted increased risk of death in dogs with MMVD." (Emphasis added.)
So, to Dr. Gordon, Stage B2 has nothing to do with heart enlargement.
So much for the "validity" of the LVIDDN measurement. Drs. Boswood and Gordon have demonstrated by their own words that these inclusion parameters were never intended to bear any relationship to dogs which actually had enlarged hearts.
Why would 36 board certified veterinary cardiologists choose a species-wide LVIDDN parameter of > 1.7 for enlarged hearts, while knowing that 1.7 is in the normal range?
Since none of the citations relied upon by the EPIC Study investigators in fact support the three minimum parameters they have selected, we must wonder whether any of them even bothered to read the articles they have cited.* In short, it appears that these three parameters were just concocted arbitrarily.
*Interestingly, however, the three irrelevant veterinary journal articles have one thing in common. One of the EPIC Study lead investigators is listed as an author of all three articles.
Yes, 36 cardiologists could be very, very wrong!
Did any of the 36 EPIC Study investigators - all purportedly being board certified veterinary cardiologists - perform any subjective analysis to verify whether the participating dogs actually had enlarged hearts? In other words, did they follow the traditional, professional routine of thoroughly examining the x-rays, as a cardiac specialist would be expected to, and with their experienced eyes look for the classic signs of enlargement - cardiomegaly or dilatation - such as the shape of the left atrium, or the overall cardiac appearance, or the appearance of the vascular structures? Apparently not. They certainly did not state as much in their report.
You see, the EPIC Study authors carefully worded the "enrollment criteria" by creatively defining "dilatation" (vet-speak for "enlargement") using their three sham parameters:
"To be eligible for inclusion, a dog had to ... have echocardiographic evidence of left atrial and left ventricular dilatation [enlargement], defined as a left atrial-to-aortic root ratio (LA/Ao) > 1.6 and body weight normalized left ventricular internal diameter in diastole (LVIDDN) > 1.7, in addition to radiographic evidence of cardiomegaly (vertebral heart sum (VHS) > 10.5)." (Emphasis added.)
The irony of that quote is that, based upon the prior published research specifically cited and footnoted by the EPIC Study investigators, many dogs - especially CKCSs - with those measurements would not have enlarged hearts, because none of those three measurements assure that the dogs' hearts would in fact be enlarged.
Because the EPIC Study's inclusion criteria were irrelevant to Stage B2, and no independent, subjective determinations of heart enlargement were performed, no one will ever know how many - or if any at all - of the 360 dogs in that study had enlarged hearts when the testing commenced. All that is known for certain is that all of the dogs in the study started out in Stage B, and based upon the study's liberal inclusion criteria, many of them very well could have been Stage B1 dogs.
Since no effort was made to determine which of the 360 dogs in the study actually had any enlargement and actually were in Stage B2, likewise no effort was made to determine how many of those Stage B2 dogs were in the pimobendan group and how many were in the placebo group. Presumably it would take a dog without enlargement a significantly longer time to reach heart failure than it would a dog with enlargement. If a higher percentage of the dogs without enlargement were in the pimobendan group than in the placebo group, then the median times for the dogs to reach heart failure would be skewed and the results meaningless. This is an obvious, fundamental flaw in this so-called "top tier" study.
But the worst thing about the EPIC Study is that, since its inclusion parameters have also become its recommended treatment protocol, many MVD-affected dogs only at Stage B1 will be prescribed pimobendan from now on.
Frankly, the very notion of trying to establish a set of species-wide echo and x-ray minimum measurements for enlarged hearts is patently nonsensical, unless the minimums are so high as to severely prejudice breeds with smaller hearts. We adhere to the old fashioned concept of determining whether an individual dog's heart is normal or enlarged based upon comparison of baseline and current measurements of only that dog's heart, and the cardiologist's subjective analysis of the change in shape of the dog's left atrium and ventricle. That's what cardiologists are supposed to be doing to earn the big bucks.
There are several peer-reviewed veterinary journal articles telling us that, at the very least, breed-specific x-ray measurements are necessary (such as the March 2005 article cited in the EPIC Study report), and other such articles telling us that establishing species-wide echo index ranges for enlarged hearts would be inappropriately arbitrary (such as the November 2002 article cited in the EPIC Study report). If any of the 36 cardiologists had bothered to read those two articles which they, themselves, included in footnotes in their own article, they would have recognized the folly of their three species-wide parameters from the outset.
EPIC's dogs may or may not have had enlarged hearts
So, what the EPIC Study really tells us is that this "top tier" study was cobbled together in as superficial and unscientific a manner as possible, to gather 360 MVD-affected dogs which may - or may not - have enlarged hearts. We still cannot tell that from the published data. "Pseudo-science" is defined as the assertions of alleged scientific data but which are unsupported by empirical evidence. By any standard, the definition of an enlarged heart in this study is a textbook example of pseudo-science.
Interestingly, EPIC Study lead investigator Dr. Boswood commented on the importance of the accuracy of the "inclusion" parameters. In a May 2017 article, he wrote:
"In order to be enrolled to a study, patients usually need to meet a number of specific criteria; these are often referred to as inclusion and exclusion criteria. The purpose of these criteria is to establish that the enrolled patients definitely have the disease of interest at an appropriate stage. In order to show that they meet these criteria patients need to undergo a series of diagnostic tests before inclusion in the trial." (Emphasis added.)
Compare that statement to these admissions he had made about the EPIC Study inclusion parameters in the November 2016 interview noted above:
"A vertebral heart score of 10.5 is in the normal range for some dogs, particularly cavaliers actually."
"Now interestingly, if you look in the literature, the normalized left ventricular diameter of 1.7 is in the normal range. The abnormal is above about 1.85, [1.]9, 1.9 depending upon how you read it, so that's nudging the top of the normal range but still normal."
He went on in his May 2017 article to specifically refer to those inclusion parameters of the EPIC Study trial:
"To illustrate this point with a current example - in order to ensure that the patients recruited to the EPIC study definitely had primary mitral valve disease and enlargement of their heart they underwent both echocardiography and radiography before study entry. If I am now asked by a practitioner - 'should I treat this dog, which I believe has preclinical mitral valve disease, with pimobendan?' - my response will typically be 'to be certain that therapy is indicated the dog will need to undergo echocardiography and ideally also radiography.' Had the dogs in the study not undergone those tests our results would have been (justifiably) doubted by our peers because the severity of the recruited dogs' heart disease would not have been known ... ." (Emphasis added.)
In a June 2022 article, Dr. Mark Rishniw and Dr. Donald J. Brown concluded that the EPIC definition (LVIDDN > 1.7) was "arbitrarily chosen", and they single out five specific breeds, including the CKCS, as having larger LVs than average dogs of similar size. They state:
"The EPIC study employed an essentially arbitrary value of LVIDDN to dogs subsequently randomized to treatment with pimobendan or placebo and showed that dogs with LVIDDN>1.7 (and LA:Ao>1.6 and a VHS>10.5V) generally do better with the drug than without. ... The criterion for left ventricular enlargement used by the EPIC investigators for study inclusion has never been critically evaluated as indicative of left ventricular enlargement. ...
"We should note, however, that the definition of LV enlargement proposed by ... the EPIC trial ... is not a reference value, but a somewhat arbitrarily chosen threshold for inclusion in the EPIC trial. Therefore, clinicians adhering to these guidelines should be cautious in ascribing LVIDDN that exceed the threshold value of 1.7 as being indicative of LV enlargement.
Drs. Rishniw and Brown warn that such breeds as the CKCS "likely require breed-specific reference intervals for LVIDDN to correctly identify left ventricular enlargement." They also point out:
"For example, if a dog has a LVIDDN that consistently oscillates around 1.3 (within 0.1 units), an increase to 1.6 could indicate left ventricular enlargement for that dog, despite being within the population-based reference interval."
Well, in the EPIC Study, due to the
lack of any inclusion criteria relevant to heart enlargement, the peers have
every reason to justifiably doubt its results. Perhaps we can chalk these
oversights up to the fact that the manufacturer of Vetmedin funded and
spearheaded the entire study. Whatever the reason, this is but one more piece of evidence that the EPIC Study report
is a pathetic example of veterinary research, and it needs to be retracted, thoroughly re-analyzed, and then re-written. Its
current rendition is inexcusable, and the 36 cardiologists should be
embarrassed to have their names associated with it.
RETURN TO TOP
September 19, 2017:
Telemedicine is the answer,
when no cardiologist is nearby
Only board certified veterinary cardiologists
should treat
MVD-affected cavaliers
 Does
your dog have a heart murmur? Do you wonder whether your dog has mitral
valve disease? Do you think your dog may have an enlarged heart or symptoms
of heart failure?
Does
your dog have a heart murmur? Do you wonder whether your dog has mitral
valve disease? Do you think your dog may have an enlarged heart or symptoms
of heart failure?
We repeatedly warn all owners of cavalier King Charles spaniels to not rely upon general practice (GP) veterinarians to diagnose mitral valve disease (MVD) and to never allow GPs to prescribe medications such as pimobendan to CKCSs suspected of having MVD. Instead, we always recommend that only veterinary specialists - preferably board certified veterinary cardiologists - diagnose heart enlargement and heart failure in MVD-affected dogs.
A July 2016 study compared the survival times of MVD-affected dogs treated solely by primary care veterinarians with the survival times of MVD-affected dogs treated in collaboration by primary care vets and board certified cardiologists. The researchers found that dogs which received colaborative care had a median survival time of 254 days, while dogs treated only by primary care vets had a median survival time of 146 days.
But what if you and your dog live in a remote, rural area of the country, or, worse yet, you live in a country where there are no cardiologists or other internal medicine specialists, at all?
There is a solution. If there is no veterinary cardiologist close enough for an office visit, tell your general practice veterinarian to consult with a cardiologist by telemedicine. There are dozens of board certified veterinary cardiologists available by telephone, email, Internet video, and digital connections. They can review your dog's x-rays and echocardiography files on their computer screens while on the telephone with your dog's GP veterinarian. They even can guide your vet's hand as he moves the ultrasound transducer over your dog's heart.
And, these specialists are just a telephone call away from your GP vet.
So, if and when the time comes that your vet thinks your dog's heart murmur is getting louder, or he thinks the x-rays show enlargement of the heart, tell him to consult with a cardiologist by telemedicine. The bottom line is to never allow a GP vet to prescribe medicine to treat MVD, and the solution is for the vet to consult with a cardiologist by telemedicine.
Here is a list of telemedicine websites which offer veterinary cardiology consultation services:
Worldwide Veterinary Cardiology Telemedicine Websites
• IDEXX •
• Institute of Veterinary Specialists •
• PetRays •
•
VIN.com •
•
CardioVet •
• VitalRads •
RETURN TO TOP
September 14, 2017:
Cardiac Education Group doubles down on prescribing Vetmedin (pimobendan) to dogs without enlarged hearts
CEG recommends pimobendan if the dog's x-ray VHS value is 11.5
and
regardless of any heart enlargement
CEG admits it's species-wide VHS 11.5 value parameter
is without any scientific
support
CEG admits it is sponsored by Vetmedin's manufacturer
The Cardiac Education Group (CEG), a panel of seven veterinary
cardiologists (Drs. John D. Bonagura,
 Rebecca L. Stepien, Brian A. Scansen,
Barret Bulmer, Whit M. Church, Alan W. Spier, and Sonya G. Gordon -- left to
right), is sponsored by Vetmedin's manufacturer, Boehringer Ingelheim
Vetmedica, Inc.
Rebecca L. Stepien, Brian A. Scansen,
Barret Bulmer, Whit M. Church, Alan W. Spier, and Sonya G. Gordon -- left to
right), is sponsored by Vetmedin's manufacturer, Boehringer Ingelheim
Vetmedica, Inc.
The CEG has issued a July 2017 leaflet advising clinicians to prescribe Vetmedin (generic name: pimobendan) to any dog affected with mitral valve disease (MVD) if the dog's vertebral heart size (VHS) value* is at least 11.5, which means, regardless of whether the dog's heart is enlarged or not! They unabashedly state:
"Pimobendan treatment should be initiated in dogs with ... a VHS > 11.5."
* VHS values are calculated based upon x-rays of the dog's heart, and no echocardiography is involved in reaching those calculations. See this link for a discussion of how VHS values are determined.
Briefly, to refresh our memories:
The EPIC trial, which was sponsored by Vetmedin's manufacturer, Boehringer Ingelheim Vetmedica, Inc., concluded that Vetmedin (generic name: pimobendan) could be prescribed to any dog affected with mitral valve disease (MVD or MMVD) if the left atrium and left ventricle of the dog's heart are enlarged, based upon two minimum echocardiogram measurements, and a set of x-rays showed that the dog's heart had a Vertebral Heart Sum (VHS) value greater than (>) 10.5.
The EPIC trial's conclusions were a ground-breaking advance for the administration of pimobendan, because previously the drug was not to be prescribed to MVD-affected dogs before their hearts reached congestive heart failure (CHF). One of the reasons for limiting the use of pimobendan to dogs in heart failure before the EPIC trial had been due to previous studies showing that for dogs not yet in CHF, pimobendan could accelerate the progression of MVD and also damage their hearts in other ways.
The EPIC trial's report concluded:
"Chronic oral administration of pimobendan to dogs with echocardiographic and radiographic evidence of cardiomegaly [enlargement] secondary to MMVD, in the absence of concurrent cardiovascular medication, results in the prolongation of the preclinical period, and is safe and well tolerated."
Note that, as big a step as the EPIC trial took for promoting pimobendan, its investigators still emphasized the necessity of both "echocardiographic and radiographic [x-ray] evidence" that the dog's heart is enlarged due to MVD.
Previously, as we pointed out in our July 10, 2017 blog entry, the CEG had recommended that as long as the dog's x-ray showed a VHS value above 11.5, the dog (any dog, of any breed, regardless of whether its heart is enlarged or not) may be started on pimobendan. In stating that advice, the CEG admitted that their x-ray-only recommendation was not based upon any findings from the EPIC trial nor upon any other evidence. (See the CEG's December 2016 newsletter for that amazing admission. )
Now the CEG has shoved our dogs farther out on its risk-taking limb by reducing the
minimum species-wide VHS parameter from a value greater than 11.5 to
equal
to 11.5. As we mentioned in our earlier article, the CEG is ignoring the
well-researched and documented fact that, for some breeds, especially the
cavalier, a VHS value
 of 11.5
may well mean that the heart is not enlarged at
all. In at least
one study, a VHS value of 11.7 was found normal for
one of the
CKCSs. In that same study, a VHS value as high as 12.6 was normal for
a boxer
in the study,
and as high as 11.7 was normal for a Labrador retriever in the study. In
another study,
a pug had a normal VHS value as high as 14.1, a bulldog as high as 14.4, and
a Boston terrier as high as 13.1.
of 11.5
may well mean that the heart is not enlarged at
all. In at least
one study, a VHS value of 11.7 was found normal for
one of the
CKCSs. In that same study, a VHS value as high as 12.6 was normal for
a boxer
in the study,
and as high as 11.7 was normal for a Labrador retriever in the study. In
another study,
a pug had a normal VHS value as high as 14.1, a bulldog as high as 14.4, and
a Boston terrier as high as 13.1.
The CEG's July 2017 leaflet provides no explanation for the group's recommendation. It cites no veterinary journal articles or other published research. It does not even suggest that its own unpublished research warrants such advice. The CEG just substitutes an arbitrary number -- 11.5 -- for any professional veterinary determination of whether the patient does or does not have an enlarged heart!
At least, in the CEG's December 2016 brochure, the group gave some cautious advice by warning that:
"Documentation of substantial cardiac enlargement is critical to determine whether or not to start pimobendan in dogs with preclinical mxyomatous [sic] mitral valve disease." (Emphasis added.)
That means, not just a little bit of enlargement, but substantial enlargement, is super important!
Now, in its July 2017 "update", the CEG has completely reversed its cautionary approach to prescribing pimobendan and has deleted any suggestion that the heart enlargement be "substantial". As of now, as far as the CEG is concerned, no enlargement at all is a criterion, as long as a minimum VHS value is met!
To sum up:
● The EPIC Study report concludes that pimobendan can delay the onset of heart failure in MVD-dogs with enlarged hearts, based upon both x-ray and echocardiographic measurements of the heart.
● The CEG used to recommend that pimobendan not be prescribed unless the extent of that enlargement was "substantial".
● Now, the CEG recommends that pimobendan should be administered regardless of whether the dog's heart is enlarged at all, as long it's x-ray VHS value is at least 11.5.
● The CEG admits it has no evidence whatsoever to support this advice.
 For some undisclosed reason, the CEG seems just itching to encourage
general practice vets to prescribe pimobendan to dogs without first taking
any steps to verify that the dogs' hearts actually are enlarged. The bottom line appears to be that when Vetmedin's manufacturer
financially supports a group of veterinary cardiologists, cavalier owners
cannot count on those cardiologists to offer well-researched, objective veterinary advice in
treating their dogs for MVD. Once again, follow the money!
For some undisclosed reason, the CEG seems just itching to encourage
general practice vets to prescribe pimobendan to dogs without first taking
any steps to verify that the dogs' hearts actually are enlarged. The bottom line appears to be that when Vetmedin's manufacturer
financially supports a group of veterinary cardiologists, cavalier owners
cannot count on those cardiologists to offer well-researched, objective veterinary advice in
treating their dogs for MVD. Once again, follow the money!
RETURN TO TOP
July 10, 2017:
The Cardiac Education Group waters down
the EPIC trial
recommendations
Heart enlargement no longer counts.
Now, only overall heart size
matters.
Could financial contributions by Vetmedin's manufacturer
play a role in
the CEG giving such
irresponsible advice?
 The
Cardiac Education Group (CEG) is a team of seven board certified veterinary
cardiologists (Drs. John D. Bonagura, Barret Bulmer, Whit M. Church, Sonya
G. Gordon, Brian A. Scansen, Alan W. Spier, and Rebecca L. Stepien), which
is sponsored by a grant from Boehringer Ingelheim Vetmedica, Inc., the manufacturer of
Vetmedin. Vetmedin is a brand name for the drug pimobendan.
CEG's
website professes that:
The
Cardiac Education Group (CEG) is a team of seven board certified veterinary
cardiologists (Drs. John D. Bonagura, Barret Bulmer, Whit M. Church, Sonya
G. Gordon, Brian A. Scansen, Alan W. Spier, and Rebecca L. Stepien), which
is sponsored by a grant from Boehringer Ingelheim Vetmedica, Inc., the manufacturer of
Vetmedin. Vetmedin is a brand name for the drug pimobendan.
CEG's
website professes that:
"The group is committed to providing resources and information on the diagnosis, treatment and management of heart disease and heart failure in dogs and cats in order to promote early detection and diagnosis with greater accuracy and confidences." (Emphasis added.)
Contrary to that stated commitment, the information discussed herein demonstrates that the CEG, at least in the case of when to start prescribing pimobendan to MVD-affected dogs, is providing information which makes for less accuracy and no confidence, and can be putting cavalier King Charles spaniels (CKCS) at greater risk. We are wondering whether Vetmedin's sponsorship is getting in the way of CEG's objectivity.
Five of these CEG cardiologists participated in the EPIC Study trial, about which we have written much in the past*, and one of them, Dr. Gordon, was one of the EPIC trial's three lead investigators. So, why are they ignoring its findings, conclusions, and warnings?
* See, e.g., Pimobendan's EPIC Study: The BAD and the UGLY!; and Will general practice vets cut corners to prematurely prescribe pimobendan to MVD-affected cavaliers?; and EPIC study's bluster about pimobendan unravels as critical analysis finally takes hold.
The EPIC trial, in a nutshell
Briefly, the EPIC trial, which also was sponsored by Vetmedin's
manufacturer, concluded that pimobendan could be prescribed to any dog in
ACVIM Stage B2 of mitral valve disease (MVD or MMVD), if two minimum
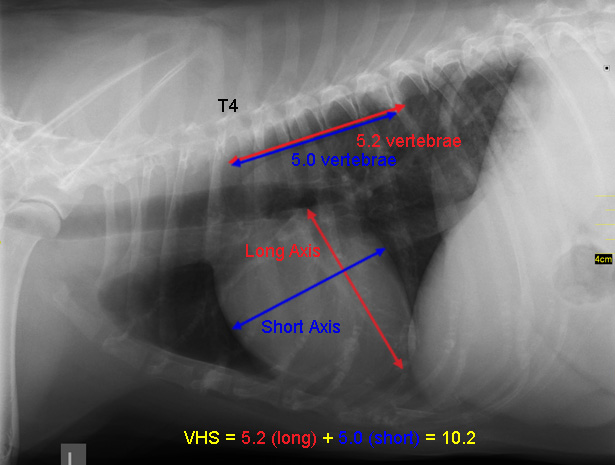 echocardiogram measurements showed that the dog's left atrium and left
ventricle were enlarged and a set of x-rays showed that the dog's heart had
a Vertebral Heart Sum (VHS) value greater than (>) 10.5. (See how a
VHS value is determined, in the x-ray at right.)
echocardiogram measurements showed that the dog's left atrium and left
ventricle were enlarged and a set of x-rays showed that the dog's heart had
a Vertebral Heart Sum (VHS) value greater than (>) 10.5. (See how a
VHS value is determined, in the x-ray at right.)
The EPIC trial's conclusions were a ground-breaking advance for the administration of pimobendan, because previously the drug was not to be prescribed to MVD-affected dogs before their hearts reached ACVIM Stage C, meaning congestive heart failure (CHF). One of the reasons for limiting the use of pimobendan to dogs in heart failure before the EPIC trial had been due to previous studies showing that for dogs not yet in CHF, pimobendan could accelerate the progression of MVD and also damage their hearts in other ways. (See the list of studies, linked here.)
The EPIC trial's report concluded:
"Chronic oral administration of pimobendan to dogs with echocardiographic and radiographic evidence of cardiomegaly [enlargement] secondary to MMVD, in the absence of concurrent cardiovascular medication, results in the prolongation of the preclinical period, and is safe and well tolerated."
Note that, as big a step as the EPIC trial took for promoting pimobendan, its investigators still emphasized the necessity of both "echocardiographic and radiographic [x-ray] evidence" that the dog's heart is enlarged due to MVD.
CEG advises skipping the echo exams entirely
Nevertheless, the CEG has taken a giant leap beyond anything imagined from the EPIC trial findings. In a December 2016 newsletter, the CEG has stated that an echocardiogram may be skipped entirely, and that as long as the dog's x-ray shows a VHS value above 11.5*, the dog (any dog, of any breed, regardless of whether its heart is enlarged or not) may be started on pimobendan. Specifically, it states:
"The strictest interpretation of the trial would suggest that all small breed dogs with a left apical systolic murmur of grade 3/6 or louder should have radiographs taken and an echocardiogram performed to determine if substantial cardiac enlargement is present and pimobendan therapy warranted."
* In a July 2017 "update", the CEG changed the "above 11.5" to "11.5 or above", making the risk even greater that dogs with no enlargement at all will be prescribed pimobendan. See this September 2017 article.
In fact, what CEG calls the EPIC Study's "strictest interpretation" really is the only factually-based one. How does the CEG advise practitioners to distort these results? They continue:
"... If an echocardiogram is not available and only thoracic radiographs are performed, the CEG recommends starting pimobendan in dogs with heart murmurs of grade 3/6 or louder only when the VHS exceeds 11.5 vertebral bodies or an incremental increase of greater than 0.5 vertebral bodies per 6 months is accurately documented." (Emphasis added.)
CEG admits their advice is "not based on evidence"
The CEG goes on to acknowledge that:
"ACVIM guidelines recommend both imaging methods for optimal evaluation of a dog with suspected MMVD. The EPIC trial did not investigate a cutoff for cardiac enlargement by VHS alone at which to start pimobendan therapy. This algorithm represents the consensus of the CEG to initiate therapy when echocardiography is not available, but is not based on evidence." (Emphasis added.)
So, the CEG admits that their x-ray-only recommendation is not based upon the EPIC trial and is not based upon any other evidence! This is a stunning - even jaw-dropping - effort to water-down the recommendations of the EPIC trial's report! In our opinion, the only saving grace of the EPIC trial is that it requires that two precise minimum echocardiographic measurements be met, in addition to the very troubling, species-wide VHS value of >10.5, before prescribing pimobendan to MVD-affected dogs prior to heart failure.
What could possibly motivate the CEG to ignore all of the evidence?
Why would the CEG want to encourage veterinarians to cut corners and not perform echocardiograph examinations in order to determine if the two left chambers of an MVD-affected dog's heart are enlarged? It gives no explanation. We can think of two possible reasons:
● One is that primary care, general practice (GP) veterinarians, either not having ultrasound devices or not being sufficiently trained to use them for echocardiography, might have complained that the EPIC Study's requirement of having echocardiograms was discriminatory against them and in favor of the cardiologists. Since GP vets have been prescribing pimobendan to dogs in heart failure (Stage C) for the past ten years without even having an ultrasound device in their clinics, it should come as no surprisethat they would be inclined to ignore the EPIC Study report's admonition that minimum echocardiograph measurements are necessary, and issue scripts for this very expensive drug (and sell it from their own inventories) for Stage B2 dogs, based only upon x-rays.
● The other is that the manufacturer of Vetmedin, which fully funded the EPIC Study and also financially sponsors the CEG, might have complained that by requiring that echo exams be conducted before pimobendan can be prescribed prior to heart failure, fewer, rather than more, prescriptions for Vetmedin will be issued, resulting in less profit to that benevolent sponsor.
Whatever the reason (they both focus on making more money for somebody), such corner-cutting certainly is of no net benefit to the MVD-affected cavalier King Charles spaniels. Instead of warning veterinarians to not prescribe pimobendan to Stage B2 dogs without first performing any echocardiograms, the CEG is ditching the mandatory echo parameters altogether and is recommending a new, dumbed-down, all-breed x-ray-only parameter for them to follow.
So, based upon the CEG's advice, any GP veterinarian with only an x-ray machine will be able to calculate VHS values and, once the arbitrary, minimum value of >11.5 is met in any dog of any breed, then go ahead and prescribe the pimobendan. But since the CEG admits that there is no research or evidence to back up this deletion of echos as part of the diagnostic process, any veterinarian who chooses to follow the CEG's advice and opt out of using echocardiography is essentially "flying blind" in determining if the dog's heart really is enlarged.
 What the CEG ignores is that, for some breeds, especially the cavalier, a
VHS value of >11.5 likely means that the heart is not enlarged at all. In at
least
one study*, a VHS value of 11.7 was found normal for
one of the CKCSs. So,
why
does the CEG insist upon using a "one size fits all" set of parameters,
which means that the cavalier is put at greater risk? Whether the dog's
heart is enlarged no longer is the issue. Now the question is just how
big the heart is, enlarged or not.
What the CEG ignores is that, for some breeds, especially the cavalier, a
VHS value of >11.5 likely means that the heart is not enlarged at all. In at
least
one study*, a VHS value of 11.7 was found normal for
one of the CKCSs. So,
why
does the CEG insist upon using a "one size fits all" set of parameters,
which means that the cavalier is put at greater risk? Whether the dog's
heart is enlarged no longer is the issue. Now the question is just how
big the heart is, enlarged or not.
* In that same study, a VHS value as high as 12.6 was normal for boxers in the study, and as high as 11.7 was normal for Labrador retrievers in the study. In another study, the pug had a normal VHS value as high as 14.1, the bulldog as high as 14.4, and the Boston terrier as high as 13.1.
At the very least, the CEG's members should pay attention to the advice given in this landmark article on VHS measurements, which expressly states:
"The use of breed-specific VHS values is needed for the VHS method to have a high specificity for normal heart size." (Emphasis added.)
We would prefer using a patient-specific VHS value, rather than just breed-specific, but either one is better than an arbitrary, risky, species-wide VHS value which CEG admits is unsupported by any research or evidence. In this era of more "individualized medicine", there is no justification whatsoever for creating a single, species-wide parameter, especially when it flatly and admittedly contradicts the only peer-reviewed research on the topic.
What has become of using baseline x-rays?
What is even more disturbing is that the CEG does not acknowledge the dirty little secret about GP vets: many of them cannot determine whether a dog's heart is enlarged or not, simply by looking at one set of x-rays -- the so-called "one-off" assessment.* As a result, they often tend to find enlargement when there really is none at all. When that leads to prematurely prescribing pimobendan, severe heart damage can occur, based upon prior peer-reviewed studies. To remedy this hazard, all the CEG members had to do was also recommend that the GP vets make baseline x-rays of their MVD patients before any enlargement takes place, so that the GP vet will be able to compare the VHS of the normal size of the patient's heart in the baseline x-ray to the later x-ray which may (or may not) show enlargement. This is what we mean by using a patient-specific VHS value.
* Even experienced board certified cardiologists will argue over whether a single set of x-rays (they call them "chest rads") shows left side enlargement or not, and if so, its degree. This usually is due to poor positioning of the dog during the x-rays, which is not uncommon. See e.g., Why Is Cardiac Radiology So Difficult? Christopher R. Lamb. WSAVA Congress 2004. ("In a recent study two experienced observers examined the radiographs of 57 dogs with common congenital cardiac anomalies without access to any clinical information in order to avoid biasing their interpretations. Under these conditions, the observers reached the correct diagnosis in less than 40% cases. This poor result reflects the difficulty observers had identifying shape changes that can occur in radiographs of dogs with enlarged cardiac chambers. Radiographic signs of specific cardiac chamber enlargement (or pulmonary vascular abnormalities) were recognised by both observers in only 20% instances in which they might be expected.")
When Dr. James Buchanan, board certified veterinary cardiologist, devised the VHS measurement system in his article, "Vertebral Scale System to Measure Heart Size in Radiographs", he wrote:
"In addition to initial assessment of heart size, the VHS method is also useful in monitoring the progression of heart enlargement over time. Recording the heart size using a vertebral scale encourages objectivity and is a convenient way of recording changes in heart size in response to treatment or progression of cardiomegaly." (Emphasis added.)
Dr. Buchanan subsequently explained to a group of CKCS breeders how the VHS system should work for MVD-affected dogs:
"I would get a chest x-ray when the murmur is first heard. ... Then I would get a yearly x-ray to monitor the development of cardiac enlargement and use heart size as a guide. If [for example] the heart in a baseline x-ray measures 9.5v, and subsequently 10.5v, that indicates cardiac enlargement and the effects of mitral regurgitation." (Emphasis added.)
You see, as the two x-rays at the right show, with two sets of x-rays, one taken before any enlargement takes place and the other when enlargement is suspected, even a veterinary technician with no cardiac experience can measure the dimensions on both sets of x-rays, to arrive at VHS values and be certain that the heart either is or is not enlarged, and if so, by how much. (The two x-rays of one cavalier above at right are a 1999 baseline with no enlargement and a 2004 view showing an increase in heart size. -- Courtesy of the Royal Veterinary College.)
Why the CEG ignored this advice is perplexing. Surely its members are aware that the 2009 ACVIM Consensus Statement, of which three of them - Drs. John D. Bonagura, Sonya G. Gordon, and Rebecca L. Stepien - were among its ten authors, specifically emphasized the importance of obtaining baseline x-rays. Here is what they wrote back in 2009:
"Diagnosis for Stage B: Consensus recommendations: Thoracic radiography is recommended in all patients to assess the hemodynamic significance of the murmur and also to obtain baseline thoracic radiographs at a time when the patient is asymptomatic for CVHD [chronic valvular heart disease]." (Emphasis added.)
Now, the CEG team may reply by saying that, in many instances, no baseline x-rays of the dog have been taken, and it is too late now. Apart from the fact that they never mention the baseline option at all, our response to that situation is for the CEG simply to follow the EPIC trial findings and to require that the dog undergo an echocardiographic examination. To advise vets to waive echo exams for cavaliers, when there is no baseline x-ray for confirming if any enlargement has occurred, is, frankly, encouraging malpractice.
Even with baseline x-rays for comparison purposes, relying upon the x-rays alone and their VHS values only tell the clinician that the heart as a whole is enlarged, and not whether the left atrium (LA) and/or the left ventricle (LV) are enlarged. Maybe a board certified cardiologist can tell from x-rays (rads) alone that the LA or LV is enlarged, but as we noted above, even they will disagree up to 60% of the time, and especially if the positioning of the dog (even flexing the neck can cause misleading shadowing) and quality of the films are less than perfect, or the dog was inhaling in one view and exhaling in another or sedated in one and not in the other. This list could go on and on.
The EPIC trial report emphasizes the importance that both the left atrium and left ventricle be enlarged by specified minimum dimensions, which is important information that the echocardiogram can provide and even an expertly produced x-ray can not.
EPIC lead investigator Adrian Boswood rejects CEG's "algorithm"
Clearly one of the other two lead investigators/authors of the EPIC Study report flatly disagrees with CEG's short-cut diagnostic trick. Dr. Adrian Boswood, in a Q&A article published in The Veterinary Record in February 2017 was asked how primary care vets can reliably identify MVD-affected dogs which would benefit from pimobendan treatment at Stage B2. He answered:
"At the moment we can only be confident that a dog will benefit from therapy if it undergoes diagnostic imaging; ideally echocardiography. It is probably unrealistic to expect that every dog in primary care practice with a moderately loud heart murmur will undergo echocardiography - so is there another way we can find these dogs? The answer to that question is currently - we don't know.
"What I would like to develop is a simple tool or algorithm that may combine factors from a dog's history, clinical examination and perhaps biomarker concentrations to generate a patient risk score. It is possible that such a score could be used to either select those patients in which diagnostic imaging is strongly recommended or, even better, a high score could be used as a basis on which to initiate therapy. We are a long way from having such a validated clinical scoring system, but 10 years ago we were a long way from knowing that pimobendan was effective in the treatment of dogs with preclinical mitral valve disease - and now we do! Difficult questions sometimes take a long time to answer." (Emphasis added.)
In a May 2017 article, Dr. Boswood emphasized the importance of echocardiograph examinations, and "ideally', x-rays to determine if an MVD-affected dog has heart enlargement, before considering treating the dog with pimobendan. He wrote:
"If I am now asked by a practitioner - "should I treat this dog, which I believe has preclinical mitral valve disease, with pimobendan?" - my response will typically be "to be certain that therapy is indicated the dog will need to undergo echocardiography and ideally also radiography." (Emphasis added.)
At least Dr. Boswood recognizes that the condition of the individual dog needs to be taken into account, instead of using an arbitrary, species-wide x-ray measurement which has been proven in previous peer-reviewed studies to inaccurately reflect actual heart enlargement in several breeds of dogs, including the CKCS.
Should we "follow the Vetmedin money"?
 In conclusion, the CEG openly admits that "The EPIC trial did not
investigate a cutoff for cardiac enlargement by VHS alone at which to start
pimobendan therapy." And, the CEG also admits that its x-ray-only parameter
is "not based on evidence." In essence, by these admissions, the only
professional course of action for the CEG to take would be to not make any
such x-ray-only recommendation at all. One must wonder why the CEG is doing
this. Could it be that it was pressured by the manufacturer of Vetmedin
-which fully funded the EPIC Study and financially sponsors the CEG itself - to go out
on such an irresponsible limb?
In conclusion, the CEG openly admits that "The EPIC trial did not
investigate a cutoff for cardiac enlargement by VHS alone at which to start
pimobendan therapy." And, the CEG also admits that its x-ray-only parameter
is "not based on evidence." In essence, by these admissions, the only
professional course of action for the CEG to take would be to not make any
such x-ray-only recommendation at all. One must wonder why the CEG is doing
this. Could it be that it was pressured by the manufacturer of Vetmedin
-which fully funded the EPIC Study and financially sponsors the CEG itself - to go out
on such an irresponsible limb?
RETURN TO TOP
July 3, 2017:
ACVIM forum Consensus Statement further deteriorates
the flawed EPIC Study report
Now they are just making stuff up!
Is a Consensus Statement worth anything
if it is not based upon any
evidence?
 NOVEMBER
2018 UPDATE: The latest word is that the revised ACVIM Consensus
Statement on mitral valve disease in small dogs will not be published
until late 2019, following the June 2019 ACVIM annual forum in Phoenix,
Arizona.
NOVEMBER
2018 UPDATE: The latest word is that the revised ACVIM Consensus
Statement on mitral valve disease in small dogs will not be published
until late 2019, following the June 2019 ACVIM annual forum in Phoenix,
Arizona.
We previously have written about how the lead investigators of the troublesome EPIC Study report had only superficially analyzed the study's own data. For instance, in "Pimobendan's EPIC Study: The BAD and the UGLY! ... And the cherry-picked GOOD news", we pointed out how they arbitrarily chose a minimum Vertebral Heart Score (VHS) value of >10.5 for determining that any and all MVD-affected dogs (of all breeds) had heart enlargement and should be administered pimobendan. Since the average cavalier King Charles spaniel (CKCS), with no heart enlargement whatsoever, has a VHS significantly higher than 10.5 (some as high as 11.7), then following the EPIC Study investigators' VHS parameter would put a substantial number of healthy cavaliers at serious risk of heart damage (because that is what pimobendan can do to healthy dogs which do not need it).
EPIC lead investigator Dr. Adrian Boswood even admitted, in an audio interview (at time 31:24) in November 2016, that the VHS parameter of > 10.5 was too low to amount to heart enlargement for some breeds. He said:
"A vertebral heart score of 10.5 is in the normal range for some dogs, particularly cavaliers actually."
We have also pointed out the that the two echocardiograph parameters chosen by the EPIC Study investigators likewise were arbitrary and do not even fall within the enlarged heart region on a species-wide basis. Regarding EPIC's minimum left ventricle parameter,"body weight normalized left ventricular internal diameter in diastole (LVIDDN)", of > 1.7, in that same audio interview (at time 31:06) in November 2016 that is noted above, Dr. Boswood admitted that the LVIDDN of 1.7 also is below the range for enlargement. He said:
"Now interestingly, if you look in the literature, the normalized left ventricular diameter of 1.7 is in the normal range. The abnormal is above about 1.85, [1.]9, 1.9 depending upon how you read it, so that's nudging the top of the normal range but still normal."
And we pointed out that the EPIC Study's authors attribute their choice of the "left atrial-to-aortic root ratio (LA/Ao)" parameter of > 1.6 to a November 2002 article which found for the CKCSs in its study that had mitral regurgitation (MR) had an LA/Ao ratio of 1.6 ± 0.57. Significantly, however, in that 2002 article, the LA/Ao ratio referred only to dogs which had mitral regurgitation, but it did not refer to dogs with enlarged hearts. The 2002 study's authors were careful to exclude any findings comparing LA/Ao ratios of dogs with and without enlarged hearts.
"In this study, we have deliberately refrained from introducing index ranges for mild, moderate, and severe enlargement, because the grading would be arbitrary and was not included in the study design."
Thus, what would be "arbitrary" to the authors of the 2002 study (and therefore should be excluded) now, in the EPIC Study report, is "top tier" (as one of its authors has described it). "Pseudo-science" is defined as the assertions of alleged scientific data but which are unsupported by empirical evidence. By any standard, the definition of an enlarged heart in this study is a textbook example of pseudo-science.
Even more glaring is that, while the EPIC Study concludes that its minimum enrollment parameters (LA/Ao > 1.6, LVIDDN > 1.7, and VHS > 10.5) should also define enlarged hearts for prescribing Vetmedin in the future, the fact is that none of the dogs in the EPIC Study had heart measurements as low as any of those parameters. The lowest LA/Ao ratio for any dog in the EPIC Study was 1.72 (not 1.6), and the lowest LVIDDN measurement was 1.8 (not 1.7), and the lowest VHS value was 10.9 (not 10.5).
So, neither the EPIC Study's conclusion nor its species-wide definition of heart enlargement are least bit evidence-based. They in fact are directly contrary to the EPIC Study's own, published evidence.
And in our "EPIC study's bluster about pimobendan unravels as critical analysis finally takes hold", we noted that several cardiologists were rejecting the EPIC authors' recommendation to start pimobendan at the first sign of heart enlargement, and calling for a "more measured approach".
 Now we
witness another chink in EPIC's armor. At the June 2017 ACVIM forum (an annual
event for board certified veterinarians, majorly sponsored by Vetmedin's
manufacturer, Boehringer Ingelheim Vetmedica), a team of cardiologists (see
list at right)
ostensibly presented a "Consensus Statement (update): Degenerative Valve
Disease". (We say "ostensibly" because they all are listed on the schedule
but Dr. Keene was the primary presenter, and not all of the others attended.)
Now we
witness another chink in EPIC's armor. At the June 2017 ACVIM forum (an annual
event for board certified veterinarians, majorly sponsored by Vetmedin's
manufacturer, Boehringer Ingelheim Vetmedica), a team of cardiologists (see
list at right)
ostensibly presented a "Consensus Statement (update): Degenerative Valve
Disease". (We say "ostensibly" because they all are listed on the schedule
but Dr. Keene was the primary presenter, and not all of the others attended.)
One thing notable about seven of these ten veterinarians is that they were among the ten authors of the 2009 ACVIM "Consensus Statement: Guidelines for the Diagnosis and Treatment of Canine Chronic Valvular Heart Disease". This is the article which created the stages of severity of mitral valve disease, Stages A, B1, B2, C, and D, which by now everybody is using to categorize how bad the mitral valve disease (MVD) is.
It also should be noted that eight of the presenters at the 2017 ACVIM forum were among the 36 cardiologists who participated in the data gathering of the EPIC Study, and one of these eight, Dr. Jens Haggstrom, was one of the three lead investigators of EPIC and presumably was one of its authors.
Another chink in EPIC's armor
So, what is this new chink in EPIC's armor? Well, here is a photo of a slide which was on the screen at the ACVIM conference while Dr. Keene was making his presentation.
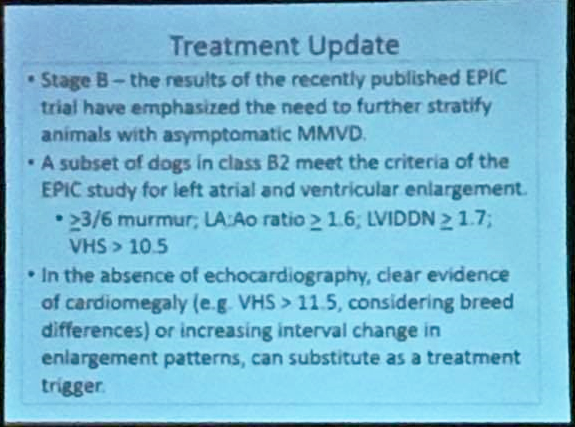 The
first two bullet points of this slide are consistent with the EPIC Study.
The
first two bullet points of this slide are consistent with the EPIC Study.
Nevertheless, the second point, regarding EPIC's definition of enlargement, has been totally discredited as having anything to do with enlargement on a species-wide basis. EPIC Study's inclusion criteria -- vertebral heart size (VHS) >10.5, echocardio-graphically derived normalized left ventricular internal dimension in diastole (LVIDDN) >1.7, and left atrial to aortic ratio (LA:Ao) >1.6 -- do not in reality define enlargement and necessarily include dogs with normal-sized hearts. Despite that, the ACVIM's new Consensus Statement authors seem to blindly accept those arbitrary parameters.
The third bullet point - "In the absence of echocardiography, clear evidence of cardiomegaly (e.g. VHS > 11.5, considering breed differences) or increasing interval change in enlargement patterns, can substitute as a treatment trigger" - is not only not to be found in the EPIC Study report, but is directly contradictory to the recommendations of the EPIC Study's authors.
Now, they are just making stuff up!
● No where in the EPIC Study report is there to be found any advice about administering pimobendan to a dog based solely upon the VHS value from x-rays of the dog's heart. The study's three parameters were specific, and two of the three required M-mode echocardiography to make the measurements. In a December 2016 publication, the Cardiac Education Group (CEG) first proposed this x-ray-only parameter for prescribing pimobendan to Stage B2 dogs. In that publication, the CEG openly admitted that "The EPIC trial did not investigate a cutoff for cardiac enlargement by VHS alone at which to start pimobendan therapy."
● No where in the EPIC Study report is there any reference to VHS values > 11.5. The only VHS value which is mentioned among the EPIC Study parameters is > 10.5. In that same December 2016 publication, the CEG also admitted that its proposed x-ray-only parameter of >11.5 was "not based on evidence."
● No where in the EPIC Study report is there any reference to "breed differences". The EPIC Study authors took great pains to lump all breeds together (despite the fact that nearly half of all of the dogs in the study were CKCSs and in at least one study, a VHS value of 11.7 was found normal for the CKCS).
● No where in the EPIC Study report is there any reference to "increasing interval change in enlargement patterns". As EPIC Study lead investigator Dr. Adrian Boswood emphasized in interviews, all that the veterinarian needs to determine is if there is any enlargement of the dog's heart. Specifically, he stated:
"Patients that will benefit from therapy are those with enlarged hearts (cardiomegaly) and therefore patients with louder heart murmurs should ideally undergo diagnostic imaging in order to determine whether their heart is enlarged. If there is clear evidence of cardiac enlargement then treatment should be initiated." (Emphasis added.)
Indeed, the EPIC Study specifically does not recommend using only x-rays to determine enlargement of the heart. It states:
"The conclusions of this study are only relevant to dogs with cardiac enlargement secondary to preclinical MMVD (stage B2) as all dogs entering the study met or exceeded 3 different heart size criteria (LA/Ao > 1.6, LVIDDN > 1.7, and VHS > 10.5) ... ." (Note that LA/Ao and LVIDDN parameters can only be measured by echocardiogram.)
"Chronic oral administration of pimobendan to dogs with echocardiographic and radiographic evidence of cardiomegaly secondary to MMVD, in the absence of concurrent cardiovascular medication, results in the prolongation of the preclinical period, and is safe and well tolerated." (Emphasis addded.)
So, the message being conveyed by this presumably unanimous "Consensus Statement" of ten cardiologists at the June 2017 ACVIM forum is three-fold:
● First, that despite what the EPIC Study report says about needing echocardiographic measurements to determine enlargement, it is okay to just use x-rays, as long as the VHS value drawn from those x-rays is "e.g. VHS > 11.5, considering breed differences". (What about considering individual dog differences?)
● Second, that despite the EPIC Study's authors' reliance upon a mimimum VHS value of >10.5, that figure is absurdly dangerous if used alone and without echocardiographic measurements. (We may be thankful, finally, for at least that recognition.)
● Third, and perhaps most importantly, an ACVIM Consensus Statement can be based upon neither the EPIC Study research nor any other evidence. (When ten esteemed cardiologists agree upon a treatment protocol that is totally unsubstantiated, what really is going on?)
This band-aid does not solve the EPIC Study's inherent flaws
Whatever this Consensus Statement is intended to be, it does not serve the interests of the canine patient, especially the cavalier King Charles spaniel. All it does is solve the obvious financial/discriminatory/elitest (pick one) implication from the EPIC Study report that only veterinarians trained and experienced in the use of echocardiograph devices (e.g., board certified cardiologists and radiologists) should be determining when to start prescribing pimobendan. While we have no problem at all with that conclusion, it must not have sat well with either the manufacturer of Vetmedin (which fully financed the study and would expect to sell more, not less, pimobendan, and also heavily funds the ACVIM), or with the primary care, general practice (GP) veterinarians who, prior to the publication of the EPIC Study report, diagnosed heart failure and then prescribed pimobendan on a daily basis using more conventional means without the need for echocardiograms.
It was apparent that, regardless of whatever the EPIC Study report had to
say about echos, the GP vets were going to continue prescribing (and
selling) Vetmedin, one way or another. The most likely way for them to determine
enlargement would be solely by x-rays, which they can take all by
themselves. Since all that the EPIC Study report
 had to advise about x-ray
parameters was a VHS value > 10.5, the GPs' bottom-line, take-away advice
from the EPIC Study report was to prescribe pimobendan to dogs with VHS
values of 10.6 and above. This is just about the worst of several terrible
conclusions to be drawn from the ill-drafted EPIC Study report.
had to advise about x-ray
parameters was a VHS value > 10.5, the GPs' bottom-line, take-away advice
from the EPIC Study report was to prescribe pimobendan to dogs with VHS
values of 10.6 and above. This is just about the worst of several terrible
conclusions to be drawn from the ill-drafted EPIC Study report.
So, we guess that the cardiologists at the 2017 ACVIM forum were trying to put out that fire - the legitimate fear that GP vets were going to prescribe pimobendan if the patient had a VHS value as low as > 10.5 and without relying upon echocardiograms at all. We mentioned that fear in our March 2017 article, "Will general practice vets cut corners to prematurely prescribe pimobendan to MVD-affected cavaliers?" But if they had any guts, they would have said the obvious: No Echo? No Pimo!
The only saving grace in the EPIC Study report was the requirement that two echocardiographic measurements be taken, in addition to the VHS measurement from the x-rays. This 2017 ACVIM forum Consensus Statement throws out that protection, leaving the cavalier King Charles spaniel most vulnerable to the damage that premature administration of pimobendan has been shown it can do, in previous peer-reviewed publications. Simply raising the minimum VHS value from >10.5 to >11.5 does not solve the problem for our breed, when cavaliers without any heart enlargement at all may have VHS values above 11.5.
Now, the Consensus Statement cardiologists may counter that the >11.5 value was only a suggested example and not a hard and fast minimum figure. But that is expecting a bit too much from GP vets who otherwise are given no guidelines at all. Their attitude seems to be: "Just tell us what we need to do! Don't make us have to figure it out for ourselves!"
Where does that leave things with the EPIC Study report? Well, it is a totally unsatisfactory band-aid to cover an open, infected, throbbing wound. The dirty little secret about GP vets is that many of them do not know how to determine whether a dog's heart is enlarged or not, simply by looking at one set of x-rays.* As a result, they often tend to find enlargement when there really is none at all. When that results in prematurely prescribing pimobendan, severe heart damage can occur, as prior studies have shown.
* Even experienced board certified cardiologists will argue over whether a single set of x-rays (they call them "chest rads") shows left atrium enlargement or not, and if so, its degree. This usually is due to poor positioning of the dog during the x-rays, which is not uncommon. See e.g., Why Is Cardiac Radiology So Difficult? Christopher R. Lamb. WSAVA Congress 2004. ("In a recent study two experienced observers examined the radiographs of 57 dogs with common congenital cardiac anomalies without access to any clinical information in order to avoid biasing their interpretations. Under these conditions, the observers reached the correct diagnosis in less than 40% cases. This poor result reflects the difficulty observers had identifying shape changes that can occur in radiographs of dogs with enlarged cardiac chambers. Radiographic signs of specific cardiac chamber enlargement (or pulmonary vascular abnormalities) were recognised by both observers in only 20% instances in which they might be expected.")
Can any cardiologist here spell "baseline x-ray"?
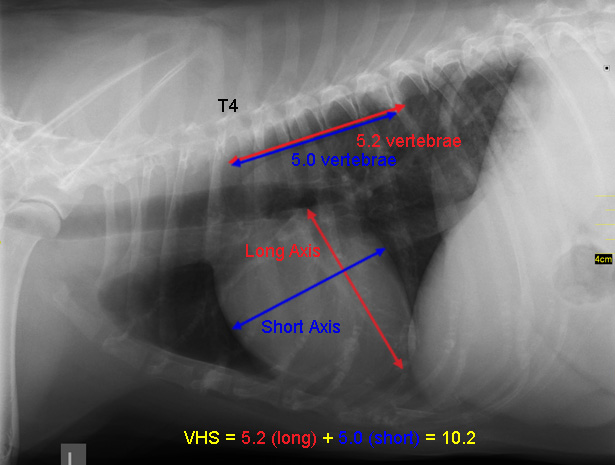 The solution to this dilemma about how to determine enlargement of a
dog's heart has been available since 1995 when Dr. James Buchanan, still a board
certified veterinary cardiologist, devised the VHS measurement system in his
article,
"Vertebral Scale System to Measure Heart Size in Radiographs".
There, he wrote:
The solution to this dilemma about how to determine enlargement of a
dog's heart has been available since 1995 when Dr. James Buchanan, still a board
certified veterinary cardiologist, devised the VHS measurement system in his
article,
"Vertebral Scale System to Measure Heart Size in Radiographs".
There, he wrote:
"In addition to initial assessment of heart size, the VHS method is also useful in monitoring the progression of heart enlargement over time. Recording the heart size using a vertebral scale encourages objectivity and is a convenient way of recording changes in heart size in response to treatment or progression of cardiomegaly."
Dr. Buchanan subsequently explained to a group of CKCS breeders how the VHS system should work for MVD-affected dogs:
"I would get a chest x-ray when the murmur is first heard. ... Then I would get a yearly x-ray to monitor the development of cardiac enlargement and use heart size as a guide. If [for example] the heart in a baseline x-ray measures 9.5v, and subsequently 10.5v, that indicates cardiac enlargement and the effects of mitral regurgitation." (Incidentally, Drs. Keene and Luis Fuentes were in attendance when Dr. Buchanan said that, at a CKCSC,USA symposium in 1998.)
You see, as the two x-rays at the right show, with two sets of x-rays, one taken before any enlargement takes place and the other when enlargement is suspected, even a veterinary technician with no cardiac experience can measure the dimensions on both sets of x-rays, to arrive at VHS values and be certain that the heart either is or is not enlarged, and if so, by how much. (The two x-rays at right show the increase in heart size of one cavalier over 5 years. -- Courtesy of the Royal Veterinary College.)
Unfortunately, neither the authors of the EPIC Study report nor the presenters at the 2017 ACVIM forum even suggest that baseline x-rays be used to compare with current x-rays of the dog's heart. And this is quite amazing when you consider the fact that in the 2009 ACVIM Consensus Statement, seven of the presenters at the 2017 ACVIM forum specifically emphasized the importance of obtaining baseline x-rays. Here is what they wrote back in 2009:
"Diagnosis for Stage B: Consensus recommendations: Thoracic radiography is recommended in all patients to assess the hemodynamic significance of the murmur and also to obtain baseline thoracic radiographs at a time when the patient is asymptomatic for CVHD [chronic valvular heart disease]." (Emphasis added.)
Even with baseline x-rays for comparison purposes, relying upon the x-rays alone and their VHS values only tell the clinician that the heart as a whole is enlarged, and not whether the left atrium (LA) and/or the left ventricle (LV) are enlarged. Maybe a board certified cardiologist can tell from x-rays (rads) alone that the LA or LV is enlarged, but as we noted above, even they will disagree up to 60% of the time, and especially if the positioning of the dog (even flexing the neck can cause misleading shadowing) and quality of the films are less than perfect, or the dog was inhaling in one view and exhaling in another or sedated in one and not in the other. This list could go on and on.
The EPIC trial report emphasizes the importance that both the left atrium and left ventricle be enlarged by specified minimum dimensions, which is important information that the echocardiogram can provide and even an expertly produced x-ray can not.
One more time: retract and re-write this monstrosity of an EPIC Study report!
And so, the flimsy band-aid which the ACVIM presenters have attempted to apply to stanch the bleeding from the oozing infected wound that is the EPIC Study report, does nothing but add more confusion to a topic which deserves preciseness, if cavaliers' lives are to be protected. The EPIC Study report needs to be retracted, thoroughly re-analyzed, and then re-written. Its current rendition is inexcusable. (And, the ACVIM Consensus Statement drafters need to think seriously about following the evidence.)
RETURN TO TOP
June 19, 2017:
American Cavalier King Charles Spaniel Club's
Charitable Trust falls
for the impossible promised dream
At the American Cavalier King Charles Spaniel Club's 2017 national specialty show last month, the ACKCSC Charitable Trust held a fund raising dinner for what the guest speaker claimed would be a trial for ten MVD-affected cavalier King Charles spaniels to be treated with DNA injections. He distributed a colorful flyer (page 1 is here) (page 2 is here) which asserts that the DNA would travel through to the dogs' hearts, modify the protein levels which allegedly are causing enlargement of the hearts, and stop that enlargement. Then, according to the flyer, each of the treated dogs will become "healthier, happier and younger" and live another "8+ years".
(See below the attractive diagram of the six-step process of how this study is designed to work, from Step 1, designing the DNA to Step 6, living another eight years -- from page 2 of the flyer.)
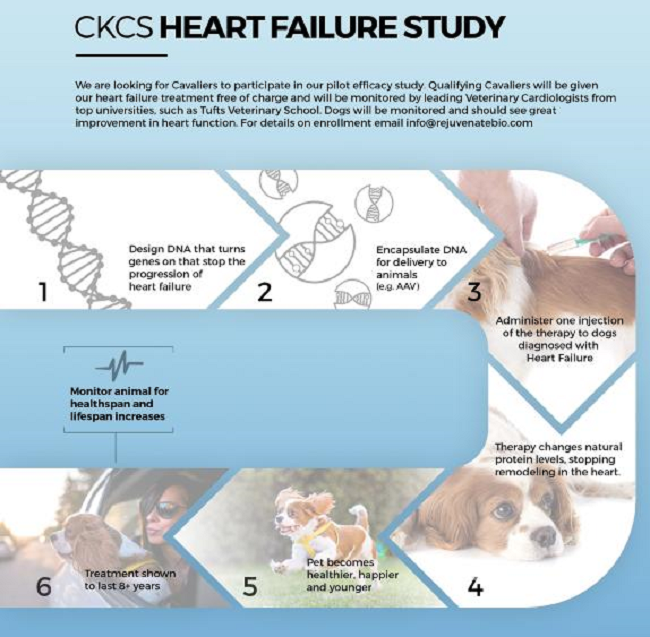
The flyer explains:
"OUR WORK: We have shown the ability to stop the progression of heart failure in mice ... and are now working with Tufts Veterinary School on a safety study in dogs. All the dogs in the safety study are doing great and have shown no deleterious effects from the treatment. We are now looking to launch an efficacy experiment in Cavalier King Charles Spaniels with heart failure. ...
"We are looking for Cavaliers to participate in our pilot efficacy study. Qualifying Cavaliers will be given our heart failure treatment free of charge and will be monitored by leading Veterinary Cardiologists from top universities, such as Tufts Veterinary School. Dogs will be monitored an should see great improvement in heart function."
The speaker and his brochure apparently induced the attendees at the ACKCSC Charitable Trust's banquet to contribute over $10,000.00, and the Charitable Trust now is urging that additional contributions be made to it. The Charitable Trust published this statement on its Facebook page:
"We are so excited and grateful to our members, exhibitors & guests who raised enough money in one evening to fund the next phase of this study where 10 Cavaliers will be given the new genetic therapy. This phase will begin NEXT MONTH! If all goes well, this therapy could be available to all as early as 2019. There will be one more phase of this study before it can go to market, so if you would like to help in this very important research please consider donating to the Charitable Trust through the Darcy Fund."
Now, what could possibly be wrong with any of this? Well, for starters, the hype of the wording is unlike anything any responsible veterinary cardiology researcher would ever dare to make. For instance, no cardiologist would assure, before experimental trials have even begun, that the treatment would "stop remodeling of the heart". Nor would he assure that the treated dog would "become happier, healthier and younger." And he would not dare to assure the dog's owner that the treatment would last for over eight years. So clearly, we are not dealing with responsibly made representations by a responsible, professional veterinarian here. Instead, we are dealing with pure hype! Impossible promised dreams!
Here are some facts about all of this:
• Thus far, no studies to determine which DNA controls the enlargement of dogs' hearts have been published. The only DNA studies thus far cannot even report which genes control the mitral valve of the dog's heart. Instead, different studies have found varying chromosomes which may be involved, and "candidate regions" within some of those chromosomes which may possibly contain one or two of the expected several genes which, working together, affect the mitral valve. Read the details here.
So, when the flyer states that Step 1 is, "Design DNA that turns genes on that stop the progression of heart failure", that step alone could take decades. Think about that!
• Step 2 says, "Encapsulate DNA for delivery to animals (e.g. AAV)." What does that mean? Well. AAV stands for "adeno-associated virus". The virus referred to therein is parvovirus. So, in essence, Step 2 involves preparing DNA to send to the dog's heart in a medium consisting of parvovirus. Think about that!
• Step 3 is: "Administer one injection of the therapy to dogs diagnosed with Heart Failure." Now, that tells something about the candidate dogs - they must be in heart failure, meaning ACVIM Stage C of mitral valve disease. The accompanying photo shows a hypodermic needle being inserted under the loose skin between the dog's shoulder blades.
Please do not assume for one second that this encapsulated DNA in its medium of parvovirus is going to be injected randomly under the loose skin of the dog's back. Encapsulated DNA is injected either directly into a particular vein, or, to be more effective, it is an injection directly into the heart muscle after making a surgical incision through the chest muscle between the ribs, a process called "minithoracotomy". Whether anesthesia will be required remains to be determined, but if it does, it would involve anesthetizing dogs in heart failure. Think about that!
• Step 4 says: "Therapy changes natural protein levels, stopping remodeling in the heart." This step is interesting for a couple of reasons. The obvious one is, how do they know it will do those things? Apparently, if what we are told is the least bit true, only mice have had this treatment. The brochure mentions a "safety study" of dogs, but safety studies only determine if the dogs will survive the treatment. How do they know that "natural protein levels" will be changed? How do they know that "remodeling in the heart" will stop?
Step 4 has one other aspect, and that is what it does not say. It leaves out any mention that this treatment will repair the mitral valve and stop the leaking of blood back into the atrium from the ventricle. All it promises is to stop "remodeling", meaning enlargement. Think about that!
• Step 5 is the easiest one to question: "Pets become healthier, happier and younger." Hopefully, no one would fall for that hype. No one would be naive enough to contribute money on a promise that this treatment will make their cavaliers younger. Or, would they?
• Step 6 is amazing: "Treatment shown to last 8+ years." We know that the only animals treated thus far have been mice. Mice live about twelve months if they are lucky. This flyer is claiming that the mice treated with this DNA injection have lived over eight years. If this was true, then the study must have been going on at least that long.
So that is our analysis of the flyer. Let us take a look at what else the ACKCSC Charitable Trust announcement has to offer. It states, "This phase will begin NEXT MONTH!" Well, it has been a month, and nothing has happened. When shown a copy of the flyer, Tufts veterinary school (actually Cummings School of Veterinary Medicine) expressed surprise because they knew nothing about it.
The flyer also lists a website, RejuvenateBio.com, which as of this date has remained content-free except for a "Coming Soon" page. Messages to its email addy go unanswered. Could this just be a predatory research project scam -- where the goal is to raise funds from gullible contributors -- much like predatory scientific journal publishers con naive researchers to submit their research papers and pay to have them published?
There is a simple lesson for charitable organizations to learn from this: Before giving money to a research program, do a little due diligence and do not just pass around a fire bucket at an annual dog show dinner.
RETURN TO TOP
June 15, 2017:
Ten Frequently Asked Questions
About Cavaliers and Mitral Valve
Disease
Since this website was created in 2001, we have found several recurring questions about our breed, the cavalier King Charles spaniel, and its relationship with mitral valve disease (MVD). Here is a compilation of ten of the most frequently asked questions about this disease:
1. What is a "heart murmur" and how is it graded?
A heart murmur is the presence of a soft whistling sound which can be
heard by a veterinarian using a stethoscope. This examination is called
"auscultation". The murmur sound is caused by the turbulent flow of blood
jetting backwards through the damaged leaflets of the mitral valve from the
left ventricle, into the left
 atrium. This backflow of blood through the
mitral valve, is called regurgitation".
atrium. This backflow of blood through the
mitral valve, is called regurgitation".
As simple a device as the stethoscope may seem to be, many cardiologists consider that auscultation is the best screening test there is for the identification of the presence of mitral valve regurgitation.
The "grades" of mitral valve murmurs are from 1, the mildest, to 6, the loudest. A grade 1 murmur can be heard with a stethoscope in a quiet room. A grade 2 murmur can be consistently heard with a stethoscope. A grade 3 murmur is louder and is heard as soon as the stethoscope is applied. A grade 4 murmur is quite loud, and the vibration can be felt with fingertips without a stethoscope. A grade 5 murmur is still louder, with a precordial "trill". A grade 6 murmur is so loud, it can be heard with the stethoscope removed from the chest, or even without using the stethoscope.
An alternative method of grading murmurs, discussed in this November 2014 article, provides:
• Soft = Grades I and II
• Moderate = Grade III
• Loud = Grade IV
• Thrilling = Grades V and VI
2. Can my dog's regular general practice vet detect a heart murmur?
Yes. Veterinarians are trained to detect mitral valve murmurs using a stethoscope. Most general practice (GP) vets are not as skilled as specialists, particularly cardiologists, to accurately identify the grade of the murmur, but nearly all licensed GP vets should be able to recognize a murmur coming from the mitral valve and judge its grade. Cavaliers should be screened for heart murmurs annually, beginning at age one year, by their regular veterinarians.
In a 2009 "Consensus Statement" published by a panel of the board certified veterinary cardiologists of the American College of Veterinary Internal Medicine (ACVIM), they state:
"Consensus recommendations:
"Small breed dogs, including breeds with known predisposition to develop CVHD [chronic valvular heart disease] (e.g., Cavalier King Charles Spaniels, Dachshunds, Miniature and Toy Poodles) should undergo regular evaluations (yearly auscultation by the family veterinarian) as part of routine health care.
"Owners of breeding dogs or those at especially high risk, such as Cavalier King Charles Spaniels, may choose to participate in yearly screening events at dog shows or other events sponsored by their breed association or kennel club and conducted by board-certified cardiologists participating in an ACVIM-approved disease registry."
3. What is a "baseline" x-ray, and how often should my dog's heart be x-rayed?
Once an MVD murmur is detected, an immediate, initial set of x-rays of
the heart is recommended, to serve as a
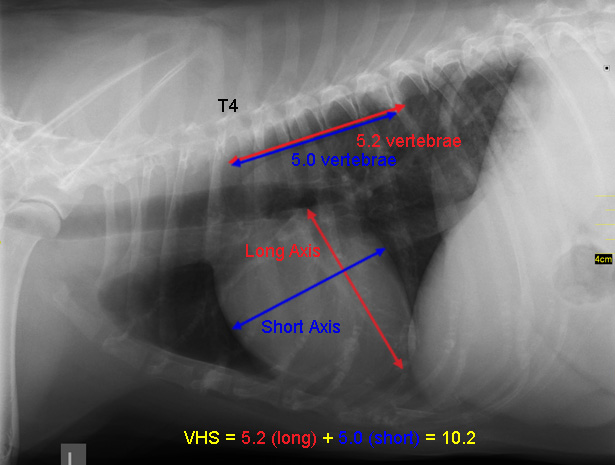 baseline of the size of the heart,
to compare with later x-rays after any enlargement of the heart takes place.
Therefore, annual x-rays thereafter are very useful in charting the
progression of the disease.
baseline of the size of the heart,
to compare with later x-rays after any enlargement of the heart takes place.
Therefore, annual x-rays thereafter are very useful in charting the
progression of the disease.
Measurements are taken of the heart's dimensions on the x-ray, and those are compared with the distance between the dog's vertebrae, to arrive at a Vertebral Heart Score (VHS), for future comparison purposes. (See example at right.)
The ACVIM "Consensus Statement" on degenerative MVD recommends baseline chest x-rays for dogs with a new mitral valve murmur, then annually thereafter. Some MVD drugs, such as pimobendan, are prescribed based upon a determination of the amount of enlargement of the dog's heart which has occurred. Therefore, the initial "baseline" x-rays are very important for determining the extent of any future enlargement.
4. What is an echocardiogram, and when is it necessary?
Echocardiography (ultrasound scanning) is a beam of ultra-high frequency sound directed at the heart, and is used to evaluate heart size, function, and valve appearance. The procedure is non-invasive and painless to the dog. The cardiologist holds a hand-held probe device over the surface of the dog's skin, and sound waves are transmitted to the heart and then echo back again, resulting in displaying real-time images of the heart on the device's video monitor screen.
 The earliest indications of MVD are outwardly invisible and silent and
can only be observed by the ultrasound. Echo scans can demonstrate details
such as the thickened valve leaflets and their abnormal movement, such as
"tethering", "tenting", and prolapse.
The earliest indications of MVD are outwardly invisible and silent and
can only be observed by the ultrasound. Echo scans can demonstrate details
such as the thickened valve leaflets and their abnormal movement, such as
"tethering", "tenting", and prolapse.
Echocardiography enables the cardiologist to assess the size and functioning of the heart chambers. Since MVD affect the size and function of the chambers, particularly the left ventricle (LV) and left artial (LA) chambers, the values determined from echocardiographic scanning are used by the cardiologist as a tool in diagnosing MVD and its progression and severity, as well as when to begin medications.
Cost-conscious cardiologists recommend that most all cavaliers which have been diagnosed by stethoscope and x-ray to have MVD with low grade murmurs and no enlargement, do not need to be examined by echocardiography unless the grade of the murmur has increased rapidly or the dog has begun to display symptoms of MVD. Echocardiograms can be very expensive, and frequently repeated ones can be cost-prohibitive. Once it is recommended that the cavalier be examined by echo, it is the best practice to have that exam performed only by a cardiologist or other heart specialist.
5. What are the "Stages" of MVD, and what does that mean?
In the 2009 "Consensus Statement", the American College of Veterinary Internal Medicine (ACVIM), created a new classification of stages of MVD. They state:
"The new system describes 4 basic stages of heart disease and failure:
"Stage A identifies patients at high risk for developing heart disease but that currently have no identifiable structural disorder of the heart (e.g., every Cavalier King Charles Spaniel without a heart murmur).
"Stage B identifies patients with structural heart disease (e.g., the typical murmur of mitral valve regurgitation is present), but that have never developed clinical signs caused by heart failure. Because of important clinical implications for prognosis and treatment, the panel further subdivided Stage B into Stage B1 and B2.
"Stage B1 refers to asymptomatic patients that have no radiographic or echocardiographic evidence of cardiac remodeling [enlargement] in response to CVHD. [In other words, the dog has a heart murmur but the heart is not enlarged.]
"Stage B2 refers to asymptomatic patients that have hemodynamically significant valve regurgitation, as evidenced by radiographic or echocardiographic findings of left-sided heart enlargement. [In other words, the dog's heart is enlarged.]
"Stage C denotes patients with past or current clinical signs of heart failure associated with structural heart disease. Because of important treatment differences between dogs with acute heart failure requiring hospital care and those with heart failure that can be treated on an outpatient basis, these issues have been addressed separately by the panel. Some animals presenting with heart failure for the 1st time may have severe clinical signs requiring aggressive therapy (eg, with additional afterload reducers or temporary ventilatory assistance) that more typically would be reserved for those with refractory disease (see Stage D). [In other words, the dog is in heart failure.]
"Stage D refers to patients with end-stage disease with clinical signs of heart failure caused by CVHD that are refractory to 'standard therapy' (defined later in this document). Such patients require advanced or specialized Dr.Andrew Beardowtreatment strategies in order to remain clinically comfortable with their disease. As with Stage C, the panel has distinguished between animals in Stage D that require acute, hospital-based therapy and those that can be managed as outpatients."

6. What are typical signs or symptoms of MVD -- (congestive heart failure)?
Rarely does a cavalier display any outward signs or symptoms of MVD until it's heart has enlarged and its murmur grade has risen to 5 or 6. These signs are evidence that the dog has entered "congestive heart failure" (CHF). Once any of these signs/symptoms are noticed, the dog should be examined by a cardiologist as soon as possible. Such signs and symptoms include:
• rapid breathing, usually above 30 breaths per minute while asleep or resting. Breathlessness is a most common sign, starting as excessive panting on exercise. As breathing difficulties become more severe, the dog may sit or stand, holding its elbows away from the chest, and it may be reluctant to sit down.
• productive coughing or a hacking cough.
• exercise intolerance and/or weakness of the hindquarters
• lack of appetite
• restlessness at night
• weight loss
• fainting
• x-rays showing fluids in the lungs or abdomen.
7. When should I make my dog's first appointment with a cardiologist, and what should I bring?
Ideally, for pet cavaliers diagnosed to have an MVD murmur, it should not be necessary to have a board certified veterinary cardiologist conduct a full examination of the dog unless and until the grade of murmur has increased rapidly (such as, from a grade 2 to a grade 3 within six months), or recent x-rays show that the heart has begun to enlarge, or the dog shows signs of MVD. Once enlargement of the heart has been detected, a visit to the cardiologist is in order.
So, be sure to bring those x-rays or arrange for the cardiologist to obtain copies of them.
For cavalier breeders' dogs, the MVD Breeding Protocol, which is designed to eliminate early-onset MVD within three generations, calls for all breeding stock to be examined by board certified veterinary cardiologists prior to being bred.
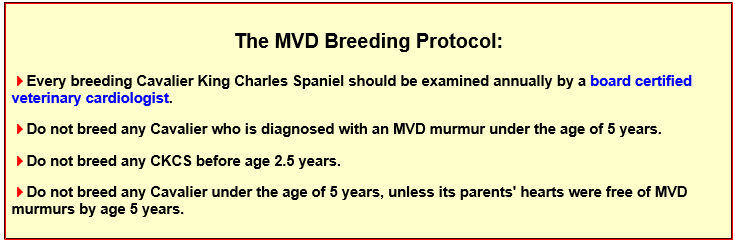
8. When should MVD-affected dogs start medications for MVD?
The simplest answer to that question is: Whenever the cardiologist prescribes them. That implies, as we intended, that only cardiologists should be determining if and when any medications should be started. We do not recommend leaving this decision to GP vets.
There are exceptions to this advice, and the main one is our concern that some cardiologists are too eager to jump-the-gun and start treating MVD-affected cavaliers before medications are necessary, or with drugs which have not been scientifically shown to be effective before the onset of heart failure. We discuss this issue at length in other articles on this website's Blog page.
9. What supplements can I give my cavalier to keep its heart as healthy as possible?
We have a list of a variety of supplements, from basic vitamins and oils, to those specifically designed to strengthen the dog's heart, at different stages of MVD. All of these have been recommended to us by members of our team of veterinarians advising us. A link to that list is here.
10. How accurate are cardiologists' predictions of future lifespans of MVD-affected dogs?
 The short answer to this question is that they usually underestimate the
future lifespan. There have been studies and statistics showing such things
as the mean average life expectancy of MVD-affected dogs, based upon various
starting points, such as when heart enlargement is first detected, or when
the dog enters congestive heart failure. But these averages combine all
sorts of different causes of death attributed to the heart, including sudden
deaths. So, we pay no
attention to such estimates, and in fact, we never ask that question to
begin with.
The short answer to this question is that they usually underestimate the
future lifespan. There have been studies and statistics showing such things
as the mean average life expectancy of MVD-affected dogs, based upon various
starting points, such as when heart enlargement is first detected, or when
the dog enters congestive heart failure. But these averages combine all
sorts of different causes of death attributed to the heart, including sudden
deaths. So, we pay no
attention to such estimates, and in fact, we never ask that question to
begin with.
(The information provided here is drawn from our website's Mitral Valve Disease page, linked here.)
RETURN TO TOP
June 14 2017:
When should intact cavaliers have
a preventative prostate ultrasound?
 In a
June 2017 article in
Theriogenology, an animal reproductive biology
journal, the investigators concluded that the most suitable age for intact
male dogs' prostates to be examined by ultrasound is at 40% of their
expected longevity.
In a
June 2017 article in
Theriogenology, an animal reproductive biology
journal, the investigators concluded that the most suitable age for intact
male dogs' prostates to be examined by ultrasound is at 40% of their
expected longevity.
A thousand and three intact male dogs of 64 breeds, including 10 cavalier King Charles spaniels, were studied to determine an optimal age at which their prostates should be examined by ultrasound as a preventative measure to stave off potentially life-threatening prostatic diseases, such as benign enlargement (prostatic hyperplasia), cysts, mineralization, bacterial infections (prostitis), lesions, abscesses, and tumors. Each breed was individually considered in terms of its expected maximum longevity.
The digital rectal examination of the prostate gland is considered the most convenient method for disease detection. However B-mode ultrasound is referred to as the "gold standard" as a non-invasive screening program. Most all prostate disorders start out asymptomatic and may reach a life-threatening stage without any advance warning.
While the investigators were specific in their recommendation that the dogs be examined when they reach 40% of their expected lifespan, they acknowledged that continued research would be appropriate to determine the effectiveness of such a screening program.
As for cavaliers, the most recent research articles* on the breed's longevity reported an average lifespan of approximately ten years. So, for CKCSs, the optimal age for the prostate ultrasound would be age 4 years.
* Longevity and mortality of owned dogs in England. D G O'Neill, D B Church, P D McGreevy, P C Thomson, D C Brodbelt. Veterinary Journal. December 2013;189(3):638-643 ("Average lifespan of popular dog breeds ... Cavalier King Charles Spaniel 9.9 years."). See also, 2014 UK Kennel Club, Cavalier King Charles Spaniel, Pedigree Breed Health Survey ("... overall median age at death was 10 years; mean age at death was 9.68 years."); Breed Longevity Data. Kelly M. Cassidy. 2008.
RETURN TO TOP
May 28, 2017:
EPIC study's bluster about pimobendan unravels
as critical analysis
finally takes hold
EPIC's recommendation to start pimobendan at the first sign of
heart
enlargement, is rejected for a "more measured approach"
Retract and re-write this ticking time-bomb before it is too late!
According to its lead investigator, Dr. Adrian Boswood, the vaunted and
long-awaited
EPIC Study report, published in September 2016, concluded that any
dog with any heart enlargement due to myxomatous mitral
 valve
disease (MVD), should be prescribed pimobendan. Dr. Boswood (right),
who made the media rounds following the release of the article,
stated:
valve
disease (MVD), should be prescribed pimobendan. Dr. Boswood (right),
who made the media rounds following the release of the article,
stated:
"When a typical mitral valve murmur is detected, vets should now investigate further to look for cardiac enlargement. If demonstrated, this suggests the patient will probably benefit from treatment with pimobendan before the onset of clinical signs."
Elsewhere, he was even more emphatic:
"Patients that will benefit from therapy are those with enlarged hearts (cardiomegaly) and therefore patients with louder heart murmurs should ideally undergo diagnostic imaging in order to determine whether their heart is enlarged. If there is clear evidence of cardiac enlargement then treatment should be initiated."
And, still more emphatic here:
"Now that a benefit of treatment before signs develop has been shown, it is necessary for vets to try to distinguish those dogs with cardiac enlargement (dogs in stage B2) from those with normal-size hearts."
Note that as in the EPIC Study article itself, Dr. Boswood does not distinguish between a little bit and a lot of enlargement or how fast the enlargement is occurring. He says, if you find any enlargement at all, the dog should be prescribed that inordinately expensive drug.
In a previous blog article here, we have been critical of that conclusion, and also of the EPIC authors' analysis of their own data (particularly as it ignores the peculiarities of our breed, placing it at greater risk). And we now find that we have not been alone in that regard. We have identified at least ten board certified veterinary cardiologists thus far who have written criticisms of the EPIC Study report.
The Cardiac Education Group (CEGp), in its
December 2016
"Recommendations" newsletter, back- peddles on prescribing pimobendan to just
any MVD-affected dogs in Stage B2 ("clearly enlarged" left atrium, left
ventricle, or both). This USA panel of seven board certified veterinary
cardiologists (Drs. John D. Bonagura, Barret Bulmer, Whit M. Church, Sonya
G. Gordon, Brian A. Scansen, Alan W. Spier, and Rebecca L. Stepien -- which, ironically, even includes one of the lead investigators
of the EPIC Study and three other participating clinicians in the study),
recommends starting pimobendan on symptomless MVD-affected dogs only if the
dogs' cardiac enlargement is "substantial". In fact, the CEGp thinks the
term "substantial cardiac enlargement" is so important, that they state it
five separate times in their newsletter. To the contrary, nowhere in the
EPIC Study report itself is the extent of heart enlargement distinguished,
and never is the term "substantial" (or any synonym) used to describe
enlargement. If one relies solely upon the EPIC report, any detectable
cardiac enlargement is sufficient to start the drug.
peddles on prescribing pimobendan to just
any MVD-affected dogs in Stage B2 ("clearly enlarged" left atrium, left
ventricle, or both). This USA panel of seven board certified veterinary
cardiologists (Drs. John D. Bonagura, Barret Bulmer, Whit M. Church, Sonya
G. Gordon, Brian A. Scansen, Alan W. Spier, and Rebecca L. Stepien -- which, ironically, even includes one of the lead investigators
of the EPIC Study and three other participating clinicians in the study),
recommends starting pimobendan on symptomless MVD-affected dogs only if the
dogs' cardiac enlargement is "substantial". In fact, the CEGp thinks the
term "substantial cardiac enlargement" is so important, that they state it
five separate times in their newsletter. To the contrary, nowhere in the
EPIC Study report itself is the extent of heart enlargement distinguished,
and never is the term "substantial" (or any synonym) used to describe
enlargement. If one relies solely upon the EPIC report, any detectable
cardiac enlargement is sufficient to start the drug.
Similarly, board certified veterinary cardiologist Dr. Kristin Jacob offered another modified interpretation of the EPIC Study report, using the term "significant" to describe the necessary degree of enlargement (distinguishing it from "mildly enlarged"), when she wrote:
"The data from this landmark study supports the use of Pimobendan once signs of significant left atrial and left ventricular dilation are present but not when the heart size is normal or even mildly enlarged." (Emphasis added.)
It would have been more helpful if these cardiologists quantified "substantial" or "significant" enlargement. We guess they must "know it when they see it." Nonetheless, they clearly are not satisfied with the EPIC Study conclusion that any enlargement at all would warrant starting the dog on pimobendan.
"Not so fast!"
 In
an April 2017 article, USA board certified veterinary cardiologist Dr.
Mark Rishniw (right) took a very critical look at the EPIC Study report. He
questioned the basis for the EPIC Study authors' optimism about starting all
heart-enlarged MVD-affected dogs on pimobendan, regardless of the extent
and/or rapidity of the enlargement. He wrote:
In
an April 2017 article, USA board certified veterinary cardiologist Dr.
Mark Rishniw (right) took a very critical look at the EPIC Study report. He
questioned the basis for the EPIC Study authors' optimism about starting all
heart-enlarged MVD-affected dogs on pimobendan, regardless of the extent
and/or rapidity of the enlargement. He wrote:
"Essentially, the risk of developing CHF or dying was almost halved, regardless of how bad the dog's disease was going into the study. On the face of it, this sounds great. Based on this information alone, every dog with MMVD and left atrial enlargement (correctly identified!) would benefit from pimobendan treatment. Not so fast! The decision to treat a dog requires additional information to be considered. First, the baseline risk of developing CHF needs to be determined, i.e., what is the chance that this dog will actually develop CHF at some point in the future?" (Emphasis added.)
He then took into account the statistics from the EPIC Study and asked this ultimate question:
"Is 'earlier' treatment better than 'later' treatment? The survival curves provide clues to this answer. ... Now, if there was a clear benefit of 'earlier' rather than 'later,' we might expect the survival curves to diverge, ie., continue to move further and further apart. But they don't. For the majority of the study, they remain parallel. So, the benefit with more severely affected dogs is about 300 days, and the benefit with the least severely affected dogs is about 300 days. This suggests that taking the more measured approach of waiting until a dog exhibits evidence of disease progression before instituting therapy is not compromising that dog nor reducing the benefit of the drug. And, dogs that were never going to progress to more severe disease and never develop CHF would not be subjected to needless drug administration (and needless expenses)." (Emphasis added.)
Dr. Rishniw analyzed the EPIC Study's own statistics to observe the falsehood of the EPIC Study authors' simplistic notion that any and all MVD-affected dogs with enlarged hearts, regardless of the degree or rapidity of enlargement, would benefit from pimobendan. As Dr. Rishniw says, "Not so fast!" and that a "more measured approach", looking into the details of each dog's MVD progression, is called for before determining if and when pimobendan may be warranted.
A needless drug and a needless expense
 Then, Dr. Rishniw focused on the economics of starting pimobendan too
early. He wrote that dogs which would likely never progress to congestive
heart failure (CHF) ought "not be subjected to needless drug administration
(and needless expenses)." He raised the suggestion that the EPIC Study's
unwarranted conclusion (that all MVD-affected dogs with any heart
enlargement need pimobendan before CHF) would be a tremendously unnecessary
expense (which may be explained by the drug manufacturer's 100% financial
underwriting of the EPIC Study - including research, travel, speaking fees,
consultancy fees, and preparation of educational materials for
participating cardiologists - and its hoped for additional sales of its very
expensive drug).
Then, Dr. Rishniw focused on the economics of starting pimobendan too
early. He wrote that dogs which would likely never progress to congestive
heart failure (CHF) ought "not be subjected to needless drug administration
(and needless expenses)." He raised the suggestion that the EPIC Study's
unwarranted conclusion (that all MVD-affected dogs with any heart
enlargement need pimobendan before CHF) would be a tremendously unnecessary
expense (which may be explained by the drug manufacturer's 100% financial
underwriting of the EPIC Study - including research, travel, speaking fees,
consultancy fees, and preparation of educational materials for
participating cardiologists - and its hoped for additional sales of its very
expensive drug).
By mentioning that starting pimobendan too early may result in "reducing the benefit of the drug", Dr. Rishniw may be suggesting another possible downside of starting pimobendan before it is truly needed - that the patients may develop a tolerance to the pimobendan, thereby decreasing its effectiveness. Drug tolerance is a pharmacological concept describing the patient's reduced affinity to a drug after sustained exposure to that drug. This means that starting the drug earlier than necessary can result in having to increase the dosage later on to achieve the same beneficial effect. Even worse, at some point the drug may become totally ineffective.
USA board certified veterinary cardiologist Dr.
Mark Kittleson (left) also has objected to the EPIC Study report's
recommendation to start pimobendan as soon as any enlargement is noted.
 He
regards the degree of mitral regurgitation (MR) as the guide for determining
when treatment should begin. He explains that amount of enlargement of the
left atrium (mild, moderate, or severe enlargement) usually correlates with
the degree of mitral regurgitation -- mild, moderate, or severe MR -- which
is the most important factor in determining when to begin treating MVD prior
to heart failure. He says that studies have shown that up to 70% of
MVD-affected dogs with only mild enlargement will never reach heart failure
(Stage C), and so to start them on pimobendan becomes an unnecessary expense
for the dogs' owners, which can be considerable, up to $1,000.00 per year. For dogs with only mild enlargement, he advises periodic
x-rays -- every six months to a year -- to determine if the enlargement has
progressed.
He
regards the degree of mitral regurgitation (MR) as the guide for determining
when treatment should begin. He explains that amount of enlargement of the
left atrium (mild, moderate, or severe enlargement) usually correlates with
the degree of mitral regurgitation -- mild, moderate, or severe MR -- which
is the most important factor in determining when to begin treating MVD prior
to heart failure. He says that studies have shown that up to 70% of
MVD-affected dogs with only mild enlargement will never reach heart failure
(Stage C), and so to start them on pimobendan becomes an unnecessary expense
for the dogs' owners, which can be considerable, up to $1,000.00 per year. For dogs with only mild enlargement, he advises periodic
x-rays -- every six months to a year -- to determine if the enlargement has
progressed.
Therefore, Dr. Kittleson recommends that the drug not be prescribed unless and until the amount of enlargement reaches the severe stage. He also says that a moderately enlarged heart may warrant starting pimobendan, but that waiting until the enlargement reaches the severe stage would be an alternative option.
Treat each patient as an individual
 Earlier, in
a January 2017 article, veterinary
cardiologist Dr. Mikaela Mueller (right) impliedly concurred with Drs. Rishniw's
and Kittleson's viewpoints on the EPIC Study. She wrote:
Earlier, in
a January 2017 article, veterinary
cardiologist Dr. Mikaela Mueller (right) impliedly concurred with Drs. Rishniw's
and Kittleson's viewpoints on the EPIC Study. She wrote:
"One of the major concerns with the EPIC study is that many dogs with only mild enlargement never experience clinical signs of congestive heart failure in the first place, so treating them long-term with pimobendan does not change their clinical outcome. Luckily, it appears to be a very safe medication for the majority of patients, but it is not a cheap medication to give for years when it does not change the outcome. Since we do not have a good way of predicting which dogs with mild disease will progress to clinical signs, it becomes difficult to decide whether or not to recommend pimobendan for some patients. This is where the art of clinical practice comes into play. Each patient is an individual who deserves personalized thought and attention. If a patient has mild cardiomegaly and is already 16 years old, it is far less likely that the patient will progress to congestive heart failure during his or her lifetime than a different patient with similar disease who is only 5 years old." (Emphasis added.)
In a September 2017 article, Virginia-Maryland College of Veteriinary Medicine cardiologists Giulio Menciotti and Michele Borgarelli noted that Stage B2 includes various degrees of heart enlargement -- e.g., slight, moderate, and severe. However, the specific echocardiograph and x-ray parameters for selecting those dogs in the EPIC Study were narrower than the full range of Stage B2 and required that the minimum extent of their heart enlargement be "significant". The authors warn that the benefit observed in the EPIC Study -- delaying the onset of heart failure by approximately 15 months, compared to the placebo group -- must be limited to the narrow inclusion criteria of the study. Specifically, they state:
"It is very important to remark, however, that ACVIM Stage B2 dogs represent a heterogeneous group of patients. Therefore, the benefit observed in the EPIC study can be inferred only for dogs that respect inclusion criteria of this study. In fact, for being enrolled in the aforementioned trial, dogs had to have evidence of significant left cardiac enlargement both at echocardiographic examination (LA/Ao > 1.6, LVIDd divided by allometric scaled BW > 1.7) and on thoracic radiographs (Vertebral Heart Score > 10.5)." (Emphasis added.)
In a June 2022 article, Dr. Rishniw and Dr. Donald J. Brown concluded that the EPIC definition (LVIDDN > 1.7) was "arbitrarily chosen", and they single out five specific breeds, including the CKCS, as having larger left ventricles than average dogs of similar size. They state:
"The EPIC study employed an essentially arbitrary value of LVIDDN to dogs subsequently randomized to treatment with pimobendan or placebo and showed that dogs with LVIDDN>1.7 (and LA:Ao>1.6 and a VHS>10.5V) generally do better with the drug than without. ... The criterion for left ventricular enlargement used by the EPIC investigators for study inclusion has never been critically evaluated as indicative of left ventricular enlargement. ...
"We should note, however, that the definition of LV enlargement proposed by ... the EPIC trial ... is not a reference value, but a somewhat arbitrarily chosen threshold for inclusion in the EPIC trial. Therefore, clinicians adhering to these guidelines should be cautious in ascribing LVIDDN that exceed the threshold value of 1.7 as being indicative of LV enlargement.
Drs. Rishniw and Brown warn that such breeds as the CKCS "likely require breed-specific reference intervals for LVIDDN to correctly identify left ventricular enlargement." They also point out:
"For example, if a dog has a LVIDDN that consistently oscillates around 1.3 (within 0.1 units), an increase to 1.6 could indicate left ventricular enlargement for that dog, despite being within the population-based reference interval."
Retract and re-write this ticking time-bomb
 Like the white-coated sanitation
workers cleaning up behind the
parade of elephants, Drs. Rishniw and Kittleson and Mueller and Jacob and
Menciotti and Borgarelli and the CEGp are critically analyzing the EPIC Study's
own statistics, which the study's authors neglected to do themselves. And in
that process, these post-publication reviewers essentially are amending the EPIC
Study's report findings and conclusions. The
bottom line is that no cavalier owner should jump at the prospect of giving
pimobendan to their dogs unless and until a very careful, thorough study -
"a more measured approach" - is conducted for each patient, to determine the
likelihood that the drug will do any good at the current stage of the dog's
MVD.
Like the white-coated sanitation
workers cleaning up behind the
parade of elephants, Drs. Rishniw and Kittleson and Mueller and Jacob and
Menciotti and Borgarelli and the CEGp are critically analyzing the EPIC Study's
own statistics, which the study's authors neglected to do themselves. And in
that process, these post-publication reviewers essentially are amending the EPIC
Study's report findings and conclusions. The
bottom line is that no cavalier owner should jump at the prospect of giving
pimobendan to their dogs unless and until a very careful, thorough study -
"a more measured approach" - is conducted for each patient, to determine the
likelihood that the drug will do any good at the current stage of the dog's
MVD.
It is very unfortunate that these observations, drawn directly from the EPIC Study's own data, were not discussed in the EPIC Study report itself. It should not be necessary for veterinary practitioners to have to read independent, objective analyses of EPIC Study's own statistics, in addition to the report itself, to get the full picture of how to determine if and when pimobendan should be safely and economically prescribed.
In a
timely critique of medical research papers, published just this week in
Nature, Dr. William G. Kaelin Jr.
 warns that "papers need to
include fewer claims and more proof to make the scientific literature more
reliable." He condemns the kind of shenanigans displayed in the EPIC Study
report, stating:
warns that "papers need to
include fewer claims and more proof to make the scientific literature more
reliable." He condemns the kind of shenanigans displayed in the EPIC Study
report, stating:
"Unanswered questions and unexplained results are often perceived as weaknesses that jeopardize publication. This can encourage bad behaviours, such as cherry picking data so that nothing seems incomplete, inconsistent or unexplained. We should appreciate that papers strengthen science when they candidly acknowledge limitations and puzzling results."
Indeed, in addition to all of its other flaws, the EPIC Study report falls into the trap of "overdiagnosis"*. The study does not distinguish between the various sub-groups of Stage B2 mitral valve disease (i.e., mild, moderate, and severe enlargement). All that Stage B2 defines is mitral regurgitation (MR) with any enlargement of the left side of the heart. Statistically, up to 70% of MVD-affected dogs with mild enlargement will likely never go into heart failure, while dogs with severe enlargement will almost certainly go into heart failure. Treating that 70% of dogs with only mild enlargement with the inordinately costly pimobendan is both unnecessary and a textbook example of overdiagnosis.
* Overdiagnosis. Brennen A. McKenzie. JAVMA. October 2016;249(8):884-889 ("Overdiagnosis can cause waste and misallocation of medical resources and can also increase morbidity and mortality rates and have a deleterious psychological impact on individual patients and their caregivers. The testing leading to overdiagnosis and the subsequent follow-up testing and treatment have obvious financial costs.").
The EPIC Study report needs to be retracted and re-written, so that clinicians are not misled by its lack of critical analysis of its own findings. Otherwise it remains a ticking time bomb. The authors had eighteen months following the end of the study (from March 2015 to September 2016) in which to draft a thorough, objective review of their data, in accordance with the veterinary motto: Do no harm. But, unfortunately, they instead published a conclusion that could have been written by the drug manufacturer's press agent even before the study was started.
RETURN TO TOP
March 16, 2017:
Will general practice vets cut corners to prematurely prescribe pimobendan to MVD-affected cavaliers?
EPIC Study's anti-CKCS x-ray parameter
could lead to widespread
over-prescription abuse
 The
EPIC Study report, published in September 2016 and financed wholly by
the manufacturer of pimobendan (Vetmedin), set three separate minimum
measurements of dogs' heart enlargement before prescribing the drug to any
dog which does not yet display symptoms of congestive heart failure due to
mitral valve disease. Two of those measurements are taken by echocardiograph
devices and the other is by an x-ray of the dog's heart.
The
EPIC Study report, published in September 2016 and financed wholly by
the manufacturer of pimobendan (Vetmedin), set three separate minimum
measurements of dogs' heart enlargement before prescribing the drug to any
dog which does not yet display symptoms of congestive heart failure due to
mitral valve disease. Two of those measurements are taken by echocardiograph
devices and the other is by an x-ray of the dog's heart.
The EPIC investigators were careful to warn that all three of those parameters must be met before prescribing the drug. They stated:
"The conclusions of this study are only relevant to dogs with cardiac enlargement secondary to preclinical MMVD (stage B2) as all dogs entering the study met or exceeded 3 different heart size criteria (LA/Ao > 1.6, LVIDDN > 1.7, and VHS > 10.5) ... ."
Not only that, but the EPIC Study investigators were specific as to which type of echocardiograph method to use (the M-mode, or motion mode), and as to how many images must be examined. They stated:
"Echocardiography was performed on unsedated dogs. The following measurements were taken from at least 3 cardiac cycles and the mean was recorded: the LA/Ao obtained from the right parasternal short-axis 2D view as previously described, the left ventricular internal diameter at end diastole (LVIDd), and left ventricular internal diameter at end systole (LVIDs) measured on the M-mode echocardiogram, obtained from the right parasternal short-axis view. M-mode values were used to derive the fractional shortening (FS%). Normalized dimensions were calculated according to the following formulae: normalized LVIDd (LVIDDN) = LVIDd(cm)/(BW (kg))0.294; normalized LVIDs (LVIDSN) = LVIDs(cm)/(BW(kg))."
But, is it reasonable to expect that most general practice (GP) veterinarians will abide by this advice before deciding to administer pimobendan to MVD-affected cavaliers before the dogs are in congestive heart failure (CHF)? Prior to the EPIC Study, the clear starting point for prescribing pimobendan to MVD-affected dogs was CHF. This parameter was relatively easy to determine because it was generally understood that only dogs displaying symptoms* of heart failure were, in fact, in CHF.
* Symptoms such as: coughing, dyspnea/orthopnea (difficulty breathing / shortness of breath while lying down), anorexia / cachexia (lack of appetite/involuntary weight loss), edema / ascites (fluid collecting in cavities and tissues), restlessness especially at night; tire easily, reluctance to exercise, less playful, lethargic, depressed, collapse / syncopal (fainting or nearly fainting).
It did not take an examination by a board certified cardiologist to determine if a dog was in CHF. It did not even require an echocardiogram to reach that finding. A set of x-rays showing heart enlargement and fluid in the lungs was all that the GP vet needed to make the determination of CHF and start treatment with pimobendan.
Up to now, the vast majority of CHF diagnoses were performed by GP vets, and the vast majority of pimobendan prescriptions were issued by GP vets. At most veterinary conferences, cardiologists would instruct GP vets that they - the GPs - could do these CHF diagnoses themselves and could then prescribe the pimobendan accordingly.
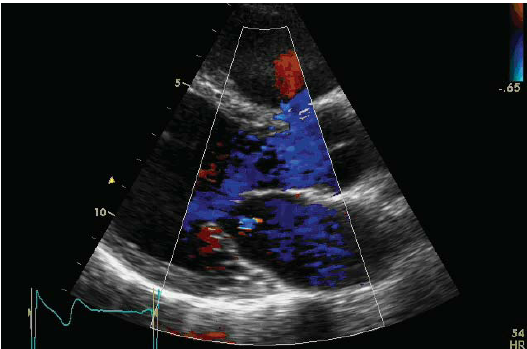 But now that the EPIC Study has turned the CHF diagnosis on its head,
most GP vets may find themselves left out of the loop in diagnosing heart
enlargement and therefore when to start the pimobendan. Very few GPs even
have an echocardiograph ultrasound device, much less know how to use
it in M-mode to measure mitral valve leakage and heart chamber enlargement.
(A screen-shot of an M-mode echo image of a dog's mitral valve is at the
right.)
But now that the EPIC Study has turned the CHF diagnosis on its head,
most GP vets may find themselves left out of the loop in diagnosing heart
enlargement and therefore when to start the pimobendan. Very few GPs even
have an echocardiograph ultrasound device, much less know how to use
it in M-mode to measure mitral valve leakage and heart chamber enlargement.
(A screen-shot of an M-mode echo image of a dog's mitral valve is at the
right.)
Properly using an M-mode echo device is not bean-bag. As board certified veterinary cardiologists Michael R. O'Grady and M. Lynne O'Sullivan explained (actually, they warned), in a recent article*:
"It must be noted that M-mode Echocardiography requires considerable expertise to perform properly. The most technically demanding feature is to identify the exact positions in the heart that fulfill the criteria established to obtain the specific parameters to be measured. Furthermore, the specific location for calaper placement to properly measure the desired parameters has been rigidly established. For adequate interlaboratory comparison of data, the established criteria must be rigidly adhered to."
* Clinical Cardiology Concepts for the dog and cat. Michael R. O'Grady, M. Lynne O'Sullivan.
Clearly, exactitude is the minimum requirement for properly using M-mode echocardiography, and very few GPs will likely have the training and experience to accurately calculate the two echo parameters which must be followed in order to safely prescribe pimobendan to MVD-affected dogs prior to heart failure.
So, what may we expect the GP vets to do about this? Up until now they have been doing most all of the diagnosing of heart failure and the prescribing of pimobendan to dogs in CHF. Now they are being told to take these three measurements, two of which they likely are incapable of doing, because of lack of the equipment and lack of the expertise.
Does this mean that, from now on, GP vets will stop prescribing pimobendan and, instead, refer all of their MVD-affected dogs with suspected enlarged hearts to the specialists - the cardiologists? WE THINK NOT!
We predict that many GPs will rely only upon that third parameter - the
x-ray - to determine if their MVD-affected patients have enlarged hearts and
therefore should be prescribed pimobendan.
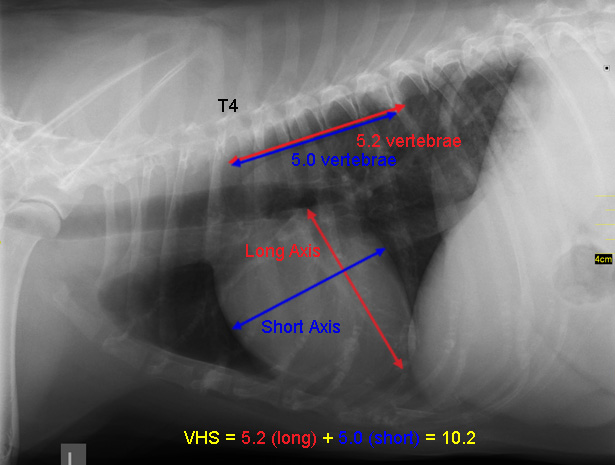 That "third parameter", if you
will recall, is a VHS value greater than 10.5. VHS stands for Vertebral
Heart Score. Veterinarians use x-rays to measure the length and width of the
heart and compare those dimensions to the number of the dog's veterbrae from
T4 to T12, to calculate the Vertebral Heart Score. A diagram showing how the
VHS is calculated is shown in the image at the right.
That "third parameter", if you
will recall, is a VHS value greater than 10.5. VHS stands for Vertebral
Heart Score. Veterinarians use x-rays to measure the length and width of the
heart and compare those dimensions to the number of the dog's veterbrae from
T4 to T12, to calculate the Vertebral Heart Score. A diagram showing how the
VHS is calculated is shown in the image at the right.
An obvious downside of measuring only the VHS value to determine enlargement is that MVD normally initially causes only the left atrium (LA) to enlarge, while the VHS method is not precise enough to measure only the size of the LA.
Cardiologist Dr. Mark Rishniw warns of the combined effect of the dangers of diagnosing heart enlargement using x-rays alone, and the likelihood that the high cost of echocardiography also will play a role in whether veterinarians will rely solely upon x-rays to determine if their MVD patients should be prescribed pimobendan. He states:
"Given that many clinicians struggle to correctly identify cardiomegaly in small-breed dogs from radiographs and tend to over-interpret cardiac enlargement, the investigators stressed that the diagnosis should be made with the benefit of echocardiography. Obviously, many clients will not be able to afford echocardiography, and clinicians will be faced with the decision based on radiographic evidence alone."
Already, at least one cardiologist, Dr. Philip R. Fox, an EPIC Trial participant, has advocated prescribing pimobendan based upon either x-rays or echos! He writes:
"In light of these findings, clinicians should change how they diagnose and manage MVD. Dogs with heart murmurs should be screened early, rather than wait for clinical signs of coughing or respiratory distress to develop. Assessment can be effectively made using history and physical examination along with the added benefit of chest radiography and/or echocardiography."
Already, general practice vets are clambering on board this x-ray-only wagon. Here is the distorted way one UK veterinary clinic advises its MVD-affected clientele of how to determine when to start pimobendan:
"Last year, the results of a long running study into a medication (Vetmedin) used to treat heart failure were published (the EPIC study). This study particularly looked at treating dogs before the onset of heart failure, to see if it could be delayed. The study found that treating dogs which had mitral valve disease, and an enlarged heart as a result, with Vetmedin delayed the onset of heart failure and the need to start other medications. If a murmur is detected in your dog, the size of their heart can be measured using an x-ray or an ultrasound scan of the heart (echocardiography). These tests can be performed here at Orchard Vets, or your pet can be referred to a specialist in cardiology for a more detailed examination." (Emphasis added.)
It appearts that this clinic is well-prepared to prescribe pimobendan after just an x-ray and to skip "a more detailed examination."
What is wrong with using only the dog's x-ray to determine if the dog's heart is enlarged, you may ask? Well, in the case of the EPIC Study parameter of VHS > 10.5, a whole lot is terribly wrong for our cavalier King Charles spaniels. You see, the average heart-healthy cavalier has a VHS value significantly above 10.5. It is troubling that the EPIC Study report fails to note that normal, heart-healthy cavaliers may have VHS measurements as high as 11.7*, which is notably higher than the 10.5+ criterion for beginning pimobendan treatment. Considering that nearly half of the dogs in the EPIC Study were CKCSs, this oversight is rather inexplicable and potentially life-threatening for our breed.
* Lamb CR, Wikeley H, Boswood A, Pfeiffer DU. Use of breed-specific ranges for the vertebral heart scale as an aid to the radiographic diagnosis of cardiac disease in dogs. Vet Rec. June 2001;148(23):707-11. Hansson K, Haggstrom J, Kvart C, Lord P. Interobserver Variability of Vertebral Heart Size Measurements in Dogs with Normal and Enlarged Hearts.Veterinary Rad. & Ultrasound, March 2005, 46(2): 122.
And so, we predict that many GPs will start prescribing pimobendan to cavaliers with mitral valve murmurs if their VHS values are only higher than 10.5, even though all of the published research on VHS values of healthy CKCSs find that their average VHS is greater than 11.0 and some much higher than that. This means that many cavaliers will be administered pimobendan even though they have absolutely no heart enlargement.
What does it mean for cavaliers with healthy hearts to be taking pimobendan? Well, pimobendan is not a sugar pill. It has been shown to have dangerous consequences when given before it is needed. Here are examples of the potentially life-threatening hazards to the premature dosing of pimobendan:
In "Comparative adverse cardiac effects of pimobendan and benazepril monotherapy in dogs with mild degenerative mitral valve disease: a prospective, controlled, blinded, and randomized study", published in 2007 in the Journal of Veterinary Internal Medicine, the researchers found that "PIMO has adverse cardiac functional and morphologic effects in dogs with asymptomatic MVD."
In "Increased Mitral Valve Regurgitation and Myocardial Hypertrophy in Two Dogs With Long-Term Pimobendan Therapy", published in 2005 in Cardiovascular Toxicology, the researchers concluded "This is the first report to describe an increase in mitral regurgitation under clinical conditions in dogs treated with pimobendan. We also suggest that pimobendan may induce ventricular hypertrophy."
In Cardiac Care for Pets (CVCA) "Pimobendan- A Silver Bullet?", published in May 2009, the cardiology department stated: "In a small study performed by CVCA, it was determined that after two to three weeks of Pimobendan therapy about 75% of dogs had an increased frequency of ventricular arrhythmias documented on 24 hour ambulatory ECG monitoring."
In the U.S. Food and Drug Administration's (FDA) 2007 report approving the use of pimobendan for dogs, it stated this conclusion in a four week toxicity study of pimobendan administered to 30 previously healthy lab Beagles:
"Conclusions: Pimobendan administered IV daily to healthy Beagles caused dose dependent increases in heart rate, mitral valve myxomatous thickening, left ventricular outflow tract endocardial thickening, and ventricular muscle ischemic lesions (multifocal subendocardial necrosis and scarring). The cardiac pathology seen in these dogs is typical of positive inotropic drug toxicity in normal dog hearts, and is related to the physiologic effect of the drug on contractility and exaggerated hemodynamic response."On Vetmedin's website, it had this warning: "The safety of VETMEDIN has not been established in dogs with asymptomatic heart disease."
Additionally, veterinary cardiologists spoke out against the premature use of pimobendan:
Dr. Amara Estrada warned: "There is evidence that treatment with a positive inotropic agent such as pimobendan prior to the development of systolic myocardial failure can have deleterious effects. ... Pimobendan ... should be reserved for use when systolic myocardial failure is detected or suspected."
Dr. George A. Kramer warned: "Most dogs with chronic heart disease do not have decreased contractility and do not need positive inotropic support."
Dr. Mark Rishniw warned: "One study in dogs with early mitral valve disease suggested an increase in valve damage in the dogs give pimobendan."
The bottom line is to not allow any GP vet to prescribe pimobendan to any cavalier King Charles spaniel, no matter how loud the GPs scream.
RETURN TO TOP
February 3, 2017:
Does detecting heart failure in MVD-affected cavaliers
matter
anymore?
More vets are prescribing heart failure drugs before heart failure
Their new threshold is called "enlargement"
The slippery slope of drug tolerance is ignored
Peer-reviewed research be damned!
Anecdotal reports are meaningless,
unless the cardiologists want to
believe them
 For
decades, hundreds of veterinary cardiologists have been researching dozens
of ways to determine if and/or when dogs, especially our cavalier King
Charles spaniels (CKCS), affected with mitral valve disease (MVD) are at
risk to enter into congestive heart failure (CHF).
For
decades, hundreds of veterinary cardiologists have been researching dozens
of ways to determine if and/or when dogs, especially our cavalier King
Charles spaniels (CKCS), affected with mitral valve disease (MVD) are at
risk to enter into congestive heart failure (CHF).
They have taken x-rays to measured heart enlargement and lung congestion.
They have counted breaths.
They have counted heart beats.
They have devised complicated calculations of measurements of the heart's left ventricle and left atrium, using several different types of echocardiograph methods, including one-dimension (M-mode, or 1-D), two-dimension (2-D), and three-dimension (3-D) echocardiographic modes and devices, color-flow Doppler, tissue Doppler imaging, the Tei Index, left ventricular torsion, and speckle-tracking.
They have used cardiac magnetic resonance imaging (cMRI).
They have used computed tomography (CT).
They have used advanced electrocardiography (ECG or EKG).
They have measured natriuretic peptides.
They have measured these other cardiac biomarkers: cardiac troponin I (cTnI), and high-sensitivity cardiac troponin I (hscTnI), C-reactive protein (CRP), sodium-calcium exchanger (NCX-1), aldosterone concentration (UAC), serum serotonin (serum 5HT), antidiuretic hormone (ADH), histamine concentration, enzymes and growth factors, Galectin-3 (Gal-3), vitamin D, microRNAs (miRNAs), serum cystatin-C (Cys-C) and symmetric, dimethylarginine (SDMA), oxidative stress, serum fatty acids, serum leptin and adipokines, anemia, desmin, vimentin, periostin, caspase-3, complement factor H isoform 2, calpain-3 isoform X2, dystrobrevin beta isoform X7, CD5 molecule-like and l-2-hydroxyglutarate dehydrogenase.
They have studied DNA and cell transitions.
All for what? To determine when the dog's MVD progresses to heart failure.
But why has it been so important to pinpoint the moment of heart failure? Because the commencement of heart failure traditionally has been the threshold for medicating the MVD, based upon peer-reviewed scientific research.
But the operative words seem to be "has been".
Because, no longer is the start of heart failure the balance-tipper for
plying pills into the MVD patient.
 It
seems that now, even otherwise cautious cardiologists have jumped the gun
and started the pill-plying before heart failure. Now, instead
of heart failure, the operative word is "enlargement". If the
left atrium or left ventricle is the least bit enlarged, that seems to be
the latest excuse for these canine heart specialists to start writing their
prescriptions for their cocktails of pimobendan, diuretics, ACE-inhibitors,
and spironolactone.
It
seems that now, even otherwise cautious cardiologists have jumped the gun
and started the pill-plying before heart failure. Now, instead
of heart failure, the operative word is "enlargement". If the
left atrium or left ventricle is the least bit enlarged, that seems to be
the latest excuse for these canine heart specialists to start writing their
prescriptions for their cocktails of pimobendan, diuretics, ACE-inhibitors,
and spironolactone.
And, they are prematurely pushing these pills without any peer-reviewed veterinary cardiology research to support their multitude of medicinal scripts. The one possible exception is the EPIC Study, which, when its troubling flaws are ignored, arguably justifies prescribing pimobendan to MVD-affected dogs with enlarged hearts but no CHF if two echocardiograph measurements and one radiograph measurement exceed precise minimum dimensions.* But even the EPIC Study tested only one medicine - pimobendan - without any other medications combined with it.
*To make matters worse, some veterinary cardiologists are urging clinicians to not even bother with finding any enlargement before prescribing pimobendan. Instead, they are recommending that if the clinicians find from radiographs that a dog's vertibral heart score (VHS) value is at least 11.5, it would be perfectly proper to skip the echocardiogram and administer pimobendan to that dog, regardless of whether the dog's heart is actually enlarged or not. See our blog articles "The Cardiac Education Group waters down the EPIC trial recommendations" and "Cardiac Education Group doubles down on prescribing Vetmedin (pimobendan) to dogs without enlarged hearts" and "Dr. Sonya Gordon recommends pimobendan for Stage B2 dogs even without echocardiograms".
No excuse for starting diuretics, ACE-inhibitors, or spironolactone before CHF
There is no excuse for prescribing diuretics before CHF because no unwanted fluids are being retained in the dog's heart or lungs until heart failure starts. Plus, loop diuretics stimulate the renin angiotensin aldosterone system (RAAS), which is known to accelerate the progression of MVD, including sodium and water retention, vasoconstriction, and heart enlargement. Thus, the premature administration of diuretics in Stage B2 can cause the onset of Stage C. And, there is no excuse for prescribing ACE-inhibitors to cavaliers prior to heart failure because the SVEP Trial of 229 CKCSs conclusively showed that they do not extend the time in which cavaliers reach heart failure. And, there is no excuse for prescribing spironolactone prior to heart failure because there is no peer-reviewed research showing that it would have any benefit to pre-CHF dogs.
But, despite the lack of veterinary research justifying the pre-CHF dosing of these drugs, it unquestionably has become the mainstream way to treat mitral valve disease these days. No longer are many cardiologists following the principle of "do no harm".
That means, in the context of prescribing diuretics, they should wait until the MVD-affected dogs are retaining fluids which need to be removed. It does not mean giving the diuretic in advance of fluid retention, in the blind hope of preventing or delaying it. We say, "blind hope" because there is no peer-reviewed research which shows that giving a diuretic to a dog which is not retaining fluids will prevent the dog from retaining fluids and otherwise do no harm to that dog. Considering the harmful side effects of diuretics -- impairing kidney function and activating the renin-angiotensin-aldosterone system (RAAS) -- there is no upside to starting them before they are needed.
Nevertheless. even board certified cardiologists are relying upon that blind hope and risking the health of cavaliers by prescribing Lasix to them despite no evidence of heart failure. See this excerpt from a cardiologist's report in which the vet admits that "though there is no congestion at this time ... I would like to start a low dose of Lasix to help delay the onset of heart failure."
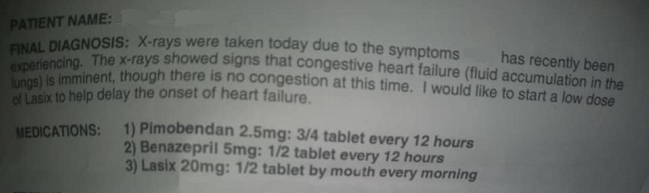
It means, in the context of prescribing ACE-inhibitors to cavaliers, they should wait until the MVD-affected dog is in heart failure. It does not mean giving the ACE-inhibitor in the blind hope of preventing or delaying it. We say, "blind hope" because there is no peer-reviewed research which shows that giving an ACE-inhibitor to an MVD-affected CKCS before heart failure will prevent or delay the onset of heart failure and otherwise do no harm to that dog. In fact, the research, the SVEP Study, concluded the opposite - that ACE-inhibitors prior to heart failure does not delay the onset of MVD in the 229 cavaliers in that study. ACE-inhibitors have documented side effects which could be avoided if the drugs are not prescribed prematurely.
And it means, in the context of prescribing spironolactone, they should wait until the MVD-affected cavalier is in heart failure. It does not mean giving the spironolactone in the blind hope of preventing or delaying it. We say, "blind hope" because there is no peer-reviewed research which shows that giving spironolactone to an MVD-affected dog before heart failure will prevent or delay the onset of heart failure and otherwise do no harm to that dog. In addition, spironolactone has been approved within the European Union only for use in dogs with clinical signs of heart failure.
The slippery slope of drug tolerance is ignored
 Another hazard to the premature administration of these drugs is that the
patients may develop a tolerance to the drugs, thereby decreasing their
effectiveness. Drug tolerance is a pharmacological concept
describing the patient's reduced affinity to a drug after sustained exposure
to that drug. This means that starting the drug earlier than
necessary can result in having to increase the dosage later on to achieve
the same beneficial effect. Even worse, at some point the drug may become
totally ineffective.
Another hazard to the premature administration of these drugs is that the
patients may develop a tolerance to the drugs, thereby decreasing their
effectiveness. Drug tolerance is a pharmacological concept
describing the patient's reduced affinity to a drug after sustained exposure
to that drug. This means that starting the drug earlier than
necessary can result in having to increase the dosage later on to achieve
the same beneficial effect. Even worse, at some point the drug may become
totally ineffective.
Drug tolerance is a known factor in treating MVD-affected dogs with diuretics, since in nearly all cases, the dosage of the diuretic must be increased over time. In the case of furosemide, it eventually can become so ineffective that it must be replaced with the ten-times more powerful torsemide.
Also, in the EPIC Study, an un-acknowledged (by its authors) but obvious consequence of the pre-CHF administration of pimobendan is the evidence that the time between heart failure and death appeared to be shorter than for dogs in the placebo group. In the placebo group, the dogs did not receive pimobendan until they reached CHF, while in the pimobendan group, the dogs were started on the pimobendan from day one. A most plausible hypothesis for this evidence is a pharmacological tolerance to the drug, but the authors of the EPIC Study have ignored that data which their study produced, much as they have chosen to overlook other apparent downsides to their study, replete as their report is with cherry-picked good news.
Anecdotal reports are meaningless, unless the cardiologists want to believe them
So, why do these cardiologists
ignore the peer-reviewed research and prescribe these drugs to MVD-affected
dogs before heart failure?
 We
have asked some cardiologists that very question, and their answers have
been consistent and also troubling. They respond that they do not agree with
the research. In some cases, they argue that the parameters of the research
were not appropriate; in others, that the doses of the drugs in the studies
were too low. In still others, they claim the early dosing has worked for
their patients -- in other words, their own anecdotal evidence. But in no
case have they cited any alternative research to justify their decisions to
blindly prescribe these drugs to our cavaliers before they really need them.
They do not cite any alternative research, because there is
none!
We
have asked some cardiologists that very question, and their answers have
been consistent and also troubling. They respond that they do not agree with
the research. In some cases, they argue that the parameters of the research
were not appropriate; in others, that the doses of the drugs in the studies
were too low. In still others, they claim the early dosing has worked for
their patients -- in other words, their own anecdotal evidence. But in no
case have they cited any alternative research to justify their decisions to
blindly prescribe these drugs to our cavaliers before they really need them.
They do not cite any alternative research, because there is
none!
A typical example is that of USA veterinary cardiologist Dr. Jonathan Abbott, who acknowledges in his presentations before veterinary groups that:
"the value of ACE inhibitors in dogs with subclinical (asymptomatic) valvular disease is uncertain [citing the SVEP and VETPROOF studies] ... but ACE inhibitors appear not to do harm and there was the suggestion of a decrease in all cause mortality."
His is kind of a Mad Magazine-esque "Why Not?" attitude that we should not expect from cardiology specialists. Actually, the value of ACE-inhibitors is not the least bit uncertain for cavaliers. The SVEP Study makes it very certain that they are worthless, at best. The possibility of progressive drug-tolerance never seems to cross their expert minds.
All too often, cardiologists will tell cavalier owners that ancedotal reports about the effectiveness of supplements (e.g., CoQ10, Vitamins C and E, fish oils) are meaningless, and therefore the cardiologists do not recommend the supplements. However, it appears that when the anecdotal reports -- or even worse, just gut feelings -- come from those cardiologists themselves, they not only are meaningful, but they are more reliable than the peer-reviewed studies which contradict them. In short, these cardiologists are following the basic tenet of hypocrisy. The problem is that they are applying that tenet to our dogs and putting them at risk.
RETURN TO TOP
January 20, 2017:
All that cavalier owners need to know
about spironolactone
A mild, potassium-sparing diuretic treatment for mitral valve disease
 Spironolactone
(Aldactone, Prilactone) is both an aldosterone antagonist and a
potassium-sparing diuretic. It has been approved within the European Union
for use in dogs with clinical signs of heart failure secondary to MVD
(meaning, the ACVIM Consensus Statement's Stage C), as adjunctive therapy.
It typically acts as a comparatively weak diuretic, when administered alone,
but has synergistic effects when combined with other diuretics.
Spironolactone
(Aldactone, Prilactone) is both an aldosterone antagonist and a
potassium-sparing diuretic. It has been approved within the European Union
for use in dogs with clinical signs of heart failure secondary to MVD
(meaning, the ACVIM Consensus Statement's Stage C), as adjunctive therapy.
It typically acts as a comparatively weak diuretic, when administered alone,
but has synergistic effects when combined with other diuretics.
The main reason for prescribing spironolactone is to protect the dog against the harmful effects of aldosterone on the heart and blood vessels. Aldosterone is a hormone in the mineralocorticoids group. Its function is to regulate blood pressure and sodium potassium levels. High levels of this hormone may have harmful effects in the heart, including as mechanism of cardiac remodeling, meaning enlargement. Spironolactone reportedly is rapidly absorbed through the dog's gastrointestinal tract into the bloodstream and then converted to active metabolites. Its value level is highest when it is administered with food.
Approved for cavaliers in Stages C and D - congestive heart failure
Spironolactone is a drug often prescribed by veterinary cardiologists to cavalier King Charles spaniels in congestive heart failure (CHF) resulting from our breed's worst nemesis, mitral valve disease (MVD). It usually is not in the first wave* of medications prescribed for CHF, but typically is added as the heart failure worsens.
* That "first wave" - called "conventional therapy" - consists of pimobendan, a loop diuretic such as furosemide, and an ACE-inhibitor such as enalapril. (Spironolactone is not a loop diuretic.)
In this 2010 European study, spironolactone, when added to the conventional CHF therapies, was found to significantly decrease the risk of reaching the primary endpoint (i.e., cardiac-related death, euthanasia, or severe worsening) in dogs with MVD. However, this 2011 report indicated that spironolactone did not extend survival times of dogs with advanced heart failure.
 In
a
2013 study of the possible increased risk of adverse events for dogs
taking spironolactone in addition to conventional therapies, the researchers
concluded that dogs with heart failure receiving spironolactone in addition
to conventional treatment are not at a higher risk for any adverse events,
such as death caused by cardiac disease, renal disease, or both. This study
was funded by the manufacturer of Prilactone, a spironolactone trade name.
In
a
2013 study of the possible increased risk of adverse events for dogs
taking spironolactone in addition to conventional therapies, the researchers
concluded that dogs with heart failure receiving spironolactone in addition
to conventional treatment are not at a higher risk for any adverse events,
such as death caused by cardiac disease, renal disease, or both. This study
was funded by the manufacturer of Prilactone, a spironolactone trade name.
The guidelines of the American College of Veterinary Internal Medicine (ACVIM) 2009 Consensus Statement on MVD (chart at right) recommend spironolactone as an additional therapy in dogs with Stage D MVD. A majority of panelists recommended the use of spironolactone to treat Stage C MVD, although a 100% consensus agreement was not reached. Oddly, a minority of the ACVIM panelists recommended the use of spironolactone in dogs Stage B2 MVD. (See below.)
Cardalis is a tablet which combines spironolactone with the ACE-inhibitor benazepril. Aldactazide is a combination of spironolactone and hydrochlorothiazide, which inhibits the activity of the hormone aldosterone.
Spironolactone is NOT approved for cavaliers in Stage B2
 There
are no veterinary studies recommending beginning spironolactone in Stage B2.*
To repeat that: There are NO veterinary studies recommending
beginning spironolactone in Stage B2! The emphasis is
necessary because that fact is inexplicably ignored by many veterinarians
and even several cardiologists.
There
are no veterinary studies recommending beginning spironolactone in Stage B2.*
To repeat that: There are NO veterinary studies recommending
beginning spironolactone in Stage B2! The emphasis is
necessary because that fact is inexplicably ignored by many veterinarians
and even several cardiologists.
* Stage B2 of MVD consists of an MVD murmur and heart enlargement but no symptoms of heart failure.
The DELAY Study: In 2010, a team of Italian cardiologists, led by Dr. Michele Borgarelli (now at VA-MD Regional College of Veterinary Medicine in Virginia, USA), began the DELAY Study to determine if giving combined doses of spironolactone and benazepril can delay the onset of symptoms of heart failure in dogs with MVD. The results of the study were reported in a January 2020 article, and they were mixed. A total of 183 dogs participated, including 34 cavaliers (19%), the highest number of purebreds. Mixed breeds totaled 72 (40%). The dogs were divided into a treatment group (87 dogs) and control group (92 dogs) which received a placebo and no medication. At the end of the study, 42 dogs in the treatment group and 33 in the control group remained (most of the drop-outs opting to switch treatment to pimobendan). Of those, the median time to reaching heart failiure in the treatment group was 902 days, and the median time in the placebo group was 1,139 days, a difference of 237 days, roughly 8 months. However, the treatment group's heart measurements showed that treatment could reduce -- and in some cases even reverse -- heart enlargement and reduce NT-proBNP. They concluded:
"This study failed to demonstrate a prolongation of the asymptomatic phase of the disease in this population of dogs. Nevertheless, the treatment appears effective in reducing or even reverse cardiac remodeling as indicated by various cardiac imaging parameters and NT-proBNP concentrations. Chronic administration of combined spironolactone and benazepril treatment in dogs with pre-clinical MMVD and cardiac enlargement is safe and well tolerated. The significant effect of this treatment on secondary end-points could be of clinical relevance and merits further study."
Dr. Borgarelli reiterated in a December 2016 email that, "About your question on prescribing spironolactone to cavaliers prior to heart failure at this moment there is no scientific background for this recommendation."
In conclusion, spironolactone may extend the lives of cavaliers in heart failure (Stages C and D) due to MVD, if added to conventional medications at an appropriate time as the MVD progresses. Care must be taken to assure that the drug's downsides do not interfere with the dog's bodily systems. As for prescribing spironolactone to cavaliers in Stage B2, there is no scientific justification for any veterinarian to do so, whatsoever.
RETURN TO TOP
December 20, 2016:
Why do any veterinarians prescribe useless drugs
to
MVD-affected cavaliers before heart failure?
ACE-inhibitors, loop diuretics, and spironolactone
have not been
shown to work before
heart failure
And, they may have damaging side effects
 There is no question that, once cavalier King Charles spaniels (CKCS)
affected by mitral valve disease (MVD) reach the point of congestive heart
failure (Stage C of MVD),
research studies have shown that some medications can delay the progression
of their MVD to the ultimate end point, death. Those drugs include
pimobendan (Vetmedin, Cardisure, Safeheart 5), ACE-inhibitors (e.g.,
enalapril, benazepril, imidapril), loop diuretics (e.g., furosemide,
hydrochlorothiazide), and spironolactone.
There is no question that, once cavalier King Charles spaniels (CKCS)
affected by mitral valve disease (MVD) reach the point of congestive heart
failure (Stage C of MVD),
research studies have shown that some medications can delay the progression
of their MVD to the ultimate end point, death. Those drugs include
pimobendan (Vetmedin, Cardisure, Safeheart 5), ACE-inhibitors (e.g.,
enalapril, benazepril, imidapril), loop diuretics (e.g., furosemide,
hydrochlorothiazide), and spironolactone.
However, there is only one research study showing that any of these medications can delay the progression of MVD of cavaliers before they reach congestive heart failure (CHF). Those CKCSs have enlarged hearts but are not in CHF, and are in Stage B2 of MVD. That medication is pimobendan, and the study is the EPIC Study, published in September 2016. Some cavaliers in Stage B2 of MVD may benefit from starting low doses of pimobendan, as long as they meet the strict minimum parameters of the EPIC Study findings.
So, as our main title asks, why do any veterinarians, even including some
board certified cardiologists, prescribe the other drugs -- ACE-inhibitors,
loop diuretics, and spironolactone --
 to Stage B2 cavaliers since those
drugs have not been shown to work in Stage B2?
to Stage B2 cavaliers since those
drugs have not been shown to work in Stage B2?
We ask this question because, amazingly and unfortunately, many veterinarians do prematurely prescribe these drugs to cavaliers, and we are very concerned that these veterinarians are putting our CKCSs at risk of harm. None of these drugs, when given to a dog before they are medically needed, are harmless like sugar pills. Plus, generally, the more drugs a patient takes, the greater the risk of adverse events and drug-drug interactions. This piling on of drugs is a disease in and of itself, suffered by the prescribing veterinarians. It is called polypharmacy syndrome.
Let us examine each inappropriate pre-CHF drug individually:
ACE-inhibitors
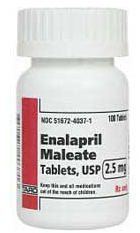 The question of whether ACE-inhibitors can delay heart failure in CKCSs
was answered with a definitive "NO" in 2002, when the
SVEP Trial
(Scandinavian Veterinary Enalapril Prevention Trial) was published. The
SVEP study included 229 MVD-affected cavalier King Charles spaniels, of
which 107 CKCSs also had heart enlargement (Stage B2). The
researchers concluded that the ACE-inhibitor enalapril did not delay the
onset of CHF, compared to the placebo group. The authors stated:
The question of whether ACE-inhibitors can delay heart failure in CKCSs
was answered with a definitive "NO" in 2002, when the
SVEP Trial
(Scandinavian Veterinary Enalapril Prevention Trial) was published. The
SVEP study included 229 MVD-affected cavalier King Charles spaniels, of
which 107 CKCSs also had heart enlargement (Stage B2). The
researchers concluded that the ACE-inhibitor enalapril did not delay the
onset of CHF, compared to the placebo group. The authors stated:
"[T]his study failed to show any preventive effect of enalapril for developing CHF. ... Indeed, the finding in this study, ie, that enalapril did not prevent CHF regardless of whether the dogs had cardiomegaly or not at the time of initiation of therapy, speaks against the possibility that ACE inhibition prevents progression of dilatation. Accordingly, the practice of starting ACE inhibitor treatment in dogs with MVD as soon as cardiomegaly is evident, as is commonly recommended and used in clinical practice, is not supported by the present study. ... In conclusion, long-term treatment with ACE inhibition in asymptomatic dogs with MVD does not delay the onset of CHF regardless of whether cardiomegaly is present at initiation of therapy or not. " (Emphasis added.)
In addition to that SVEP Trial, in 2007 the manufacturer of enalapril sponsored a similar study (the VETPROOF Trial), which included 124 dogs of several breeds, only 10 of which were cavaliers. In that study, the authors found that the ACE-inhibitor enalapril "modestly delays the onset of CHF in dogs with moderate to severe mitral regurgitation."
They also grudgingly acknowledged the importance of the SVEP Trial results. They wrote:
"The VETPROOF, reported here, suggests that enalapril treatment provides a modest benefit in delaying onset of CHF, whereas the first and larger of these studies, the SVEP trial, does not."
The VETPROOF authors further acknowledged the importance of SVEP's 229 cavaliers versus their multi-breed enrollment with only ten cavaliers. They wrote:
"It is noteworthy that the natural history of mitral valve regurgitation and the RAAS in Cavalier King Charles Spaniels are different from those of other breeds".
As recently as April 2017, veterinary cardiologist Mark Rishniw summed up the effectiveness of ACE-inhibitors in treating MVD prior to heart failure, thusly:
"At least 3 studies have examined the ability of ACE inhibitors in this respect. All failed to demonstrate a protective effect of early ACE inhibitor therapy."
In a February 2020 article, Dr. Mark Rishniw carefully dissected all five drug-company-funded studies of the ACE-inhibitor enalapril (the IMPROVE, COVE, LIVE, SVEP, and VETPROOF studies) to determine whether the drug would delay the onset of cardiac death in MVD-affected dogs in heart failure (CHF) or would delay the onset of CHF in pre-clinical MVD-affected dogs (i.e., in Stages B1 or B2). While the conclusions of some of the studies were muddled by drug-company interference, Dr. Rishniw's analysis of the underlying data showed that ACE-inhibitors have not been scientifically shown to delay the onset of either CHF or cardiac death due to MVD. He goes on to determine that:
"In retrospect, it became clear that the veterinary community was hoodwinked into believing that ACE-I were the medical cure for CHF dogs because of corporate marketing decisions."
"So, what does all this mean? My interpretation of all this literature suggests that ACE-I have no place in managing mitral valve disease, whether in dogs with CHF or dogs with subclinical disease."
Notwithstanding that conclusive peer-reviewed research evidence, even some cardiologists prescribe ACE-inhibitors before heart failure. In fact, a majority of the ten members of the 2009 ACVIM Consensus Statement panel recommended starting an ACE-inhibitor at Stage B2, although their reasoning was not included in the Consensus Statement, and the Consensus Statement recommendations apply to all breeds and not just CKCSs. Since the vote was not unanimous, the ACVIM Consensus Statement did not endorse ACE-inhibitor therapy of MVD dogs at Stage B2 MVD. Further, ACE-inhibitors have not been approved for veterinary medicine for MVD dogs in Stage B2 by regulating authorities.
Additionally, it is well established that ACE-inhibitors can have undesireable side effects, particularly to dogs' kidneys. ACE-inhibitors may contribute to renal dysfunction by activating the renin-angiotensin aldosterone system (RAAS). Other side effects include the accumulation of toxins which can damage the liver, anorexia or loss of appetite, vomiting, azotemia -- elevation of blood urea nitrogen (BUN) -- and the development of a dry cough due to the accumulation of bradykinin. Since a dry, hacking cough is a frequent symptom of progressing MVD, this side effect of the drug could be confused with the worsening of the disease.
So, why does any veterinarian prescribe ACE-inhibitors to MVD-affected cavaliers before heart failure?
Well, we may have an answer. In a January 2017 article, veterinary cardiologist Mikaela Mueller suggests a kind of placebo effect, making both the cavalier's owner and the veterinarian feel better about their situation. She writes:
"As doctors, we want to be able to fix problems for our patients. Sadly, this is one disease that we cannot fix (yet). We have been frustrated alongside our clients with nothing to offer them in this common preclinical stage. One intervention that has gotten a lot of research attention is ACE-inhibitors. We seemto really want them to make a difference in delaying the time to onset of congestive heart failure, maybe because we can make physiological justifications for why ACE-inhibitors should, theoretically, help. Multiple studies have shown 'trends' to improvement, but no statistical significance (VETPROOF, SVEP). Many arguments suggest that we simply haven't performed the right study to find the benefit, but one could also argue that if multiple different studies didn't show a statistical difference, then the true benefit is likely modest, at best. That said, I think many of us have prescribed ACE-inhibitors in the preclinical stage just in case it does help. It makes us, and our clients, feel like we are doing something that may possibly help, while we are, in all honesty, in a position where our hands are tied." (Emphasis added.)
In that vein, the Cardiac Education Group (CEGp), in its December 2016 "Recommendations" newsletter, takes the placebo effect one step farther by pretending that the VETPROOF trial concluded something that the CEGp cardiologists know, deep in their heart of hearts, it did not say at all. CEGp writes:
"Interpretation of prior veterinary trials (SVEP and VETPROOF) investigating enalapril in preclinical mitral valve disease dogs failed to achieve a statistically-significant benefit compared to placebo. However, in VETPROOF some secondary endpoints were in favor of enalapril and on average there was a modest delay in the onset of CHF by about four months." (Emphasis added.)
Ah, thank goodness for those secondary endpoints! So, despite the documented, peer-reviewed proof that ACE-inhibitors are a waste of time and money prior to heart failure (especially for cavaliers!), the CEGp places feel-good over professionalism and ends up recommending an ACE-inhibitor before heart failure, anyway. And they don't even cite anecdotal evidence in this case!
Another typical excuse for prescribing ACE-inhibitors is that of USA
board certified veterinary cardiologist Dr.
 Jonathan Abbott,
who acknowledges
in his presentations before veterinary groups that:
Jonathan Abbott,
who acknowledges
in his presentations before veterinary groups that:
"the value of ACE inhibitors in dogs with subclinical (asymptomatic) valvular disease is uncertain [citing the SVEP and VETPROOF studies] ... but ACE inhibitors appear not to do harm and there was the suggestion of a decrease in all cause mortality."
His is kind of a Mad Magazine-esque "What, Me Worry?" attitude that we should not expect from cardiology specialists. Actually, the value of ACE-inhibitors is not the least bit uncertain for cavaliers. The SVEP Study makes it very certain that they are worthless, at best. The possibilities of an adverse kidney reaction and progressive drug-tolerance never seem to cross their expert minds.
There is a name for this feel-goodism in the veterinary field. It is a syndrome called the "caregiver placebo effect". It even has been studied and published. See this November 2012 article, "Caregiver placebo effect for dogs with lameness from osteoarthritis". And, yes, according to this article, it could apply to veterinarians as well as to dog owners. Specifically regarding ACE-inhibitors, such as enalapril, this synrome is called "placebopril". But we don't think that is what is going on here. We do not think the veterinarians who prescribe ACE-inhibitors to cavaliers not yet in heart failure are unknowingly falling for the caregiver placebo effect. Instead, we suspect that they are doing what Dr. Mueller described in her quote above, when she wrote:
"As doctors, we want to be able to fix problems for our patients. Sadly, this is one disease that we cannot fix (yet). We have been frustrated alongside our clients with nothing to offer them in this common preclinical stage. ... I think many of us have prescribed ACE-inhibitors in the preclinical stage just in case it does help. It makes us, and our clients, feel like we are doing something that may possibly help, while we are, in all honesty, in a position where our hands are tied."
And so, probably more than half of all board certified cardiologists, and countless general practice vets, still are prescribing ACE-inhibitors to cavaliers, in direct opposition to the scientific evidence. While the drug may not be very expensive, it is dangerous enough that the standard protocol before prescribing it is to require two (usually expensive) blood panels, one before starting the drug and a second one 10 to 14 days afterwards, focusing mainly upon the kidney results (BUN and creatinine), because of the possible damage this "harmless" drug can do to some dogs' kidneys.
Loop diuretics
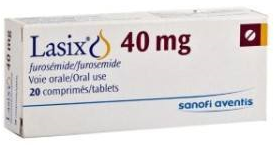 Diuretics, by definition, are intended to increase the
excretion of water from the bodily system. When an MVD-affected cavalier
reaches Stage C, congestive heart failure, that means that fluids are
building up in the heart and lungs or abdomen due to the heart not functioning
properly. In fact, the word "congestive" refers to the build-up of fluids.
So, it is very easy to understand why veterinarians would prescribe a
loop diuretic, such as furosemide (Lasix), once the cavalier enters CHF.
Diuretics, by definition, are intended to increase the
excretion of water from the bodily system. When an MVD-affected cavalier
reaches Stage C, congestive heart failure, that means that fluids are
building up in the heart and lungs or abdomen due to the heart not functioning
properly. In fact, the word "congestive" refers to the build-up of fluids.
So, it is very easy to understand why veterinarians would prescribe a
loop diuretic, such as furosemide (Lasix), once the cavalier enters CHF.
There is no excuse for prescribing diuretics before CHF because no unwanted fluids are being retained in the dog's heart or lungs until heart failure starts. As board certified veterinary cardiologist Dr. Janet Olson states in her December 2016 article about diuretics, "Therefore, it is necessary to take thoracic radiographs to confirm the presence of pulmonary edema prior to starting lasix." Plus, loop diuretics stimulate the renin angiotensin aldosterone system (RAAS), which is known to accelerate the progression of MVD, including sodium and water retention, vasoconstriction, and heart enlargement.
The ACVIM Consensus Statement on MVD in dogs does not even suggest starting diuretics on MVD-affected dogs until the congestive heart failure stage.
Nevertheless. even board certified cardiologists are prescribing Lasix to cavaliers without any evidence of heart failure. See this excerpt from a cardiologist's report in which the vet admits that "though there is no congestion at this time ... I would like to start a low dose of Lasix to help delay the onset of heart failure."
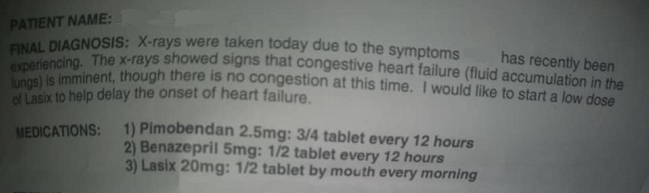
But why would any veterinarian prescribe a diuretic to an MVD-affected cavalier which does not have any fluid build-up?
Spironolactone
 The most surprising MVD drug which we have found
to be
prescribed before heart failure is this one. Spironolactone is mild diuretic
but also has other attributes which in some cases makes it a useful
supplemental drug to cavaliers in CHF, when combined with the others --
pimobendan, ACE-inhibitor, and diuretic -- to delay the dog's death.
The most surprising MVD drug which we have found
to be
prescribed before heart failure is this one. Spironolactone is mild diuretic
but also has other attributes which in some cases makes it a useful
supplemental drug to cavaliers in CHF, when combined with the others --
pimobendan, ACE-inhibitor, and diuretic -- to delay the dog's death.
But there is no research evidence showing that spironolactone has any value at all when given to cavaliers not yet in CHF. Also, it has its own downsides. It is a potassium-sparing diuretic, meaning that it may lead to excessively high, life-threatening levels of potassium in the dog's blood, particularly when combined with ACE inhibitors.
Therefore, cautious veterinary cardiologists recommend that potassium levels be carefully monitored when using spironolactone in combination with ACE-inhibitors, by drawing blood at regular intervals until it is evident that the potassium level is or is not going to be a problem.
So, why would any veterinarian prescribe spironolactone to an MVD-affected cavalier before heart failure?
Perhaps it is the same caregiver placebo effect we mentioned above. We suggest that you ask your vet, if any of these instances happen to your cavalier King Charles spaniel.
RETURN TO TOP
October 3, 2016:
Pimobendan's EPIC Study: The BAD and the UGLY!
... And the cherry-picked GOOD news
Why have the researchers thumbed their noses at the CKCS?
Over-diagnosis can be good for the drug business
-
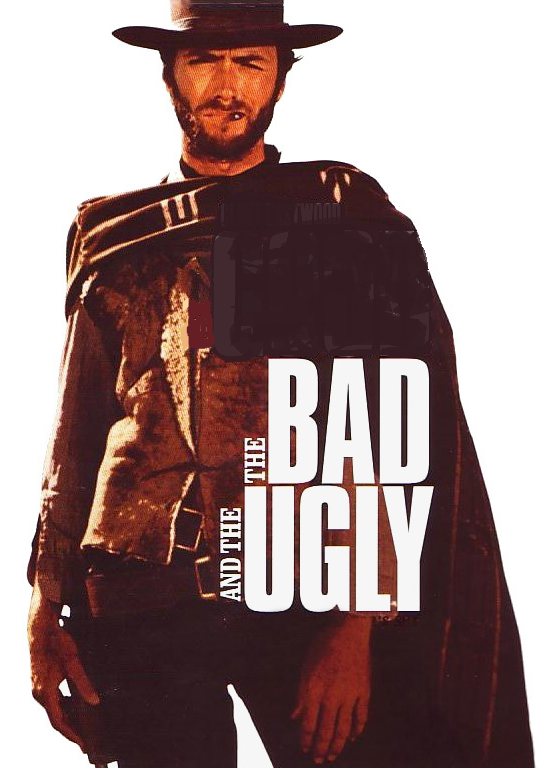 The
hazards of pimobendan treatment before CHF
The
hazards of pimobendan treatment before CHF - The qualifications for dogs to be in the EPIC trial
- The unfortunate March 2015 press releases
- What the final report DOES say
- The BAD and the UGLY!
The long-awaited and highly vaunted final report on the EPIC (Evaluation of Pimobendan In Cardiomegaly) trial study was published on September 28, 2016. The trial has been of utmost importance to owners of cavalier King Charles spaniels (CKCS) because it has been thought that it could mean extending the lives and well-being of CKCSs suffering from mitral valve disease (MVD), which affects and kills more cavaliers than any other cause.
The questions the EPIC trial raised were whether daily oral administration of the drug pimobendan to MVD-affected dogs before they reached heart failure (CHF), (a) was safe and well tolerated, and (b) would prolong the length of time MVD-affected dogs lived before reaching CHF.
Pimobendan is a propriety drug owned and manufactured by the German pharmaceutical company, Boehringer Ingelheim Animal Health GmbH. The drug is not available as a generic. It is marketed primarily under the name Vetmedin, but also as Cardisure, Safeheart 5, and Fortekor Plus.
We have covered this trial from its inception in a series of articles on this blog site. (See our April 23, 2011, March 25, 2015, February 2, 2016, August 3, 2016, and September 30, 2016 articles.) As most of these previous articles indicate, we have been suspicious of the motives underlying this trial from the beginning. Our main concern has been that the trial has been fully financed by the manufacturer of pimobendan. The manufacturer's underwriting included paying the 36 veterinary cardiologists involved in the study, including compensating them for their research, travel, speaking fees, consultancy fees, and preparation of educational materials, in addition to providing all of the pimobendan for the 360 dogs in the trial.
There is a scientific term which describes what the EPIC Study amounts
to. It is called "Shambolic
 Research",
which means that its researchers have shown a tendency to conduct incomplete
research and then announce their desired conclusions. Perhaps these were not
the conclusions desired by all 36 researchers here, but they certainly were
desired by the study's financier, and as we shall observe below, possibly
also by one or more of the lead investigators.
Research",
which means that its researchers have shown a tendency to conduct incomplete
research and then announce their desired conclusions. Perhaps these were not
the conclusions desired by all 36 researchers here, but they certainly were
desired by the study's financier, and as we shall observe below, possibly
also by one or more of the lead investigators.
The hazards of pimobendan treatment before heart failure
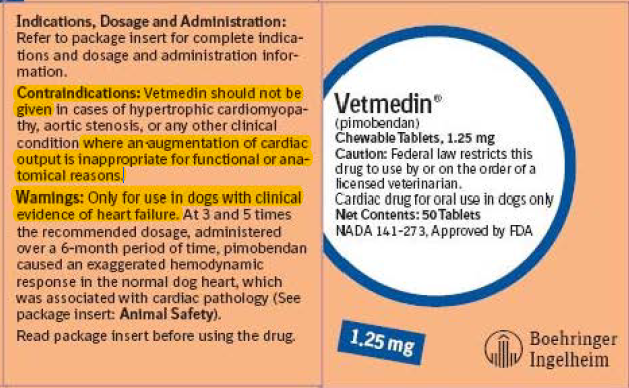 Prior to release of the EPIC Study report, the universally recommended use of
pimobendan had been limited to MVD-affected dogs only after they reached
CHF. The reasons for delaying the start of pimobendan treatment until the
dogs reached CHF has been due to prior peer-reviewed veterinary studies
finding harmful side-effects if the dogs were treated before the need for
the positive inotropic support of their hearts' contractility,
which pimobendan provides.
Prior to release of the EPIC Study report, the universally recommended use of
pimobendan had been limited to MVD-affected dogs only after they reached
CHF. The reasons for delaying the start of pimobendan treatment until the
dogs reached CHF has been due to prior peer-reviewed veterinary studies
finding harmful side-effects if the dogs were treated before the need for
the positive inotropic support of their hearts' contractility,
which pimobendan provides.
Specifically, these articles warned about the hazadous downsides of pre-CHF administration of pimobendan:
In "Comparative adverse cardiac effects of pimobendan and benazepril monotherapy in dogs with mild degenerative mitral valve disease: a prospective, controlled, blinded, and randomized study", published in 2007 in the Journal of Veterinary Internal Medicine, the researchers found that "PIMO has adverse cardiac functional and morphologic effects in dogs with asymptomatic MVD."
In "Increased Mitral Valve Regurgitation and Myocardial Hypertrophy in Two Dogs With Long-Term Pimobendan Therapy", published in 2005 in Cardiovascular Toxicology, the researchers concluded "This is the first report to describe an increase in mitral regurgitation under clinical conditions in dogs treated with pimobendan. We also suggest that pimobendan may induce ventricular hypertrophy."
In Cardiac Care for Pets (CVCA) "Pimobendan- A Silver Bullet?", published in May 2009, the cardiology department stated: "In a small study performed by CVCA, it was determined that after two to three weeks of Pimobendan therapy about 75% of dogs had an increased frequency of ventricular arrhythmias documented on 24 hour ambulatory ECG monitoring."
In the U.S. Food and Drug Administration's (FDA) 2007 report approving the use of pimobendan for dogs, it stated this conclusion in a four week toxicity study of pimobendan administered to 30 previously healthy lab Beagles:
"Conclusions: Pimobendan administered IV daily to healthy Beagles caused dose dependent increases in heart rate, mitral valve myxomatous thickening, left ventricular outflow tract endocardial thickening, and ventricular muscle ischemic lesions (multifocal subendocardial necrosis and scarring). The cardiac pathology seen in these dogs is typical of positive inotropic drug toxicity in normal dog hearts, and is related to the physiologic effect of the drug on contractility and exaggerated hemodynamic response."On Vetmedin's website, it had this warning: "The safety of VETMEDIN has not been established in dogs with asymptomatic heart disease."
Additionally, veterinary cardiologists spoke out against the pre-CHF use of pimobendan:
Dr. Amara Estrada warned: "There is evidence that treatment with a positive inotropic agent such as pimobendan prior to the development of systolic myocardial failure can have deleterious effects. ... Pimobendan ... should be reserved for use when systolic myocardial failure is detected or suspected."
Dr. George A. Kramer warned: "Most dogs with chronic heart disease do not have decreased contractility and do not need positive inotropic support."
Dr. Mark Rishniw warned: "One study in dogs with early mitral valve disease suggested an increase in valve damage in the dogs give pimobendan."
Dr. Mark Kittleson, referring specifically to the EPIC trial while it was ongoing, warned:
"Because this study found pimobendan to be detrimental to dogs with MMVD it is the opinion of the author that further study was warranted prior to exposing 150 dogs to it in a large clinical trial (the EPIC study). Primum non nocere (first do no harm). It is also the opinion of the author that pimobendan should not be administered to dogs with MMVD prior to the onset of heart failure until the results of the EPIC trial are published. ... Will it prolong the time until a dog with MMVD goes into heart failure? That remains to be seen. Given the one study that has been done to date I don't believe you can give this anything more than a 50:50 chance."
Notice that the main focus of these warnings is about the damage that pimobendan could do to the hearts of pre-CHF dogs which are not in a depressed contractile state and therefore do not need the additional positive inotropic support which is the primary benefit of pimobendan. The measure of the need for positive inotropic support typically is determined by calculating left ventricle performance by such means as the ejection fraction or the fractional shortening percentage (FS%). While the baseline FS% of the dogs in the EPIC trial were calculated before administration of pimobendan began, no minimum or maximum FS% was a criterion in selecting or excluding the dogs for the trial, and there is no indication from the final report that any subsequent FS% measurements were taken. The initial median FS% were 43 (39-48) for the pimobendan dogs and 44 (41-49) for the placebo dogs.
Despite all of these warnings from peer-reviewed articles and board certified cardiologists (cited above), the EPIC trial was designed from the beginning to ignore the FS% as a parameter for the dogs to qualify for the study. The designers of the study were willing to take the risk - a risk to be borne by the pimobendan dogs - that these dogs would survive the trial nonetheless. They were intentionally flying blind.
The qualifications for dogs to be in the EPIC trial
The actual qualifications which the dogs had to meet were these: (a) A dog had to be 6 years of age or older; (b)have a mitral valve murmur of at least Grade 3 of 6; (c) have echocardiographic evidence of advanced MVD consisting of characteristic valvular lesions of the mitral valve, regurgitation through the mitral valve (MR) on the color Doppler echocardiogram, and have echocardiographic evidence of left atrial and left ventricular dilatation. All dogs entering the study met or exceeded three different heart size criteria. They are, first, the left atrial-to-aortic ratio (LA/Ao) equal to or greater than (>) 1.6. Second, the normalized left ventricular internal diameter in diastole (LVIDDN) > 1.7. Third, radiographic evidence of enlargement with a vertebral heart score (VHS) >10.5.
As discussed below and also in more depth in a later blog article, all three of these parameters appear to have been selected arbitrarily and without any published data justifying them as indicating that the dogs' hearts would actually be enlarged. "Pseudo-science" is defined as the assertions of alleged scientific data but which are unsupported by empirical evidence. By any standard, the definition of an enlarged heart in this study is a textbook example of pseudo-science.
The unfortunate March 2015 press releases (advertisements)
 The actual clinic phase of the trial for the 360 dogs started in early
2012 and was intended to last for three years, ending in early 2015. In
March 2015 (notably early 2015), the three lead researchers quite surprisingly issued three press
releases (two were identical) in which they announced that, because of an
interim analysis that was performed in February, the trial was being ended
"early". (In fact, the study was nearly 90% complete by then.) The press releases boldly stated:
The actual clinic phase of the trial for the 360 dogs started in early
2012 and was intended to last for three years, ending in early 2015. In
March 2015 (notably early 2015), the three lead researchers quite surprisingly issued three press
releases (two were identical) in which they announced that, because of an
interim analysis that was performed in February, the trial was being ended
"early". (In fact, the study was nearly 90% complete by then.) The press releases boldly stated:
"A global clinical trial ... has found evidence of benefit of the drug pimobendan for dogs with mitral valve disease."
"The interim analysis indicated that there was clear evidence of benefit of the administration of pimobendan in prolonging the time to the primary endpoint of the study, which was a composite of the development of left-sided congestive heart failure, or death presumed to be cardiac in origin. The interim analysis did not raise any concern over the safety of pimobendan administration." (Link)
"A mid-study analysis in mid-February 2015 indicated that pimobendan is clearly beneficial and did not raise any concern over the administration of pimobendan." (Link)
While the March 2015 press releases concluded with this statement - "Full and final results of the study are expected at a later date." - the releases notably did not include the list of initial qualifications which the dogs in the trial needed to meet. So, while the readers of these press releases - essentially advertisements for the drug - knew of the success of prescribing pimobendan prior to heart failure, they were not told what the parameters needed to be to start the drug.
For eighteen months, from mid-March 2015 until September 28, 2016 when the EPIC Study report was published, all anyone not involved in the study knew was that pimobendan worked on pre-CHF dogs with MVD and some heart enlargement. And hundreds of veterinarians, including cardiologists, presumably fell for it, by prescribing pimobendan to asymptomatic MVD-affected dogs, without having any idea of what the dogs' actual minimum echocardiographic and radiographic parameters needed to be.
What the final report DOES say
So now that the final report is out, what do the EPIC Study results show?
Well, for sure, the end result has not
 disappointed pimobendan's
manufacturer, in the least.
disappointed pimobendan's
manufacturer, in the least.
First of all, the researchers warn that:
"... it should be borne in mind when interpreting these results that all dogs included in the analyses also met the echocardiographic inclusion criteria and these results therefore might not be generalizable to all dogs with a VHS > 10.5 in the absence of concurrent echocardiographic measurements and a confirmed diagnosis of MMVD."
Therefore, to apply the results of this study to future treatment of MVD-affected dogs, an x-ray of the heart showing a VHS value over 10.5 is not sufficient by itself, and that the two echo measurements must also be confirmed.
Of 354 dogs in the study, 161 (45.5%) were cavalier King Charles spaniels (CKCS) -- the largest breed group. Therefore, the results of this study obviously are of supreme importance to owners of cavaliers. Of those 354 dogs, 178 of the dogs were treated with pimobendan (77 CKCSs), and 180 received the placebo (81 CKCSs). Of those 178 dogs treated with pimobendan, 59 (33.1%) reached congestive heart failure (CHF), 15 (8.4%) died of cardiac-related deaths during the treatment. The others had not reached CHF by the time the study ended. Unfortunately, the report does not tell us how many cavaliers were in any of these categories.
Median time to the "primary endpoint" (CHF or death) was 1228 days in the pimobendan group and 766 days in the placebo group. Dogs in the pimobendan group lived longer, with a median survival time of 1059 days in the pimobendan group and 902 days in the placebo group. But, the study does not tell us how many of those deaths were attributable to MVD. Surely they have that information. Why they have failed to include it in their report is mystifying.
As for the dogs which died prior to reaching CHF, the authors explained that:
"Although a greater number of dogs in the pimobendan group experienced spontaneous cardiac death (12 versus 5), the proportion of dogs in each group experiencing this event was not significantly different."
The report concludes:
"Chronic oral administration of pimobendan to dogs with echocardiographic and radiographic evidence of cardiomegaly secondary to MMVD, in the absence of concurrent cardiovascular medication, results in the prolongation of the preclinical period, and is safe and well tolerated. The median time to the onset of CHF or cardiac-related death was prolonged by approximately 15 months, and the risk of a dog experiencing this event was reduced by approximately one-third; the majority of the benefit observed was attributable to delaying the onset of CHF. This substantial degree of prolongation of the preclinical period is f clinical relevance and is of importance to veterinarians and owners of dogs affected by this common disease."
So, the bottom line is:
(1) The dog must be in Stage B2 of mitral valve disease; AND
(2) Have a murmur of at least Grade 3; AND
(3) The dog must NOT be on any other cardiac medication; AND
(4) An echocardiogram must be conducted and show valvular lesions of the mitral valve, regurgitation through the mitral valve (MR) on the color Doppler echocardiogram, and have echocardiographic evidence of left atrial and left ventricular dilatation (defined as a left atrial-to-aortic root ratio [LA/Ao] equal to or greater than 1.6 and body weight normalized left ventricular internal diameter in diastole [LVIDDN] equal to or greater than 1.7); AND
(5) X-rays most be obtained, showing evidence of enlargement with a vertebral heart score (VHS) value greater than 10.5.
This essentially means that once the MVD-affected dog develops a Grade 3 murmur and an x-ray showing enlargement, the owner should have a board certified veterinary cardiologist perform a thorough echo exam.
The BAD and the UGLY!
- (1) Parameters measure size, not enlargement
- (2) Parameters are arbitrary and unsupported
- (3) CKCSs have normal hearts above VHS 10.5 value
- (4) Heart-healthy CKCS has a LA/Ao ratio way below 1.6
- (5) All Stage B2 sub-groups are lumped together
- (6) Recommended parameters ignored study's data
- (7) Study glosses over pimo causing sudden deaths
- (8) Report hides categories of pimo-caused adverse events
- (9) Early termination leads to risk of false positives
- (10) Study ignores contractility and systolic functions
- (11) Report excludes data of pimo shortening life spans in CHF
- (12) Report provides no breed-specific information
- (13) Authors try to defend manufacturer's control over them
- (14) Report contradicts earlier, misleading press releases
But what is most disturbing is what is not in the EPIC Study report.
We know the cherry-picked GOOD news -- that pre-CHF
 dogs which are treated with pimobendan
and are were lucky enough not to die, could stave off the CHF much longer
than dogs on sugar pills. But what about the BAD and the UGLY? The report
is loaded with unanswered questions. Notable
examples of the BAD and the UGLY:
dogs which are treated with pimobendan
and are were lucky enough not to die, could stave off the CHF much longer
than dogs on sugar pills. But what about the BAD and the UGLY? The report
is loaded with unanswered questions. Notable
examples of the BAD and the UGLY:
• (1) The three parameters focus on heart size instead of heart enlargement. By specifying species-wide measurement parameters (VHS >10.5; LA/Ao > 1.6; LVIDDN > 1.7), the researchers arbitrarily assume that any dog with measurements which equal or exceed those minimum parameters necessarily must have an enlarged heart. They amount to "decision thresholds" made without any scientific basis whatsoever. They ignore the rule that veterinarians should treat the dog and instead advise to treat the measurement. These minimum criteria are an example of what veterinary researchers call "quantitative measurement methods", which are designed to dumb-down the level of professionalism which one otherwise would expect from both investigative and clinical veterinarians in performing their examinations.
• (2) The three parameters are arbitrary and are unsupported by their cited authorities. Each of the three species-wide measurement parameters (VHS >10.5; LA/Ao > 1.6; LVIDDN > 1.7) have a citation to a previous veterinary research article, leading the reader to assume that the cited article supports the EPIC Study investigators' selection of those specific parameters. Unfortunately, none of the cited articles provide any such support. The lead investigators' definition is nothing more than an hypothesis which they never bother to test.
VHS > 10.5 -- For example, the Study's x-ray parameter of the vertebral heart score (VHS), "radiographic evidence of cardiomegaly (vertebral heart sum (VHS) > 10.5)" is attributed to a March 2005 article in which the 2005 researchers studied 50 sets of heart x-rays of only one breed - ironically our breed, the cavalier - and found that a VHS value of 10.8 ± 0.49 in cavaliers was "normal", meaning that those dogs' hearts were not enlarged at all. So, we have the EPIC Study authors assume that any dog with a VHS value of >10.5 must have enlargement, while citing as authority for that assumption an article which found that CKCSs with a significantly higher VHS value of 10.8 (and up to 11.29) had no enlargement at all. This is known in the world of scientific research as "citation bluffing", and the EPIC Study report is replete with examples of it. The authors of the 2005 article ironically stated:
"The mean VHS for normal cavalier King Charles spaniels was 10.8 ± 0.49 v (10.0-11.4). ... The use of breed-specific VHS values is needed for the VHS method to have a high specificity for normal heart size."
Actually, in an audio interview (at time 31:24) in November 2016, lead investigator, Dr. Adrian Boswood, admitted that the EPIC Study's VHS parameter of > 10.5 was too low to amount to heart enlargement for some breeds. He said:
"A vertebral heart score of 10.5 is in the normal range for some dogs, particularly cavaliers actually."
As stunningly dismissive of the authenticity of the EPIC Study's VHS parameter as Dr. Boswood is in this quote, this is not the only mocking comment he made about its parameters in just this one interview. More to come later. One can only imagine what he may have to say about the study off-mic.
Another of the EPIC Study's three lead investigators, Dr. Sonya Gordon, wrote in a June 2017 article:
"However, given the potential low accuracy of depending solely on a radiographic VHS greater than 10.5, ... and that there are known breed-related differences in normal VHS reference ranges with much higher normal VHS ranges reported in some breeds, including the CKCS, ... ."
Note that both comments indicate the lead investigators' complete lack of concern about possibly placing our breed, the cavalier King Charles spaniel, at great risk by administering pimobendan to several CKCSs prematurely for several years. Nearly half of the 360 dogs were cavaliers.
In 2019, Dr. Gordon went even further in demeaning her own VHS cut-off value. In fact, she went so far as to question using a value of 11.5 as the species-wide cur-off when she wrote:
"Several reports and publications have suggested a VHS > 11.5 may be predictive of EPIC echocardiographic inclusion criteria (now ACVIM Stage B2) in dogs with MMVD, however this cutoff is based on small sample sizes, or was made based on inferences from other publications."
So that amounts to two out of three lead investigators who pooh-pooh their study's own VHS parameter. (We have not heard from Dr. Haggstrom yet, but he was one of the authors of that March 2005 article about cavaliers with normal hearts at VHS value 10.8 and higher.) When a study's lead investigators do not control their study's inclusion parameters, you must wonder who really is in charge of the study. Could it be the sponsor?
LA/Ao > 1.6 -- The EPIC Study authors selected the single line measurement of left atrium size, called the "left atrial-to-aortic root ratio (LA/Ao)" as the sole echocardiographic measurement of the left atrium in determining both the LA's size and whether or not it is enlarged. This method has been discredited in published veterinary journal articles since 2014. See this July 2014 article, for example.
The EPIC Study's authors attribute their choice of the LA/Ao parameter of > 1.6 to a November 2002 article (Dr. Haggstrom was an author of that study, too) which found the CKCSs that had mitral regurgitation (MR) had an LA/Ao ratio of 1.61 ± 0.57. That range of measurements included cavaliers which had no heart enlargement at all. More citation bluffing.
Dr. Haggstrom and the other authors of the 2002 study warned against applying these measurements for cavaliers to any other breeds, much less species-wide. They stated:
"The 2-D method can be used for any breed, but direct extrapolation of our normal values should not be made to other breeds, because the heart has a slightly different appearance in various breeds reflecting variability in size, shape, and position within the thorax."
The 2002 study's authors also were careful to exclude any findings comparing LA/Ao ratios of dogs with and without enlarged hearts. Since the 2002 article made no distinction between MVD-affected dogs with and without enlargement, that LA/Ao ratio data was irrelevant to the EPIC Study. The 2002 article authors stated:
"In this study, we have deliberately refrained from introducing index ranges for mild, moderate, and severe enlargement, because the grading would be arbitrary and was not included in the study design."
The EPIC Study authors ignore all of those cautions against applying the 2002 study's findings to any other breed. Thus, what would be "arbitrary" to the authors of the 2002 study (and therefore should be excluded) now, in the EPIC Study report, is "top tier" (as Dr. Boswood immodestly has described it).
In addition, in that previouly referenced audio interview, Dr. Boswood raised the prospect of clinicians frequently mis-calculating the LA/Ao ratio. He said (at 30:40):
"Everyone knows you can get an inaccurate single measurement of left atrium to aortic ratio -- over-estimated. The dog goes on to treatment it didn't need."
Nevertheless, this minimum measurement of left atrial enlargement appears to be widely accepted by veterinary cardiologists, in addition to those in the EPIC Study.
LVIDDN > 1.7 -- The EPIC authors attribute their "body weight normalized left ventricular internal diameter in diastole (LVIDDN)" parameter of > 1.7 to a May 2004 article (another one co-authored by Dr. Haggstrom) which in no way states that > 1.7 signifies heart enlargement. In fact, the 2004 article does not deal with MVD at all.
In that same audio interview (at time 31:06) in November 2016 that is noted above, Dr. Boswood admitted that the LVIDDN of 1.7 also is below the range for enlargement. He said:
"Now interestingly, if you look in the literature, the normalized left ventricular diameter of 1.7 is in the normal range. The abnormal is above about 1.85, [1.]9, 1.9 depending upon how you read it, so that's nudging the top of the normal range but still normal."
Perhaps Dr. Boswood was referring to the normal LVIDDN range as high as 1.85 reported in this widely-cited 2004 article, in which its authors stated:
"If the result is between 1.27 and 1.85, the value is within the normal [95%] prediction interval for this study." (Emphasis added.)
EPIC lead investigator Sonya Gordon made a similar admission in a 2017 article when she and her co-authors wrote:
"In addition, all dogs with stage B2 MMVD were required to have a left ventricular internal dimension (LVID) in diastole normalized to body weight 1.7. The selected cutoff value for normalized LVID in diastole was based on a study that found higher values, although technically within the normal reported range (<1.85), predicted increased risk of death in dogs with MMVD." (Emphasis added.)
So, to Dr. Gordon, Stage B2 has nothing to do with heart enlargement.
So much for the "validity" of the LVIDDN measurement. Drs. Boswood and Gordon have demonstrated by their own words that these inclusion parameters were never intended to bear any relationship to dogs which actually had enlarged hearts.
Additionally, in a June 2022 article, Dr. Mark Rishniw and Dr. Donald J. Brown concluded that the EPIC definition (LVIDDN > 1.7) was "arbitrarily chosen", and they single out five specific breeds, including the CKCS, as having larger LVs than average dogs of similar size. They state:
"The EPIC study employed an essentially arbitrary value of LVIDDN to dogs subsequently randomized to treatment with pimobendan or placebo and showed that dogs with LVIDDN>1.7 (and LA:Ao>1.6 and a VHS>10.5V) generally do better with the drug than without. ... The criterion for left ventricular enlargement used by the EPIC investigators for study inclusion has never been critically evaluated as indicative of left ventricular enlargement. ...
"We should note, however, that the definition of LV enlargement proposed by ... the EPIC trial ... is not a reference value, but a somewhat arbitrarily chosen threshold for inclusion in the EPIC trial. Therefore, clinicians adhering to these guidelines should be cautious in ascribing LVIDDN that exceed the threshold value of 1.7 as being indicative of LV enlargement."
Drs. Rishniw and Brown warn that such breeds as the CKCS "likely require breed-specific reference intervals for LVIDDN to correctly identify left ventricular enlargement." They also point out:
"For example, if a dog has a LVIDDN that consistently oscillates around 1.3 (within 0.1 units), an increase to 1.6 could indicate left ventricular enlargement for that dog, despite being within the population-based reference interval."
Since none of the citations relied upon by the EPIC Study authors in fact support the three minimum parameters they have selected, we must wonder whether the authors even bothered to read the articles they have cited (and all of which Dr. Haggstrom co-authored). It appears that the normal range VHS and LVIDDN parameters were chosen intentionally, since Dr. Boswood admitted their inaccuracies in his November 2016 audio interview. In short, it appears that these three parameters were just concocted arbitrarily. Or perhaps they were selected to better insure reaching the magic participation number of 360 dogs -- regardless of whether their hearts really were enlarged or not -- to reach that "top tier" goal.
Did the EPIC Study investigators perform any subjective analysis to confirm whether the participating dogs actually had enlarged hearts? In other words, did they thoroughly examine the x-rays, as a cardiac specialist would be expected to, and with their experienced eyes look for the classic signs of enlargement -- cardiomegaly -- such as the shape of the left atrium, or the overall cardiac appearance, or the appearance of the vascular structures? Apparently not. They certainly did not state as much in their report.
Because the EPIC Study's inclusion criteria were irrelevant to Stage B2, and no independent, subjective determinations of heart enlargement were performed, no one will ever know how many - or if any at all - of the 360 dogs in that study had enlarged hearts when the testing commenced. All that is known for certain is that all of the dogs in the study started out somewhere in Stage B, and based upon the study's liberal inclusion criteria, many of them very well could have been Stage B1 dogs.*
Since no effort was made to determine which of the 360 dogs in the study actually had any enlargement and actually were in Stage B2, likewise no effort was made to determine how many of those Stage B2 dogs were in the pimobendan group and how many in the placebo group. Presumably it would take a dog without enlargement a significantly longer time to reach heart failure than it would a dog with enlargement. If a higher percentage of the dogs without enlargement were in the pimobendan group than in the placebo group, then the median times for the dogs to reach heart failure would be skewed and the results meaningless. This is an obvious, fundamental flaw in this so-called "top tier" study.
* The incredible disconnect between the EPIC Study's inclusion parameters and dogs which may actually have had any heart enlargement makes us wonder whether these were not the original parameters selected by the lead investigators. Could they have started out with some realistic parameters which they subsequently felt the need to abandon because they had fallen several months behind their two-year recruitment phase goal to enlist 360 dogs with enlarged hearts?
• (3) The average heart-healthy cavalier has a VHS value way above 10.5. It is troubling that the EPIC Study report fails to note that normal, heart-healthy cavaliers may have VHS measurements as high as 11.7*, which is notably higher than the >10.5 criterion for beginning pimobendan treatment. Considering that nearly half of the dogs in the study were CKCSs, this oversight is rather inexplicable and potentially life-threatening. This is especially true since, as noted above, Dr. Boswood admitted that:
"A vertebral heart score of 10.5 is in the normal range for some dogs, particularly cavaliers actually."
* Lamb CR, Wikeley H,
Boswood A, Pfeiffer DU.
Use of breed-specific ranges for the vertebral
heart scale as an aid to the radiographic diagnosis of cardiac disease in
dogs. Vet Rec. June 2001;148(23):707-11. Hansson K, Haggstrom J, Kvart
C, Lord P.
Interobserver Variability of Vertebral Heart Size
Measurements in Dogs with Normal and Enlarged Hearts.Veterinary Rad. &
Ultrasound, Marc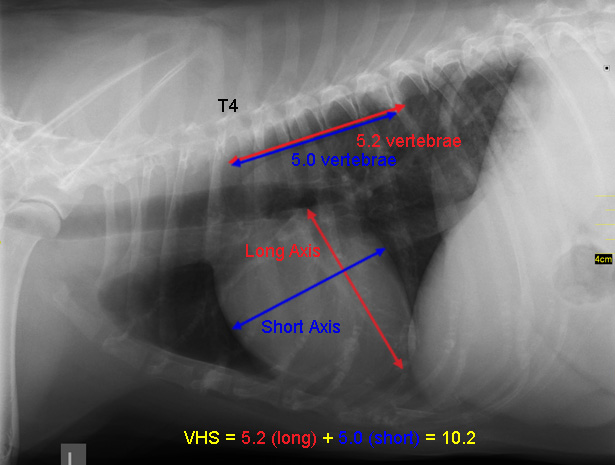 h 2005, 46(2): 122.
h 2005, 46(2): 122.
In other studies, the boxer (12.6), Labrador retriever (11.7), greyhound (10.6), beagle (10.7), whippet (11.8), pug (14.1), Pomeranian (11.4), bulldog (14.4), Boston terrier (13.1), and dachshund (11.0), were found to have normal VHS values above 10.5.
Bizarrely, the researchers' footnoted citation justifying this VHS score is an article which expressly states:
"The use of breed-specific VHS values is needed for the VHS method to have a high specificity for normal heart size."
It previously has been customary when cardiologists determine heart enlargement using VHS values, to compare the current x-ray with previous ones, such as a baseline x-ray. Indeed, the ACVIM's 2009 Consensus Statement specifically recommends, for Stage B dogs, to obtain baseline x-rays. It states:
"Thoracic radiography is recommended in all patients to assess the hemodynamic significance of the murmur and also to obtain baseline thoracic radiographs at a time when the patient is asymptomatic for CVHD."
Therefore, it is perplexing as to why this EPIC Study, being hyped as "top tier" by its boastful chief lead researcher, ignores breed-specific VHS values (which the same researcher previously had recommended as "needed for the VHS method to have a high specificity"), and establishes an unfounded and abnormal parameter for the cavalier King Charles spaniel. More importantly for cavaliers, it ignores the individual patient's specific VHS value compared to the dog's baseline x-ray.
There is nothing "top tier" about a study which ignores the basic research principle that differences likely influenced by genetic factors should be taken into account when designing clinical trials, and also most particularly in this instance, when making recommendations about parameters to be followed by clinicians hereinafter.
But if the manufacturer's goal is to sell more pills, then reducing the threshold VHS value to significantly below the average score of a healthy cavalier, will do just that -- sell more pills. Let's face it, the CKCS breed will be its biggest customer.
• (4) The average heart-healthy cavalier has a LA/Ao ratio way below 1.6. A 2014 study of 134 cavaliers with healthy hearts showed a LA/Ao range from 0.47 to 0.94.* This could mean that if the cut-off ratio between a normal-sized CKCS left atrium and an enlarged one is arbitrarily assumed to be 1.6, then cavaliers with acutal enlarged atriums but with LA/Ao ratios as low as 0.95 and as high as 1.59 would not be treated with pimobendan when they should be regarded as in Stage B2 and therefore should be prescribed the drug.
* Charlotte Mishbach, et al., Echocardiography and conventional Doppler examination in clinically healthy adult Cavalier King Charles Spaniels: Effect of body weight, age, and gender, and establishment of reference intervals. J. Vet. Cardiol. 2014;16(2):91-100.
• (5) The study does not distinguish between the various sub-groups of Stage B2 mitral valve disease. All that Stage B2 defines is mitral regurgitation (MR) with enlargement of the left side of the heart. But, Stage B2 does not distinguish between mild MR and severe MR. Also, Stage B2 does not distinguish between mild, moderate, or severe enlargement. Statistically, up to 70% of dogs with mild MR will likely never go into heart failure, while dogs with severe MR will almost certainly go into heart failure. Treating that 70% of dogs with mild MR with the inordinately costly pimobendan is both unnecessary and a textbook example of "overdiagnosis"*.
* Brennen A. McKenzie. Overdiagnosis. JAVMA. October 2016;249(8):884-889 ("Overdiagnosis can cause waste and misallocation of medical resources and can also increase morbidity and mortality rates and have a deleterious psychological impact on individual patients and their caregivers. The testing leading to overdiagnosis and the subsequent follow-up testing and treatment have obvious financial costs.").
Dr. Mark Rishniw provides this analysis of the EPIC Study's Survival Chart (below), a classic divergent-parallel curve model:
"If we assume that the survival curve is in some way an estimate of the initial disease severity, then the most severely affected dogs are in the upper left corner, and the least severely affected dogs are in the lower right of the curve. As an analogy, if you have bad disease, you are probably going to die from it. If you have mild disease, you are likely to keep living for years and years. Now, if there was a clear benefit of 'earlier' rather than 'later,' we might expect the survival curves to diverge, ie., continue to move further and further apart. But they don't. For the majority of the study, they remain parallel. So, the benefit with more severely affected dogs is about 300 days, and the benefit with the least severely affected dogs is about 300 days. This suggests that taking the more measured approach of waiting until a dog exhibits evidence of disease progression before instituting therapy is not compromising that dog nor reducing the benefit of the drug. And, dogs that were never going to progress to more severe disease and never develop CHF would not be subjected to needless drug administration (and needless expenses)."
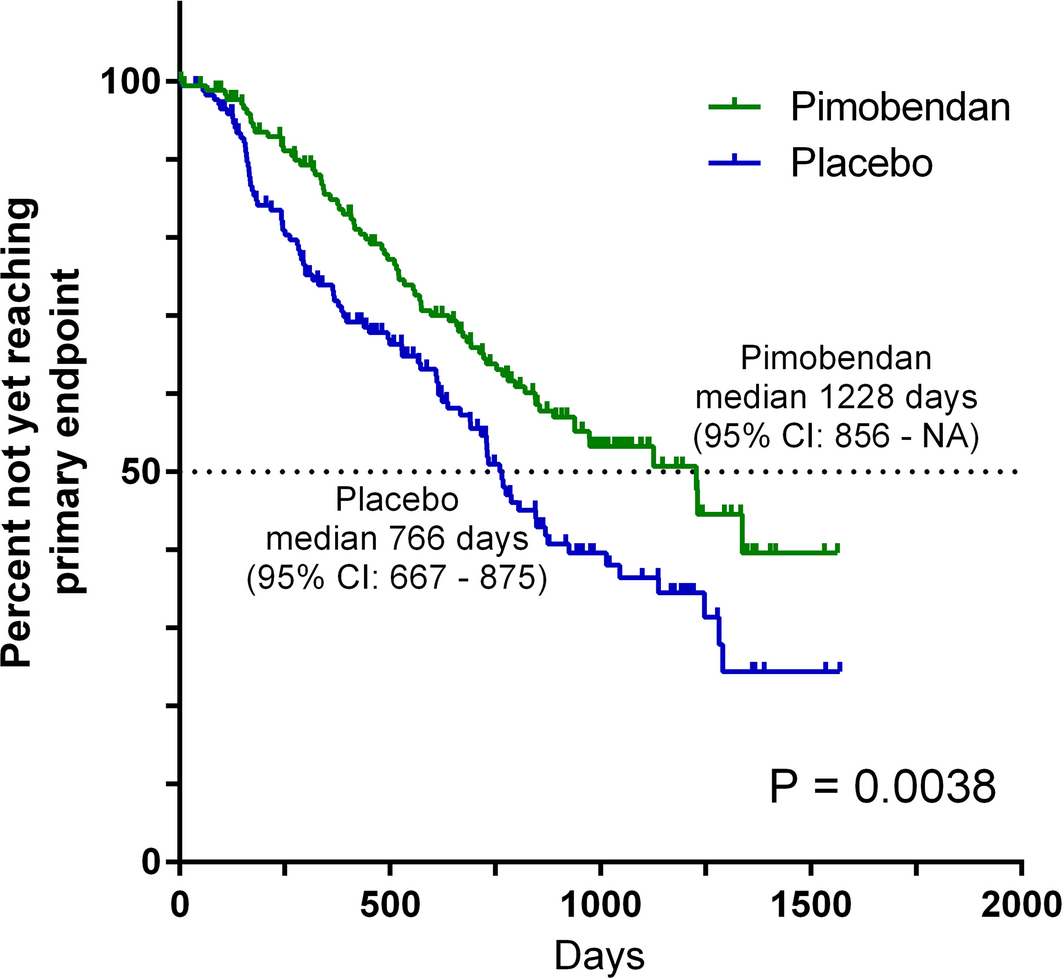
• (6) The final recommended x-ray and echo measurement parameters were set at the outset of the study, rather than scientifically determined as a result of the study. Since the conclusion of the EPIC Study includes very precise minimum heart measurement criteria (VHS >10.5; LA/Ao > 1.6; LVIDDN > 1.7), one would have hoped that the researchers made those determinations by a careful analysis of the results of the study. But, no, the exact opposite was the case. The lead researchers made up those parameters before the study even began. The Study's "enrollment criteria" were:
"To be eligible for inclusion, a dog had to ... have echocardiographic evidence of left atrial and left ventricular dilatation, defined as a left atrial-to-aortic root ratio (LA/Ao) > 1.6 and body weight normalized left ventricular internal diameter in diastole (LVIDDN) > 1.7, in addition to radiographic evidence of cardiomegaly (vertebral heart sum (VHS) > 10.5)."
And they did not re-visit those parameters after the study ended, to determine if their initial determinations are safe and otherwise appropriate. Their final recommended parameters remained the same:
"The conclusions of this study are only relevant to dogs with cardiac enlargement secondary to preclinical MMVD (stage B2) as all dogs entering the study met or exceeded 3 different heart size criteria (LA/Ao > 1.6, LVIDDN > 1.7, and VHS > 10.5) ... ."
The fact is that all three of those parameters appear to have been chosen arbitrarily and without regard to whether the dogs' hearts actually were enlarged (as noted above). Therefore it would be flagrantly irresponsible to end the EPIC Study by recommending that the same bogus parameters be used hereinafter on all MVD-afffected dogs. But, that is what the investigators have done.
Despite the study's overwhelming empirical evidence that the enrollment crtieria do not define enlargement and therefore should not be followed by clinicians in diagnosing patients, the study's authors conclude by actually recommending that their bogus definition of enlargement be followed when prescribing their benefactor's medicine.
Because the EPIC Study's inclusion criteria were irrelevant to Stage B2, and no independent, subjective determinations of heart enlargement were performed, no one will ever know how many - or if any at all - of the 360 dogs in that study had enlarged hearts when the testing commenced. All that is known for certain is that all of the dogs in the study started out somewhere in Stage B, and based upon the study's liberal inclusion criteria, many of them probably were Stage B1 dogs. But the worst thing about the EPIC Study is that, since its inclusion parameters have also become its recommended treatment protocol, many MVD-affected dogs only at Stage B1 will be prescribed pimobendan from now on. (And for some other breeds, they will be denied medication because, like the CKCS, their normal LA:Ao ratio maxes out far below the 1.6 cut off between normal and enlarged.)
• (7) The study glosses over pimobendan causing sudden deaths.
It also is
disappointing that the study
 does not go into any details about 8.4% of dogs
being treated with pimobendan and which suffered cardiac-related deaths while only in Stage B2.
(See excerpt from the study's Fig. 1, below.) While the authors do
acknowledge that "concerns had previously been raised about possible
detrimental effects of the administration pimobendan to dogs with
preclinical MMVD", they provide nothing to explain why pimobendan played a
role in those sudden and unexpected Stage B2 deaths. To the contrary, they
seem to be patting themselves on the back for even including any data at all on
these premature cardiac deaths, stating:
does not go into any details about 8.4% of dogs
being treated with pimobendan and which suffered cardiac-related deaths while only in Stage B2.
(See excerpt from the study's Fig. 1, below.) While the authors do
acknowledge that "concerns had previously been raised about possible
detrimental effects of the administration pimobendan to dogs with
preclinical MMVD", they provide nothing to explain why pimobendan played a
role in those sudden and unexpected Stage B2 deaths. To the contrary, they
seem to be patting themselves on the back for even including any data at all on
these premature cardiac deaths, stating:
"If our primary endpoint had focused exclusively on the onset of CHF, with dogs that died being censored, it might have appeared that we were choosing to ignore potentially detrimental effects of the treatment."
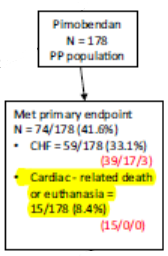 Well, it certainly does appear that they have chosen to ignore those
detrimental effects. Instead, they minimize these premature deaths of
pimobendan-treated dogs by stating:
Well, it certainly does appear that they have chosen to ignore those
detrimental effects. Instead, they minimize these premature deaths of
pimobendan-treated dogs by stating:
"We found, not unexpectedly, that only a small number of dogs met the primary endpoint in this way. Although a greater number of dogs in the pimobendan group experienced spontaneous cardiac death (12 versus 5), the proportion of dogs in each group experiencing this event was not significantly different."
In a January 2008 article, an Italian team of researchers, led by Dr. Michele Borgarelli, studied 558 MVD-affected dogs among 36 breeds, with various degrees of mitral valve regurgitation. In that study, 8.9% of the dogs died of inexplicable sudden death. This percentage so shocked the veteran investigators that they made this comment:
"The finding of sudden death in 8.9% is noteworthy. To the authors' knowledge, this is the first time sudden death has been reported in asymptomatic dogs with CMVI [chronic mitral valve disease]."
In that 2008 study, a survival analysis was performed on all causes of deaths and on cardiac-related deaths separately. In the EPIC Study, the investigators express no surprise at all about the sudden deaths, and they counted the pre-CHF sudden deaths as only a meaningless, insignificant statistic.
Since the "inclusion parameters" for the dogs participating in the EPIC trial really had to have included some (if not all) MVD-affected dogs with normal-sized hearts (Stage B1) rather than enlarged ones (Stage B2) (see that discussion above in this article), it would have been helpful to know details about these corpses, including: (a) whether their hearts really were enlarged at all; (b) if so, how enlarged they were; and (c) how soon after starting pimobendan they suddenly dropped dead of cardiac events. Of course, no such data is reported.
In the EPIC trial, how many of the suddenly dead pimobendan group dogs were cavaliers? We are not told. What if all of the dead pimobendan dogs were cavaliers? (That is not so far-fetched, considering the unreasonably low VHS threshold of >10.5.) That would amount to 15.5% of all of the CKCSs in the pimobendan group. If 15.5% of the cavaliers in the pimobendan group died suddenly, would that make a "significant" difference to these researchers?
In a prior peer-reviewed study of 317 human patients, the researchers found that: "In both pimobendan groups combined the hazard of death was 1.8 times higher than in the placebo group", and those researchers made a big deal of that finding. In this EPIC Study, the death hazard of pimobendan was 1.3 times higher than the placebo group, and the EPIC Study researchers just blow that significant fact off like it does not matter a whit.
How can they conclude that pre-CHF dosing of pimobendan "is safe and well tolerated", when nearly 10% of the dogs died cardiac-related deaths suddenly while being given pimobendan, and the researchers made no effort to find out those dogs' precise causes of death? Well, that is what the manufacturer wanted them to conclude. "Safe and well tolerated" was one of the two main goals for the EPIC Study. So, by minimizing the significance of all of the pimobendan-caused sudden deaths, that goal of "safe and well tolerated" has been attained.
But when it came to analyzing the untidy fact of sudden cardiac deaths, a sense of scientific rigor was not in these researchers' wheelhouse. When asked in a November 2016 audio interview about why dogs which died during the EPIC Study were not examined, lead investigator Dr. Adrian Boswood's response was very telling and disturbing. He said (at time 39:15):
"It wouldn't help address our primary hypothesis. So, as a side study it would be nice to know but not need to know, and I think one of the things that you always have to bear in mind is kind of keep your eyes on the prize. Why are you doing this study? You're doing this study because you want to know if the drug prolongs the time to the onset of clinical signs. That's all that matters. Anything else is just a side matter." (Emphasis addded.)
This chilling comment says it all! The "prize" in this case would have been showing that pimobendan is "safe and well tolerated", and carefully analyzed causes of otherwise inexplicable sudden cardiac deaths prior to heart failure would have interfered with attaining that prize. Clearly, they could not allow these deaths of dogs taking Vetmedin to deter the investigators from their prize.
• (8) The report hides 124 "adverse events" affecting 45% of the pimobendan group dogs under the "other" category. Arrhythmias are a well-known side effect of the pre-Stage C administration of pimobendan in MVD-affected dogs, and in particular, are well known to cause sudden deaths in MVD-affected dogs. While the report concedes that 80 dogs in the 178-dog pimobendan group, amounting to 45% of that group, experienced 196 "adverse events" during the trial, it fails to disclose the number of those dogs which were found to have suffered arrhythmias. Only 72 events are specifically categorized (e.g., diarrhea, vomiting, anorexia, lethargy, tachycardia). The remaining 124 adverse events are lumped together and identified only as "other". Of course, it would be un-tidy to single arrhythmias out, in view of the high percentage of sudden deaths among the pimobendan group in the EPIC Study.
• (9) The study was terminated early, leading to a greater risk of a false positive finding, than if it was allowed to continue to the scheduled completion. While the "interim analysis indicated that there was clear evidence of benefit of the administration of pimobendan ...", that premature termination of the study conveniently risked that a false positive finding would result.
An interesting side-light to this early termination factor is that only 135 dogs really were involved in the study, from beginning to end, reaching heart failure. Not 360. Only 135. Of those, 59 were in the pimobendan group and 76 were in the placebo group. So, for a study that was heavily advertised as a 360-dog study lasting to heart failure, only 135 of them actually reached that endpoint.
• (10) The study ignored the affect of pimobendan on contractility and systolic function of the dogs' hearts. Despite the researchers acknowledging that "concerns had previously been raised about possible detrimental effects of the administration pimobendan to dogs with preclinical MMVD", they did not bother to report measurements of the contractility and/or fractional shortening of the dogs' hearts during the treatment period. Since prior peer-reviewed studies cited above have shown that "long-term administration of PIMO in dogs with asymptomatic MVD is associated with an increase in systolic function and, concomitantly, a progressive worsening of MVD with development of specific mitral valve lesions", this periodic measurement could have predicted (and presumably avoided) the sudden deaths among the pimobendan dogs. That is another messy little detail which would not have made the manufacturer very happy.
When a study engages in questionable research practices (QRPs) and ignores these previously detailed, scientifically determined
hazards of the premature administration of pimobendan (over-stimulating the
well-compensated heart's contractility), and instead the study is based upon
superficial appearances (a heart's linear dimensions exceeding arbitrary
minimums), that study can easily lead to
false positives.
 In such a case, it really does
not matter that the current study includes a larger number of dogs
than the previous clinical ones. What matters is the damage done -- and to
be done in the future -- because of the risks taken. The failure to examine
that damage -- in this case, the causes of death of nearly 10% of the dogs
in the pimobendan group -- aids and abets the potential for those false
positives. Minimizing the negative results points to a manufacturer-driven
study.
In such a case, it really does
not matter that the current study includes a larger number of dogs
than the previous clinical ones. What matters is the damage done -- and to
be done in the future -- because of the risks taken. The failure to examine
that damage -- in this case, the causes of death of nearly 10% of the dogs
in the pimobendan group -- aids and abets the potential for those false
positives. Minimizing the negative results points to a manufacturer-driven
study.
• (11) The report excludes the study's own evidence of pimobendan shortening life spans after CHF. While it is not at all clear in the published article, at the ACVIM conference in June 2016, where the results of this study were orally presented to attending cardiologists, it was reported that once the dogs reached CHF, the subsequent life spans of the pimobendan dogs were shorter than the life spans of the placebo dogs. It therefore suggests that once CHF develops, life expectancy actually shortens for dogs treated with pimobendan, relative to untreated dogs. In a January 2017 article, veterinary cardiologist Mikaela Mueller commented on this observation:
"Patients in the pimobendan group did not live as long as the placebo group after the onset of congestive heart failure, but overall survival time (all-cause mortality) was increased."
Oddly, the EPIC Study researchers have not included this information in their article, but that missing data raises the question of whether the shortened life span of CHF dogs treated with pimobendan during Stage B2 is due either to drug toxicity or to an acquired pharmacological tolerance to the pimobendan.
The report does state that, "The median time to death by all causes was 1059 days in the pimobendan group [83 dogs] and 902 days in the placebo group [103 dogs]". (Emphasis added.) But it fails to break out the numbers of dogs which died of MVD or MVD-related disorders. So, the data which the authors provide on this topic in their report is pretty much worthless, and they are silent on the topic which would have been most relevant: How much longer, or shorter, did pimobendan dogs live than did placebo dogs before dying MVD-related deaths?
One of the lead investigators. shortly after publication of the EPIC
Study, stated that, "We intend to publish at least one further paper
relating to the study, which will provide longitudinal follow up on dogs in
the study." That is well and good, of course, but unless that further paper
is published promptly, there will be another undue delay -- like the 18
month one between the March 2015 press releases and the report itself -- in
finding out what value pimobendan, if any, may have in extending the lives
of MVD-affected dogs. Meanwhile its
 manufacturer will be able to continue to bask in the
unsubstantiated hype and promises that pre-CHF administration of pimobendan
will not only delay the onset of heart failure, but also extend the
lifespans of the dogs. For example, that same lead investigator reportedly
told the
UK Telegraph in October 2016 that,
"This is a major breakthrough in
treatment and could extend the lives of dogs around the world."
"Could" is the operative word there, because no evidence
has been presented in the published report that pimobendan added to the
longevity of any dogs dying of mitral valve disease.
manufacturer will be able to continue to bask in the
unsubstantiated hype and promises that pre-CHF administration of pimobendan
will not only delay the onset of heart failure, but also extend the
lifespans of the dogs. For example, that same lead investigator reportedly
told the
UK Telegraph in October 2016 that,
"This is a major breakthrough in
treatment and could extend the lives of dogs around the world."
"Could" is the operative word there, because no evidence
has been presented in the published report that pimobendan added to the
longevity of any dogs dying of mitral valve disease.
• (12) The researchers provide no breed-specific information. There were 360 dogs in this study. Nearly half of them were cavalier King Charles spaniels. There were eight times more CKCSs in this study than any other breed. And yet, the report includes no data specific to cavaliers -- or to any other breed, for that matter. The authors had a year and a half after the conclusion of the trial, to sift through the data and analyze every aspect of them, before publication. But no breed-specific breakdown is to be found.
No breed is going to be more affected by this study than the CKCS. When we asked chief EPIC Study author Dr. Boswood to provide any breed-specific data or findings about cavaliers, his response was, in short, "No". He wrote:
"You have asked for data specifically about the outcome in the study for cavalier King Charles spaniels and suggested that we should perform a sub-analysis looking at outcome for this group. ... [W]e will not release the exact figures you have requested."
So you see, he has those "exact figures" about cavaliers from the EPIC Study, but he refuses to release them.
 The researchers
also ignored prior studies showing the
importance of using breed-specific heart measurements for that breed --
thereby placing the CKCS at greater risk than other breeds when taking the
drug prematurely. This is just about the least informative study of the
safety and effectiveness of any drug with a prior record of toxicity, in
this century. Why would experienced veterinary cardiology researchers ignore
their own prior warnings of the vital importance of breed-specific heart
measurements and also fail to calculate the breed-specific data they
collected in this study? Why have the researchers thumbed their noses at the
cavalier King Charles spaniel?
The researchers
also ignored prior studies showing the
importance of using breed-specific heart measurements for that breed --
thereby placing the CKCS at greater risk than other breeds when taking the
drug prematurely. This is just about the least informative study of the
safety and effectiveness of any drug with a prior record of toxicity, in
this century. Why would experienced veterinary cardiology researchers ignore
their own prior warnings of the vital importance of breed-specific heart
measurements and also fail to calculate the breed-specific data they
collected in this study? Why have the researchers thumbed their noses at the
cavalier King Charles spaniel?
• (13) The authors try to defend the manufacturer's total financial control over them. Interestingly, the authors bend over backwards to justify the full funding of this study by the manufacturer of pimobendan. They essentially explain that, 'that's the way it is in the veterinary field.' Specifically, they state:
"that the majority of published clinical trials are sponsored by industry. In the veterinary field, there are no large independent funding organizations comparable to the National Institutes of Health (NIH) that are likely to be able to (or wish to) fund a study of the magnitude of the one we describe; therefore, such studies are only likely to be achieved with industry sponsorship. Potential explanations of the increased likelihood of industry-sponsored research having positive findings include the following: Industrial sponsors might be more likely to support studies that are likely to succeed, industrial sponsors might design studies with an inappropriate comparator group, or there might be publication bias with unsuccessful studies being less likely to be published." (Emphasis added.)
There is a term used in the scientific research field for this type of defensive excuse making: "publication bias", and the authors even use it in the quote above. When they write, "... unsuccessful studies being less likely to be published", they could add, "unsuccessful results within studies" to the list of those being less likely to be published. And it is also apparent in the next topic discussed here: the glaring conflict between the March 2015 press releases and the actual findings in the September 28, 2016 journal article.
• (14) The report flatly contradicts the braggadocious press releases issued 18 months earlier. But the absolutely most irresponsible fact to be drawn from this report is the March 2015 press releases issued by the three lead researchers, which unqualifiedly stated:
"The interim analysis indicated that there was clear evidence of benefit of the administration of pimobendan in prolonging the time to the primary endpoint of the study, which was a composite of the development of left-sided congestive heart failure, or death presumed to be cardiac in origin. The interim analysis did not raise any concern over the safety of pimobendan administration." (Emphasis added.)
"A mid-study analysis in mid-February 2015 indicated that pimobendan is clearly beneficial and did not raise any concern over the administration of pimobendan." (Emphasis added.)
Nowhere in any of those self-laudatory press releases did any of the researchers warn of the vital importance of first performing two precise echocardiographic measurements and a radiographic measurement before dosing pimobendan to MVD-affected dogs prior to CHF.
Since the researchers knew in advance of those press releases what the essential parameters were for the dogs participating in the trial, they easily could have included those parameters in their press releases. But they did not. And so, for 18 months, from March 2015 to September 2016, every cardiologist and internal medicine specialist and general practice veterinarian was intentionally misled about the essential parameters which had to be met before prescribing pimobendan. This obviously indicates the danger of veterinary researchers ignoring their own professional judgment and instead signing their names to such irresponsible advertisements which must have been pushed upon them by the manufacturer with the checkbook.
It is jamming the square-pegged CKCS into the species-wide round hole!
 This study, unfortunately, has cut corners and added risks to cavaliers.
The researchers essentially are jamming nearly 50% of all of the dogs
in their study -- all of the CKCSs -- into a species-wide criteria which
they intentionally designed to ignore the thoroughly-researched and
well-established criteria for our breed, as if the cavaliers were a bunch of
square pegs to be hammered into round holes. They have minimized these very
important cavalier-specific parameters without any stated justification,
excuse, apology, or other explanation in their journal article.
This study, unfortunately, has cut corners and added risks to cavaliers.
The researchers essentially are jamming nearly 50% of all of the dogs
in their study -- all of the CKCSs -- into a species-wide criteria which
they intentionally designed to ignore the thoroughly-researched and
well-established criteria for our breed, as if the cavaliers were a bunch of
square pegs to be hammered into round holes. They have minimized these very
important cavalier-specific parameters without any stated justification,
excuse, apology, or other explanation in their journal article.
Anyone with a cavalier should proceed with caution because the study has not been designed to take into account the special needs of cavaliers. It appears that the EPIC Study has not been about avoiding the risking of the lives of MVD-affected dogs, especially cavaliers. False positives, ignored negatives, questionable research practices (QRPs) in general, and publication bias all point to a pre-determined goal: over-diagnosis so that one manufacturer may sell more of its product than ever before. It is a terribly unfortunate thing, but it is not a surprising thing. A lesson to be learned is that veterinary researchers need to learn to say "NO!" to full funding by drug manufacturers.
Always keep in mind Arthur C. Clarke's Third Law: Any sufficiently crappy research is indistinguishable from fraud.
RETURN TO TOP
September 30, 2016:
So your cavalier has a heart murmur. What do you do next?
UPDATED
since the EPIC Study!
The ACVIM says: Get an x-ray, not an ultrasound!
 Since over half of all cavalier King Charles spaniels may be expected to
develop mitral valve murmurs by age 5 years, it should come as no surprise
when your veterinarian tells you that your cavalier has one. But there is no
reason to panic. The American College of Veterinary Internal Medicine (ACVIM*)
has a sensible list of steps to take once a murmur is first detected in your
CKCS.
Since over half of all cavalier King Charles spaniels may be expected to
develop mitral valve murmurs by age 5 years, it should come as no surprise
when your veterinarian tells you that your cavalier has one. But there is no
reason to panic. The American College of Veterinary Internal Medicine (ACVIM*)
has a sensible list of steps to take once a murmur is first detected in your
CKCS.
For the record, the ACVIM recommends that cavaliers be screened annually by "auscultation" (examination by stethoscope) by board certified cardiologists. Specifically, ACVIM** states:
"Owners of breeding dogs or those at especially high risk, such as Cavalier King Charles Spaniels, may choose to participate in yearly screening events at dog shows or other events sponsored by their breed association or kennel club and conducted by board-certified cardiologists participating in an ACVIM-approved disease registry."
For that reason, CavalierHealth.org has a list of upcoming heart screening clinics in the USA and Canada, which is updated weekly.
Once a murmur is detected by the vet, the first thing to realize is that you do not need to rush your dog to have an ultrasound (echocardiograph) scan of its heart. Instead of an ultrasound, the ACVIM recommends that you get your dog's heart x-rayed to be a "baseline" for measuring the heart size against future x-rays after any heart enlargement takes place. The ACVIM states:
"Thoracic radiography [chest x-ray] is recommended in all patients to assess the hemodynamic significance of the murmur and also to obtain baseline thoracic radiographs at a time when the patient is asymptomatic for CVHD [chronic valvular heart disease]."
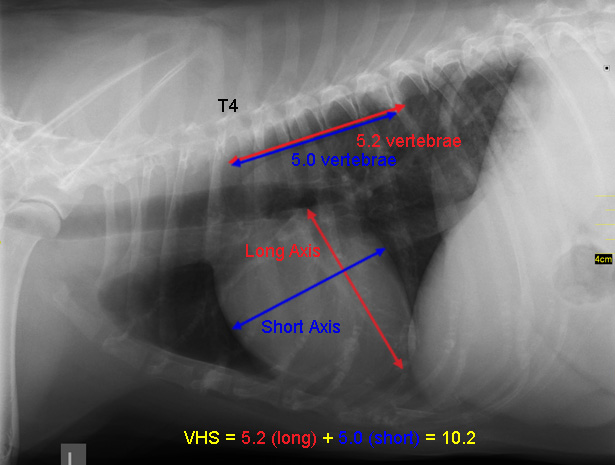 The ACVIM does not recommend that cavaliers with new murmurs be
ultrasounded unless the auscultation and the x-ray do not adequately satisfy
the cardiologist about the true cause of the murmur and the heart does not
appear to be significantly enlarged. Specifically, this is
what the ACVIM states about ultrasounding cavaliers once a mitral valve
murmur is detected:
The ACVIM does not recommend that cavaliers with new murmurs be
ultrasounded unless the auscultation and the x-ray do not adequately satisfy
the cardiologist about the true cause of the murmur and the heart does not
appear to be significantly enlarged. Specifically, this is
what the ACVIM states about ultrasounding cavaliers once a mitral valve
murmur is detected:
"In small breed dogs with typical murmurs, echocardiography is recommended to answer specific questions regarding either cardiac chamber enlargement or the cause of the murmur if those questions are not answered adequately by auscultation and thoracic radiography."
Note that the only "baseline" that the ACVIM recommends for cavaliers with new murmurs is an x-ray and not an ultrasound, as long as the cardiologist is satisfied that the stethoscopic exam and the x-ray confirm the cause of the murmur.
The EPIC Study's recommendations
In September 2016, a large team of board certified veterinary cardiologists issued a report, called the EPIC Study, revising how to diagnose and treat MVD-affected dogs once their hearts begin to enlarge significantly. Their conclusions do not change the above-described steps the cavalier's owner should take when a murmur is first detected, which is to get those baseline x-rays.
But the EPIC Study recommends that once an MVD-affected dog's heart murmur reaches Grade 3, if any x-rays -- the baseline or later ones -- show that the dog's heart has begun to enlarge (Stage B2 MVD), then the owner should have a cardiologist perform an ultrasound scan of the dog's heart -- an echocardiogram.
The EPIC Study's bottom line for starting pimobendan in Stage B2 is:
(1) The dog must be in Stage B2 of mitral valve disease; AND
(2) Have a murmur of at least Grade 3; AND
(3) The dog must NOT be on any other cardiac medication; AND
(4) An echocardiogram must be conducted and show valvular lesions of the mitral valve, regurgitation through the mitral valve (MR) on the color Doppler echocardiogram, and have echocardiographic evidence of left atrial and left ventricular dilatation (defined as a left atrial-to-aortic root ratio [LA/Ao] equal to or greater than 1.6 and body weight normalized left ventricular internal diameter in diastole [LVIDDN] equal to or greater than 1.7); AND
(5) X-rays showing evidence of enlargement with a vertebral heart score (VHS) greater than 10.5.
This essentially means that once the MVD-affected dog develops a Grade 3 murmur and an x-ray showing enlargement, the owner should have a board certified veterinary cardiologist perform the echo exam. However, published research has demonstrated that the EPIC Study's minimum measurements of enlargement really are within the range of normal sized hearts for cavaliers. Therefore, instead of relying upon the EPIC parameters, CKCSs' cardiologists should determine whether or not the Stage B dog really does have enlargement, rather than just a large normal size heart.
If and when the cardiologist determines from the x-ray and the measurements from the echocardiogram, that the dog's heart has enlarged enough, the EPIC Study's recommendation is that the cardiologist may prescribe treatment with pimobendan. Prior to publication of this EPIC Study, the consensus was to not treat MVD-affected cavaliers with any medications until the MVD progressed to heart failure.
* The ACVIM certifies
veterinary cardiologists. A list of them in the
USA and Canada is available here.
** See the ACVIM's
"Guidelines for the Diagnosis and Treatment of Canine Chronic Valvular Heart
Disease", page 1144.
RETURN TO TOP
August 18, 2016:
Is the University of Washington's
"Rapamycin Intervention Trial in
Pet Dogs" Unethical?
Thus far, all we have is publication of it's misleading
"findings"
and an obvious fund-raising campaign
 Owners
of cavalier King Charles spaniels are all excited about the prospects of
a miracle drug called "rapamycin" curing their dogs' mitral valve
disease (MVD). They are being duped.
Owners
of cavalier King Charles spaniels are all excited about the prospects of
a miracle drug called "rapamycin" curing their dogs' mitral valve
disease (MVD). They are being duped.
The University of Washington is conducting a series of studies of rapamycin*, boldly called the "Dog Aging Project", with the announced goal of determining if "rapamycin is effective at improving cardiac function in dogs at doses without significant side effects."
The researchers, mostly in the university's pathology department, have divided their study into two phases. "Trial One", concluded this month, was to "determine appropriate dosing of rapamycin and document cardiac improvements." Only 24 dogs participated in this 9-month study, all golden retrievers, Labrador retrievers, and German shepherd dogs over 40 lbs. Half of those - twelve in all - received rapamycin, and the other half received a placebo. Interestingly, they started with 40 dogs, but specifically excluded any found by echocardiogram to have even an asymptomatic heart valve disorder. The second phase, "Trial Two" is seeking participants via their study's dedicated website, which also includes a fund-raising campaign.
Our complaint is with the way they have publicized Trial One. Keep in mind these facts about it:
(1) Trial One ended this month (August 2016).
(2) The researchers immediately issued a press release announcing:
"As of August, 2016, we are finishing the analysis of the data for the dogs that completed the phase 1 study and hope to submit the results for publication within the next few months. The key findings are that there were no significant side effects associated with the rapamycin treatment, and there were statistically significant improvements in heart function in the dogs that received rapamycin relative to those that received the placebo, similar to what has been observed in older laboratory mice.
"... We view these initial results as highly encouraging, however, and feel that this phase 1 study provides a strong justification for the next phase of the intervention trial which will follow dogs for three to five years.**
So, not only has there been no peer-reviewing of this study, but the researchers admit that they have not even finished the analysis of the data. Nevertheless, they boldly make the assertion that the dogs receiving rapamycin had significant improvements in heart function!
Needless to say, the press has jumped on the bandwagon. For instance, the UK's Telegraph's headline on August 15 was "Trial to extend life of dogs shows 'significant improvements' in heart health, say scientists". The Telegraph's article goes on to state: "it could help dogs live for an extra four years."
So, whatever happened to following the ethical rules of scientific research? For instance, what has become of the need for full analysis of the data, followed by a carefully drafted article, which then is peer reviewed before a whisper is heard about the results of the study?
If you have any doubts about whether the August 2016 press release was unethical, consider that in the world of scientific research, it is highly unusual for raw research data, much less any results, to be leaked publicly before peer-reviewing and the official publication of the peer-reviewed article. Further, it used to be unheard of for there to be an official public release of any such premature information, issued by the researchers. Any such prior disclosure normally is considered unethical and unprofessional in the scientific research arena.
See, "What is Ethics in Research & Why is it Important?", by David B. Resnik, J.D., Ph.D. National Institute of Health website, 2011:
"There are many other activities that the government does not define as 'misconduct' but which are still regarded by most researchers as unethical. These are called 'other deviations' from acceptable research practices and include: ... Bypassing the peer review process and announcing your results through a press conference without giving peers adequate information to review your work."
Consider the fine print behind the University of Washington researchers' boasts. The study was limited to twelve large-breed dogs - none of which had a hint of MVD - taking rapamycin for nine months. Whether any of these dogs really did display any improvement in heart function remains to be seen. One thing we know is that their hearts already were functioning properly, because dogs with any sign of a heart problem were excluded.
We have seen another instance of this kind of research abuse recently. The glorified (and apparently exaggerated) results of the EPIC Trial, about which we have written several articles, were announced in this same seemingly unethical manner in three press releases (one each from the three lead researchers), within days of the EPIC trial's end in March 2015. The actual peer-reviewed article has yet to be published.
Let us hope that this tactic, of falsely whipping up the hopes of owners of MVD-affected cavaliers, comes to an end quickly, and is not just a beginning.
* Rapamycin is a bacteria-produced immunosuppressive agent used mainly to prevent the rejection of transplanted organs. It also is known as "sirolimus" and the brand name "Rapamune".
** The press release does contain this disclaimer, which nonetheless does not excuse the researchers from publishing anything at all at this stage: "It is important to keep in mind that this is a small study that requires replication before we can be confident in these results. It is also important to recognize that we don't have any evidence that the improvements in heart function indicate overall improvements in health or slower aging in these dogs or even what the long-term effects of rapamycin will be."
RETURN TO TOP
August 3, 2016:
Whither the EPIC Trial's final report?
Something about it smells terribly funny
 Last
February, we blogged that "EPIC trial
results are scheduled to be announced at the ACVIM Forum in Denver on
June 9", and we added, "15 months from the end of the trial to
publication of its results". The trial ended in March 2015 and was
promptly followed by tantalizing press releases claiming:
Last
February, we blogged that "EPIC trial
results are scheduled to be announced at the ACVIM Forum in Denver on
June 9", and we added, "15 months from the end of the trial to
publication of its results". The trial ended in March 2015 and was
promptly followed by tantalizing press releases claiming:
"The interim analysis indicated that there was clear evidence of benefit of the administration of pimobendan in prolonging the time to the primary endpoint of the study, which was a composite of the development of left-sided congestive heart failure, or death presumed to be cardiac in origin. The interim analysis did not raise any concern over the safety of pimobendan administration."
Apart from those extraordinarily inappropriate* March 2015 press releases, while it was true that a brief summary of the EPIC Trial findings was orally presented to a handful of veterinary cardiologists in June, very little of that information has leaked out, and the nitty-gritty data, findings, and conclusions remain under wraps. So that makes it 17 months now, since the end of the EPIC Trial, and still nothing published about it.
In the meantime, more and more veterinarians, seeing only those press releases, are prescribing pimobendan (Vetmedin, Cardisure, Safeheart 5, Fortekor Plus) willy-nilly to cavaliers with only the whispered hint of a mitral valve murmur, because they think that the EPIC Trial is all about starting doses of pimobendan as early as possible and with no exceptions. And, obviously, this is exactly what Vetmedin's manufacturer must want to happen.
We know from prior peer reviewed veterinary journal articles and cardiologists' observations that the premature use of pimobendan - prescribing it to dogs either not in heart failure or not needing augmentation of cardiac output - can accelerate the progression of MVD and irreversibly damage the dogs' hearts. And yet, know-it-all vets - including some cardiologists - are jumping the gun and prescribing this dangerous drug to our cavaliers which are not even close to heart failure.
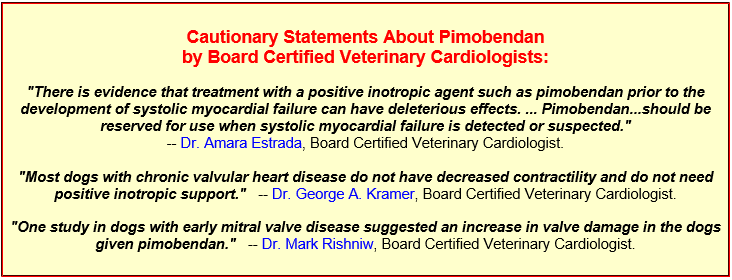
It is inexplicable as to why the EPIC Trial's final report has not yet been peer reviewed and published in a veterinary journal. The latest rumor is that the report will be published "this fall", probably in the Journal of Veterinary Internal Medicine. Whenever and wherever that may be, the premature prescribing of pimbendan has been rampant since those March 2015 press releases, and if the final report includes any exceptions to giving pimobendan to any cavalier with only a mild murmur and slight enlargement of the heart, somebody is going to have a lot of explaining to do. Something about this foot-dragging smells terribly funny, and appears to be all to the financial advantage to Vetmedin's manufacturer.
* See, "What is Ethics in Research & Why is it Important?", by David B. Resnik, J.D., Ph.D. National Institute of Health website, 2011: "There are many other activities that the government does not define as 'misconduct' but which are still regarded by most researchers as unethical. These are called 'other deviations' from acceptable research practices and include: ... Bypassing the peer review process and announcing your results through a press conference without giving peers adequate information to review your work."
RETURN TO TOP
April 15, 2016:
OFA finally recognizes what mitral valve disease is all about
Two steps forward and one step sideways for the still-provincial
Orthopedic Foundation for Animals
 The
Orthopedic Foundation for Animals (OFA) has been mired in the mid-20th
century since its inception in the 1960s. But, finally, at least in this month of April 2016, OFA has
recognized that mitral valve disease (MVD) is not "congenital"*.
For decades, OFA has maintained a database of heart defects titled
"Congenital Cardiac Database". Even though MVD is an "acquired"**
disorder and therefore not congenital, OFA fortunately has included
MVD test results in its Congenital Cardiac Database. We suppose that an
organization with "orthopedic" in its name may be excused for not quite
grasping the elementary aspects of the non-orthopedic but most widespread
herditary disease and killer among cavalier King Charles spaniels.
The
Orthopedic Foundation for Animals (OFA) has been mired in the mid-20th
century since its inception in the 1960s. But, finally, at least in this month of April 2016, OFA has
recognized that mitral valve disease (MVD) is not "congenital"*.
For decades, OFA has maintained a database of heart defects titled
"Congenital Cardiac Database". Even though MVD is an "acquired"**
disorder and therefore not congenital, OFA fortunately has included
MVD test results in its Congenital Cardiac Database. We suppose that an
organization with "orthopedic" in its name may be excused for not quite
grasping the elementary aspects of the non-orthopedic but most widespread
herditary disease and killer among cavalier King Charles spaniels.
* Congenital means
that the disease or physical abnormality existed in utero or at birth.
** Acquired means that the disease began
developing after birth.
Effective this month, OFA has attempted to right this wrong, although it still shows that it does not fully understand exactly what MVD is all about. As of April 1, OFA has joined with the American College of Veterinary Internal Medicine (ACVIM) to create a new "Advanced Cardiac Database" to distinguish between congenital and what OFA has labeled "adult-onset" cardiac diseases. It will serve two primary purposes:
"1. Develop an appropriate screening protocol for adult onset cardiac diseases; and
2. Begin collecting better data on cardiac disease prevalence and progression in the purebred dog."

According to OFA, the examinations for the Advanced Cardiac Database must be performed by board certified veterinary cardiologists. This is a huge step forward for OFA. Previously, practitioner veterinarians have been allowed to perform these tests for OFA's database purposes.
The cardiologist will send the exam results to OFA and the ACVIM
The most significant change will be the reporting procedure to OFA. Previously, the only copy of the veterinarian's exam report was given to the dog's owner, to either submit to OFA for its database or to not do so. Hereafter, the new OFA advanced cardiac examination forms will be in triplicate. As in the past, one copy of the completed exam form will be given to the dog's owner. (See a copy of the new form, below.) However, regardless of whether or not the owner sends his copy of the form to OFA for official certification, the examining cardiologist will retain one copy of the form and submit it to OFA and the ACVIM, to be used only to record results on its database, in order to collect better heart disease prevalence and progression data by breed. If the cardiologist also performs an echocardiogram, the new form's echo section is far more detailed, to collect statistics regarding flow rates, velocities, etc.
The dog owner's responsibility for obtaining an official OFA clearance certification number remains the same as in the past. Owners must submit their copy of the completed, signed form to OFA along with the filing fee. OFA clearances under the Advanced Cardiac Database will be valid for only 12 months. If the owner wants the adult onset cardiac clearance to remain current, repeat exams will be necessary.
OFA still does not grasp how and when MVD develops in cavaliers
While this step obviously is progress, since previously OFA did not officially recognize the existence of non-congenital heart disorders, OFA still does not appear to fully grasp how MVD develops, particularly in cavalier King Charles spaniels. OFA seems to think that there are only two categories of cardiac diseases in dogs - the congenital type and the "adult-onset" type. In fact, MVD is not necessarily an adult-onset disorder, since statistics have shown that as many as 10% of cavaliers have developed MVD murmurs before their first birthday. Incidentally, OFA's minimum age for dogs undergoing these cardiac examinations is 12 months, which is not quite the age of adulthood for CKCSs.
For more information, see OFA's press release here. The new Advanced Cardiac Database form is below. A pdf version is downloadable here.
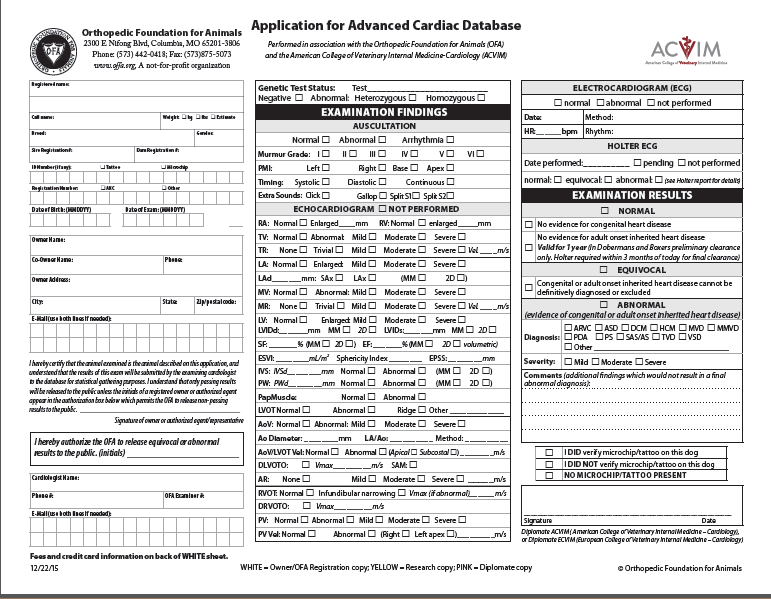
RETURN TO TOP
April 14, 2016:
A Giant Leap Backwards:
Some USA cavalier breeders boycott posting
health test clearances on
the OFA website
They must want to keep other breeders and pet buyers in the dark
 The
Orthopedic Foundation for Animals (OFA) was founded in 1966 in the USA to "promote the
health and welfare of companion animals through a reduction in the incidence
of genetic disease." Its main objectives include:
The
Orthopedic Foundation for Animals (OFA) was founded in 1966 in the USA to "promote the
health and welfare of companion animals through a reduction in the incidence
of genetic disease." Its main objectives include:
• To collate and disseminate information concerning orthopedic and genetic diseases of animals.
• To advise, encourage and establish control programs to lower the incidence of orthopedic and genetic diseases.
OFA's primary means of carrying out its objectives is its on-line database of health testing clearances of breeding stock. As OFA explains it:
"The OFA databases are core to the organization's objective of establishing control programs to lower the incidence of inherited disease. Responsible breeders have an inherent responsibility to breed healthy dogs. The OFA databases serve all breeds of dogs and cats, and provide breeders a means to respond to the challenge of improving the genetic health of their breed through better breeding practices. The testing methodology and the criteria for evaluating the test results for each database were independently established by veterinary scientists from their respective specialty areas, and the standards used are generally accepted throughout the world."
Responsible cavalier breeders post all health clearances on OFA's website
Responsible breeders have their breeding stock tested by veterinary specialists according to OFA's protocols, for such genetic disorders as hips, elbows, heart, eyes, and patellas. If a dog passes a test, OFA issues a certification number to the dog for that test and posts the test result in its databases on its website. That is, if the dog's owner allows OFA to post the health clearance result. Responsible breeders, of course, authorize the posting of those clearances for their dogs. Irresponsible breeders do not.
Recently, more and more breeders of cavalier King Charles spaniels are announcing their intention to not allow OFA to post the health clearances of their breeding stock. (See one of their posters below.) They claim that a few disgruntled pet buyers are using missing health-testing information about dogs on OFA's website to accuse the breeders of either not testing their breeding stock or not following breeding protocols based upon the results of those health tests.
Cavalier breeders' excuses for boycotting OFA are spurious
 These
cavalier breeders' excuses for boycotting OFA are spurious. These
breeders fall into three categories:
These
cavalier breeders' excuses for boycotting OFA are spurious. These
breeders fall into three categories:
1. Previously, some of these breeders have allowed OFA to post on its public databases some of their dogs' health testing clearances, but not all of them.
2. Others of these breeders have never allowed OFA to post any of their dogs' health testing clearances.
3. And, in some instances, unfortunately, some cavalier breeders do not bother to health test their breeding stock, at all.
But regardless of which category they fall within, their argument for now not allowing OFA to publicly post any health clearances, is that disgruntled pet owners are using their dogs' publicly posted clearances on the OFA website to accuse them of not testing their dogs before breeding them. The illogic of that excuse is stunning. Clearly, if all of these breeders' dogs' health-testing clearances are posted on OFA's website, the complainers would have nothing to accuse the breeders of not doing.
The fact is, as we have witnessed so many times over the past decades, some cavalier breeders care only about their own breeding program and not one whit about the health and welfare of future generations of cavalier King Charles spaniels here in the USA.
They claim that whether and when their dogs have passed health tests is nobody's business but their own. They claim that they will provide their puppy buyers with copies of the health test clearances, but no one else should be allowed to see those papers. These breeders are selfish and short-sighted, because they fail to recognize the importance of making available their dogs' health test results for future generations of breeding stock to be bred by other breeders, even decades from now.
So, the bottom line clearly is that any cavalier breeder in the USA who refuses to allow OFA to publicly post all of their dogs' health test clearances, by definition, is an irresponsible breeder.
RETURN TO TOP
February 2, 2016:
EPIC trial results are scheduled to be announced
at the ACVIM Forum
in Denver on June 9
15 months from the end of the trial to publication of its results
Why wait so long?
The results of the EPIC* Trial, a five-year
study of up to 360 dogs suffering from pre-heart-failure MVD, will
 be
announced at ACVIM's annual forum in Denver, Colorado on June 9, 2016. All
three lead researchers, Drs. Adrian Boswood, Sonya Gordon, and Jens
Haggstrom, are scheduled to participate in the "EPIC Trial Results" session
that morning.
be
announced at ACVIM's annual forum in Denver, Colorado on June 9, 2016. All
three lead researchers, Drs. Adrian Boswood, Sonya Gordon, and Jens
Haggstrom, are scheduled to participate in the "EPIC Trial Results" session
that morning.
The EPIC Trial, fully funded by Boehringer Ingelheim, the manufacturer of pimobendan (Vetmedin), began in 2010 as a placebo-controlled clinical trial evaluating the effectiveness of pimobendan in the prevention of the onset of signs of congestive heart failure in dogs with cardiac enlargement secondary to pre-clinical MVD. Thirty-six veterinary cardiologists from all over the globe participated, each examining ten MVD-affected dogs over the following five years, ending March 1, 2015.
The boastful March 2015 announcements were unethical and premature
 Since
publication of
three clearly unethical**, premature public
announcements*** in March 2015 of
non-peer-reviewed "interim analysis", claiming "clear evidence
of benefit of the administration of pimobendan in prolonging the time to the
primary endpoint of the study", a
Since
publication of
three clearly unethical**, premature public
announcements*** in March 2015 of
non-peer-reviewed "interim analysis", claiming "clear evidence
of benefit of the administration of pimobendan in prolonging the time to the
primary endpoint of the study", a
 lid has been firmly placed upon
the actual results of the study.**** See, for
example, Dr. Gordon's clearly inappropriate statement which she made in her
March 2015 press release, at left.
lid has been firmly placed upon
the actual results of the study.**** See, for
example, Dr. Gordon's clearly inappropriate statement which she made in her
March 2015 press release, at left.
It will have been an extraordinary length of time -- over fifteen months to be exact -- between the March 1, 2015 end date of the study and the June 9, 2016 release of the actual (and presumably) peer-reviewed results. The scheduled date of the release reportedly has been postponed twice, without explanation.
The March 2015 press releases had manufacturer Boehringer Ingelheim's desired effect, because numerous veterinarians -- specialists and general practice vets alike -- have been ignoring the FDA guidelines which forbid the administration of pimobendan to MVD-affected dogs prior to heart failure. When questioned about the lack of any evidentiary support for violating the FDA ruling, many such veterinarians have referenced the March 2015 announcements as their sole justification. Thus, if the full report includes any conditions or qualifications to the press releases' bold asssertion of "clear evidence of benefit", then the lead researchers will have a lot of explaining to do.
Ironically, in a March 2016 veterinary journal article, a team of Japanese researchers succintly summarized the current peer-reviewed studies finding that pimobenan can cause adverse effects, including the acceleration of mitral valve degeneration, in dogs. They stated:
"Pimobendan (PIMO) can cause adverse effects, such as mitral valve degeneration, in dogs. ... Despite the benefits of treatment, adverse effects have been reported with the use of PIMO in dogs. In a case report of two dogs with mitral insufficiency, a long-term administration of PIMO worsened mitral regurgitation and ventricular hypertrophy. Similarly, in dogs with mild mitral insufficiency, the long-term administration of PIMO was shown to worsen mitral regurgitation and valve lesions. Adverse effects on mitral valves were considered to occur because of increasing cardiac contraction, but it was unclear whether PIMO directly affected the mitral valves."
Why wait so long to publish?
A burning question remains: Why have the lead researchers waited over 15 months to disclose the peer-reviewed results of the EPIC Trial?
Obviously, in the interim, manufacturer Boehringer Ingelheim has been getting exactly what it has been paying for.
* "Evaluation of Pimobendan In dogs with Cardiomegaly caused by preclinical mitral valve disease".
** See, "What is Ethics in Research & Why is it Important?", by David B. Resnik, J.D., Ph.D. National Institute of Health website, 2011: "There are many other activities that the government does not define as 'misconduct' but which are still regarded by most researchers as unethical. These are called 'other deviations' from acceptable research practices and include: ... Bypassing the peer review process and announcing your results through a press conference without giving peers adequate information to review your work."
*** See the releases here: 1, 2, and 3.
**** Dr. Boswood's March 7, 2015 press release was supplemented a month later with this addition in bold font: "Please note - quantitative analysis of these results will not be discussed until the full results are available."
RETURN TO TOP
October 25, 2015:
Feed the fat cavalier less and exercise it more!
 Unfortunately,
but perhaps not surprisingly, cavalier King Charles spaniels are
pre-disposed to obesity. In other words, for whatever reason, it is easier
for cavaliers to gain excess weight than nearly any other breed. Their
pleading eyes and sweet demeanor are nearly impossible for many owners to
resist. The CKCS's only serious competition in this area are Labrador
retrievers, boxers, Cairn and Scottish terriers, and Cocker spaniels.
Unfortunately,
but perhaps not surprisingly, cavalier King Charles spaniels are
pre-disposed to obesity. In other words, for whatever reason, it is easier
for cavaliers to gain excess weight than nearly any other breed. Their
pleading eyes and sweet demeanor are nearly impossible for many owners to
resist. The CKCS's only serious competition in this area are Labrador
retrievers, boxers, Cairn and Scottish terriers, and Cocker spaniels.
Obesity in dogs is considered to be a medical disorder and is the canines' most common nutritional disease. Its estimated prevalence, species-wide, ranges from 30% to 50%, with the percentage of fat cavaliers probably even higher. Obesity is defined as "an accumulation of excessive amounts of adipose tissue in the body. " While some other health disorders may cause cavaliers to gain too much weight, scientifically speaking, it usually is the result of either eating too much and/or not exercising enough. Veterinary specialists call this "overnutrition".
 Obesity is unhealthful because it can lead to other disorders and
accelerate the effects of still more of them. For instance and most
importantly, it can shorten
their life spans. It can have severe effects upon the dogs' respiratory system
function, especially as an added risk factor for
breathing difficulties due to
brachycephalic airway
obstruction syndrome (BAOS), another disorder to which cavaliers are
pre-disposed due to their shortened muzzle lengths. It can affect cardiac
function, cardiac rhythm, and left ventricular volume, all of particular
concern to the CKCS because of the breed's prevalence of
mitral valve disease (MVD). It can be
a major risk factor for hip dysplasia and
intervertebral disc
disease, two other disorders more common in cavaliers than the average
purebred.
Obesity is unhealthful because it can lead to other disorders and
accelerate the effects of still more of them. For instance and most
importantly, it can shorten
their life spans. It can have severe effects upon the dogs' respiratory system
function, especially as an added risk factor for
breathing difficulties due to
brachycephalic airway
obstruction syndrome (BAOS), another disorder to which cavaliers are
pre-disposed due to their shortened muzzle lengths. It can affect cardiac
function, cardiac rhythm, and left ventricular volume, all of particular
concern to the CKCS because of the breed's prevalence of
mitral valve disease (MVD). It can be
a major risk factor for hip dysplasia and
intervertebral disc
disease, two other disorders more common in cavaliers than the average
purebred.
 What to do? Feed the fat cavalier less and exercise it
more! It usually is as simple as that. It may not be easy, because maybe you
already have conditioned your dogs and yourself to feeding them upon their
demand. But the remedy is simple. Don't feed as much per meal. Eliminate
junky treats; if you must treat, do so infrequently and only as a reward for good behaviors,
and use healthful, nutritious dog food as that reward. And, most
importantly, walk your fat dogs - every day. If you already walk them, then
take them on longer walks.
What to do? Feed the fat cavalier less and exercise it
more! It usually is as simple as that. It may not be easy, because maybe you
already have conditioned your dogs and yourself to feeding them upon their
demand. But the remedy is simple. Don't feed as much per meal. Eliminate
junky treats; if you must treat, do so infrequently and only as a reward for good behaviors,
and use healthful, nutritious dog food as that reward. And, most
importantly, walk your fat dogs - every day. If you already walk them, then
take them on longer walks.
What should be your goal - an ideal weight? The weight is not as important as the shape of the body. Veterinarians have devised a couple of charts called "Body Condition Scoring" or "Body Condition System", showing either five or nine different shapes of the canine body, from extremely fat to far too thin. The goal is to reach the middle number of, essentially, an hour-glass figure. See the two charts below:
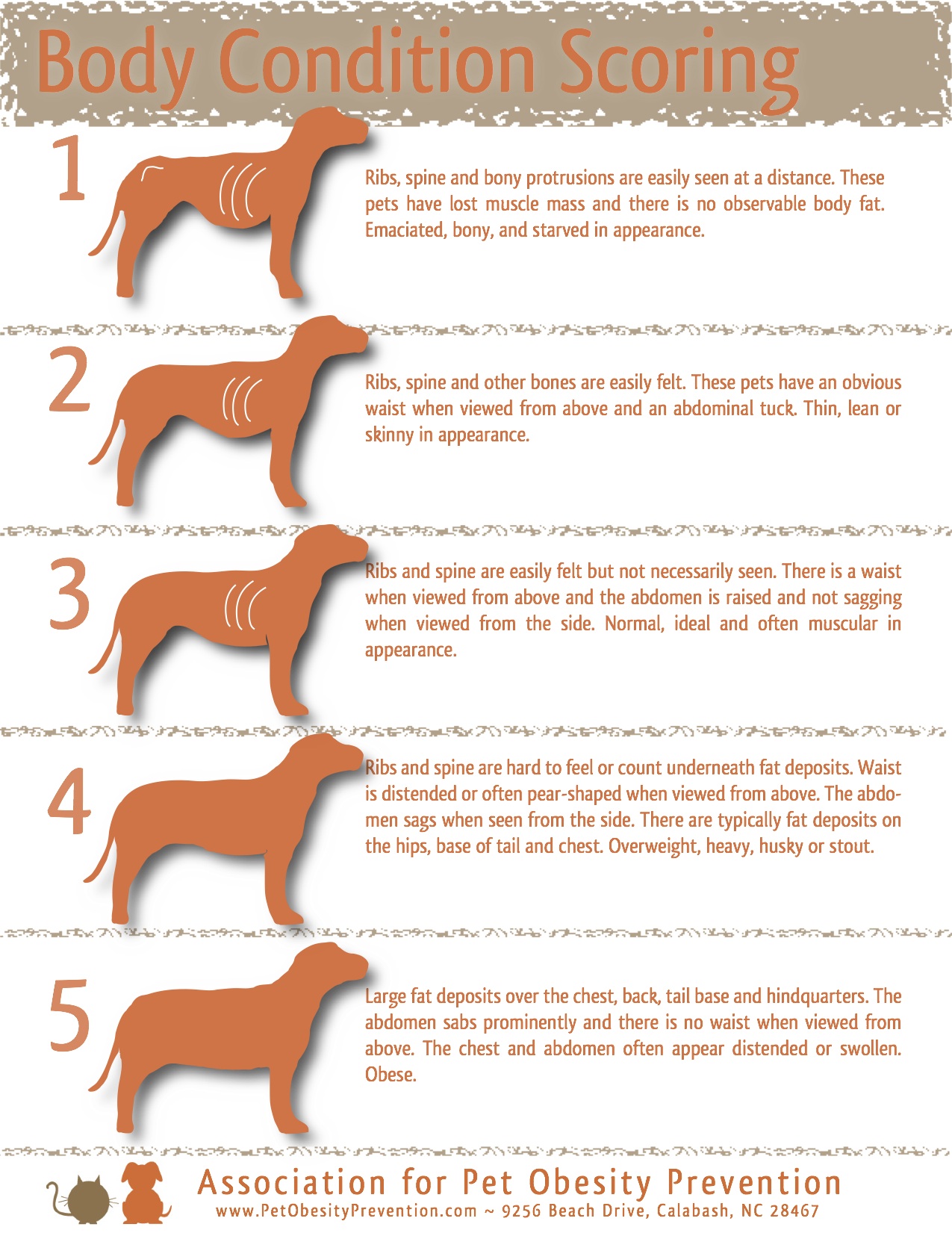
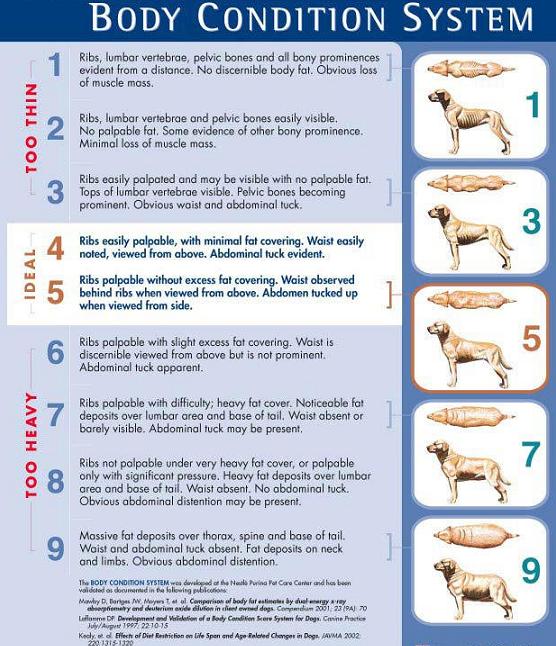
RETURN TO TOP
October 14, 2015:
Cardiologists focus on bionic fixes
to the leaking mitral valve
Four man-made devices are in the works
 Since
the first realization that some purebred dogs, particularly cavalier King
Charles spaniels, regularly develop mitral valve disease, veterinary
cardiologists have dealt with MVD-caused congestive heart failure by trying
to "manage" its consequences with drugs. They started with digoxin, a
relative of the 18th century herbal digitalis from the foxglove plant. Then
they added diuretics (and ACE-inhibitors, to offset the negative side
effects of the diuretics). And now we have pimobendan, which its
manufacturer anxiously is trying to get approved for use as a preventative
of heart failure in dogs.
Since
the first realization that some purebred dogs, particularly cavalier King
Charles spaniels, regularly develop mitral valve disease, veterinary
cardiologists have dealt with MVD-caused congestive heart failure by trying
to "manage" its consequences with drugs. They started with digoxin, a
relative of the 18th century herbal digitalis from the foxglove plant. Then
they added diuretics (and ACE-inhibitors, to offset the negative side
effects of the diuretics). And now we have pimobendan, which its
manufacturer anxiously is trying to get approved for use as a preventative
of heart failure in dogs.
In the past decade, veterinary surgeons, particularly in Japan and the USA, have tried their hand at replacing defective mitral valves with transplants from pigs, or even mechanical valves. But serious drawbacks to such surgeries include the need to by-pass the heart's pumping system during the procedures and the requirement that the patient be young and otherwise healthy enough to endure the operation and recovery without dying from stress or transplant rejection. And, it has gone without saying that the costs of such procedures, from thirty thousand dollars and up, is prohibitive to all but the wealthiest of cavalier owners.
So now, some inventive cardiologists are focusing upon simplified surgeries which would not require by-passing the heart during the brief procedure and are designed to prevent the deteriorating mitral valve from allowing blood to backflow through it.
All four of these quick-fixes involve inserting man-made devices onto or
into the heart while it continues to
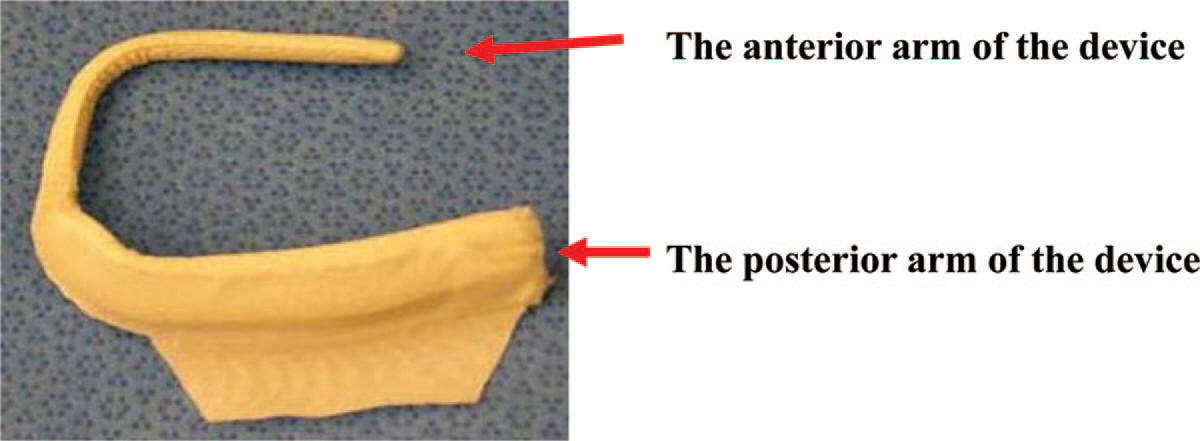 beat
normally. The first of these, with the full name of "epicardial mitral
annuloplasty device" but nicknamed "Mitrex", is essentially a U-shaped clamp
(right) which is wrapped around the mitral valve leaflets and
tightens them so that they are prevented from allowing blood to backflow
through the valve. The Mitrex clamp reportedly has been inserted on dogs'
beating hearts in less than 30 seconds. The device currently is being tested
by veterinary cardiac surgeons at clinics in California and Florida on
MVD-affected dogs in congestive heart failure.
beat
normally. The first of these, with the full name of "epicardial mitral
annuloplasty device" but nicknamed "Mitrex", is essentially a U-shaped clamp
(right) which is wrapped around the mitral valve leaflets and
tightens them so that they are prevented from allowing blood to backflow
through the valve. The Mitrex clamp reportedly has been inserted on dogs'
beating hearts in less than 30 seconds. The device currently is being tested
by veterinary cardiac surgeons at clinics in California and Florida on
MVD-affected dogs in congestive heart failure.
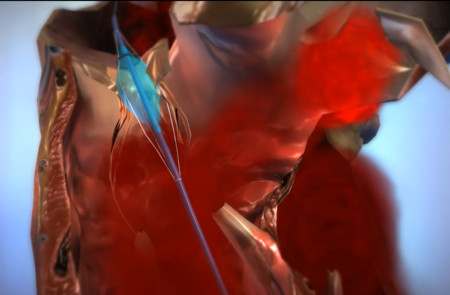 Veterinary
cardiologist Dr. George Kramer, is researching the viability of a balloon
device, called the Tucker valve (left), which is inserted through
either the mitral or the tricuspid valve in order to block regurgitation of
blood through the valve back into the atrium.
Veterinary
cardiologist Dr. George Kramer, is researching the viability of a balloon
device, called the Tucker valve (left), which is inserted through
either the mitral or the tricuspid valve in order to block regurgitation of
blood through the valve back into the atrium.
Veterinary cardiologist Simon Swift has begun research on a valvular prosthesis that is to be implanted but does not require the use of cardiopulmonary by-pass during the installation procedure. While he has not yet publicly published details of the device, he proposes to reduce the cost of the prosthesis by manufacturing his own valves.
 In
June 2013, a team of California medical cardiologists reported that they had
found that injecting alginate hydrogel directly into the left ventricle (LV)
of the hearts of 7 dogs in advanced heart failure, increased the thickness
of the LV wall, and LV structure and function improved. Alginate is a
naturally derived polysaccharide that is used in drug delivery and as cell
encapsulation material. (See a diagram of the injection at right.)
In
June 2013, a team of California medical cardiologists reported that they had
found that injecting alginate hydrogel directly into the left ventricle (LV)
of the hearts of 7 dogs in advanced heart failure, increased the thickness
of the LV wall, and LV structure and function improved. Alginate is a
naturally derived polysaccharide that is used in drug delivery and as cell
encapsulation material. (See a diagram of the injection at right.)
For more information about these devices, see our section on them on our MVD webpage.
RETURN TO TOP
July 1, 2015:
Heart failure in the MVD-affected
cavalier King Charles spaniel
What it is, and what it is not
 The terms "heart failure" and "congestive heart failure" are used almost
interchangeably by many veterinary cardiologists when discussing mitral
valve disease (MVD) in the cavalier King Charles spaniel. Nevertheless,
there can be a difference between the two.
The terms "heart failure" and "congestive heart failure" are used almost
interchangeably by many veterinary cardiologists when discussing mitral
valve disease (MVD) in the cavalier King Charles spaniel. Nevertheless,
there can be a difference between the two.
What is "heart failure"?
In the ACVIM's 2009 "Guidelines for the Diagnosis and Treatment of Canine Chronic Valvular Heart Disease" (ACVIM Consensus Statement), it claims to be providing a definition of "heart failure", but it really does not. The ACVIM introduces its "new system" of "4 basic stages of heart disease and failure", and yet the ACVIM uses the term "heart failure" in them without defining it. Nevertheless, the ACVIM's Consensus Statement gives us hints as to what that definition might be.
First, by way of introduction to the topic, it states:
"Heart failure is a general term that describes a clinical syndrome that can be caused by a variety of specific heart diseases, including CVHD [chronic valvular heart disease]. Heart failure from any cause is characterized by cardiac, hemodynamic, renal, neurohormonal, and cytokine abnormalities."
So from that, we learn that heart failure is a "clinical syndrome", characterized by "abnormalities".
 The Consensus Statement goes on to cite the 2001 American College of
Cardiology Foundation/American Heart Association [ACCF/AHA] classification system for
the treatment of heart disease and failure in human patients*, stating the
ACVIM has adapted that human classification system to the management of
canine MVD. Fortunately, the
ACCF/AHA does provide a useable and
understandable definition of heart failure. It states:
The Consensus Statement goes on to cite the 2001 American College of
Cardiology Foundation/American Heart Association [ACCF/AHA] classification system for
the treatment of heart disease and failure in human patients*, stating the
ACVIM has adapted that human classification system to the management of
canine MVD. Fortunately, the
ACCF/AHA does provide a useable and
understandable definition of heart failure. It states:
"HF [heart failure] is a complex clinical syndrome that results from any structural or functional impairment of ventricular filling or ejection of blood. The cardinal manifestations of HF are dyspnea [difficult or labored breathing] and fatigue, which may limit exercise tolerance, and fluid retention, which may lead to pulmonary and/or splanchnic congestion and/or peripheral edema. Some patients have exercise intolerance but little evidence of fluid retention, whereas others complain primarily of edema, dyspnea, or fatigue. Because some patients present without signs or symptoms of volume overload, the term 'heart failure' is preferred over 'congestive heart failure.' There is no single diagnostic test for HF because it is largely a clinical diagnosis based on a careful history and physical examination."
The "bottom line" as to what is and is not heart failure -- particularly congestive heart failure -- seems to be that it is a combination of the heart not pumping sufficient quantities of blood to the body plus outward signs or symptoms of the consequences of the body not receiving those sufficient quantities. The examining veterinarian must both determine if the heart is pumping adequately and look for those outward signs. So essentially, within reasonable limits, a veterinary cardiologist can "call it as he sees it" in terms of diagnosing heart failure in an MVD-affected cavalier.
 To get back to the ACVIM Consensus Statement, even though it fails to
adequately define "heart failure", it is crystal clear that only dogs in
either Stage C or Stage D are in heart failure, and that dogs in Stages A or
B1 or B2 are not. Therefore, a dog with a loud murmur and an enlarged heart
is not in heart failure unless it also displays some specific clinical
symptoms and signs, such as coughing, dyspnea/orthopnea (difficulty
breathing / shortness of breath while lying down), anorexia / cachexia (lack of
appetite/involuntary weight loss), edema / ascites (fluid collecting in
cavities and tissues), restlessness especially at night; tire easily,
reluctance to exercise, less playful, lethargic, depressed,
collapse / syncopal (fainting or nearly fainting). It is for this reason that
counting respiratory rates is so important in being able to identify the
onset of heart failure.
To get back to the ACVIM Consensus Statement, even though it fails to
adequately define "heart failure", it is crystal clear that only dogs in
either Stage C or Stage D are in heart failure, and that dogs in Stages A or
B1 or B2 are not. Therefore, a dog with a loud murmur and an enlarged heart
is not in heart failure unless it also displays some specific clinical
symptoms and signs, such as coughing, dyspnea/orthopnea (difficulty
breathing / shortness of breath while lying down), anorexia / cachexia (lack of
appetite/involuntary weight loss), edema / ascites (fluid collecting in
cavities and tissues), restlessness especially at night; tire easily,
reluctance to exercise, less playful, lethargic, depressed,
collapse / syncopal (fainting or nearly fainting). It is for this reason that
counting respiratory rates is so important in being able to identify the
onset of heart failure.
Is "congestive heart failure" different from "heart failure"?
Yes, it can be, in the context of MVD. The term "congestive" often mistakenly is assumed to refer to fluid from the heart, which collects in the lungs. However, medically speaking, "congestive" simply means that the heart is unable to pump adequate blood to the body, and as a result, the blood that is not being pumped out of the heart is being retained within the heart. Some of that fluid may also back up into the lungs, and so fluid detected in the lungs can be a sign of congestive heart failure.
What are "systolic dysfunction" and the "ejection fraction"?
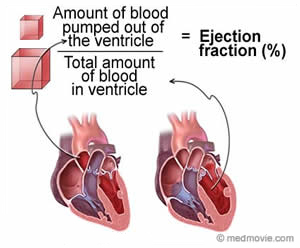 "Systolic dysfunction" occurs when the heart muscle does not contract
with enough force to pump enough oxygen-rich blood throughout the body. It
also is referred to as "diminished contractility". During an echocardiogram,
the cardiologist is able to calculate the "ejection fraction", which
measures how well the heart pumps with each beat. That ejection fraction
determines whether there is systolic dysfunction.
"Systolic dysfunction" occurs when the heart muscle does not contract
with enough force to pump enough oxygen-rich blood throughout the body. It
also is referred to as "diminished contractility". During an echocardiogram,
the cardiologist is able to calculate the "ejection fraction", which
measures how well the heart pumps with each beat. That ejection fraction
determines whether there is systolic dysfunction.
For many years, heart failure has been considered by many veterinarians to be synonymous with a systolic dysfunction, despite research evidence to the contrary.** Cardiologists have discovered that some MVD-affected dogs - particularly among toy breeds and especially many CKCSs - display classic signs and symptoms of heart failure without having a low ejection fraction or systolic dysfunction or diminished contractility. Dogs in heart failure but which nevertheless have an ejection fraction greater than about 50% are considered to be adequately "compensating" for their MVD condition or have a "preserved ejection fraction".
This distinction is particularly important when deciding when to begin medicating the MVD-affected dog in heart failure. Some standard MVD drugs for dogs in heart failure are designed to compensate for systolic dysfunction and to increase the ejection fraction. In particular, pimobendan (Vetmedin, Cardisure) is one of those drugs. But if the cavalier in heart failure is adequately compensating for its condition with a normal ejection fraction and therefore no systolic dysfunction, those drugs could over-stimulate the heart muscle and cause damage, rather than manage the dog's heart failure.
______
* ACC/AHA
Guidelines for the Evaluation and Management of Chronic Heart Failure in the
Adult: Executive Summary. A Report of the American College of
Cardiology/American Heart Association Task Force on Practice Guidelines. J.
American College of Cardiology. July 2001;38(7):2101-2113.
**
Myocardial function in small dogs with chronic mitral regurgitation and severe congestive heart failure. Kittleson MD, Eyster GE, Knowlen GG, Bari Olivier N, Anderson LK. JAVMA. February 1984;184(4):455-459.
("This study suggests that the contractile performance of the left ventricle
in most dogs with chronic mitral valve fibrosis and clinical evidence of
severe congestive heart failure is either normal or mildly depressed. This
suggests that congestive heart failure in these patients is due to severe
regurgitation and subsequent volume overload of the left ventricle and
atrium. Heart failure secondary to mitral regurgitation can be due not only
to myocardial failure, but also to severe regurgitation by itself or in
combination with myocardial failure.").
RETURN TO TOP
April 30, 2015:
The CKCSC,USA makes part of its ethics code optional!
It's real motto: "Forever Guardians of the Cavalier BREEDERS!"
 The
Cavalier King Charles Spaniel Club, USA (CKCSC,USA), like all other
nationwide cavalier clubs, has a
Code of Ethics. Traditionally, ethics
codes, like the Ten Commandments, command breeders either to always do
something or to never do something. For instances, the CKCSC,USA's code has
stated:
The
Cavalier King Charles Spaniel Club, USA (CKCSC,USA), like all other
nationwide cavalier clubs, has a
Code of Ethics. Traditionally, ethics
codes, like the Ten Commandments, command breeders either to always do
something or to never do something. For instances, the CKCSC,USA's code has
stated:
"If I decide to breed a litter, I will ..."
"As the owner of a stud dog, I realize that I must exercise exemplary conduct in the use of my dog in order to abide by the standards set forth in this Code of Ethics. Therefore I will ..."
"As the owner of a brood bitch, I realize that I must exercise exemplary conduct in breeding from her in order to abide by the standards set forth in this Code of Ethics. Therefore I will not: ..."
But no longer. As of March 14, 2015, the CKCSC,USA has made portions of its ethics code optional! Specifically, it has added this non-mandatory (and therefore meaningless) statement to the ethics code section on breeding brood bitches*:
"The CKCSC,USA recommends a minimum breeding age of 2½ years, and following the health testing guidelines as published on the CKCSC,USA website."
It is bad enough that the club's so-called "health testing guidelines" do not even include the MVD breeding protocol, but to make health testing optional in its ethics code shows that, in reality, the CKCSC,USA is Forever Guardian of the Cavalier BREEDERS!
* Not even this recommendation applies to stud dogs!
RETURN TO TOP
April 19, 2015:
"Purebred breeding" is a euphemism
for accelerated genetic entrophy
Toss out that closed studbook now!
 Researchers estimate that more than 50% of cavalier King Charles spaniels
(CKCSs) may have the genetic neurological disorder called syringomyelia
(SM), also known as "neck scratcher's disease". And, they estimate that up
to 95% of CKCSs may have Chiari-like malformation (CM), which purportedly is
at least part of the cause of SM. And, we know from statistics that more
than half of all cavaliers may be expected to develop mitral valve disease
by their fifth birthday. So what are we doing wrong? And what do these
severe genetic problems - among several others*
-- foretell about the future of our breed?
Researchers estimate that more than 50% of cavalier King Charles spaniels
(CKCSs) may have the genetic neurological disorder called syringomyelia
(SM), also known as "neck scratcher's disease". And, they estimate that up
to 95% of CKCSs may have Chiari-like malformation (CM), which purportedly is
at least part of the cause of SM. And, we know from statistics that more
than half of all cavaliers may be expected to develop mitral valve disease
by their fifth birthday. So what are we doing wrong? And what do these
severe genetic problems - among several others*
-- foretell about the future of our breed?
* To name the rest: various hereditary eye disorders, progressive hereditary deafness, low blood platelets (idiopathic asymptomatic thrombocytopenia), cerebellar infarcts (strokes), chronic pancreatitis, brachycephalic airway obstruction syndrome (BAOS), curly coat syndrome, intervertebral disk disease (IVDD), diabetes mellitus, eosinophilic stomatitis, idiopathic epilepsy, episodic falling syndrome, fly catchers syndrome, primary secretory otitis media (PSOM) - glue ear, chronic kidney disesase, masticatory muscle myositis (MMM), muscular dystrophy, obesity, patellar luxation, hip dysplasia (HD), and pneumocystis pneumonia.
 For starters, it means that the breed clubs' proverbial "closed studbook*"
is destined to fail, and bring the entire breed down with it.
For starters, it means that the breed clubs' proverbial "closed studbook*"
is destined to fail, and bring the entire breed down with it.
* In the parlance of dog breeding, the "studbook" is the list of pedigrees of the dogs of a particular breed. In turn, "pedigree" means the record of the ancestors of a breed, showing that it is "purebred". "Purebred" means that all of the dogs in the breed descended from other dogs of the same breed. Therefore, no dogs of any other breed (or multi-breed) are allowed entry into a breed club's closed studbook. If a mating occurs between a purebred dog and a dog of some other breed, their offspring are ostracized by that breed club, banned from participating in purebred activities, especially conformation shows, much less being allowed to mate with any other dogs of that breed.
The second law of thermodynamics applies to closed studbooks
A basic tenet of physics is Rudolf Clausius' and Lord Kelvin's statement
of the Second Law of Thermodynamics:
"The amount of energy available for useful work in a given isolated system is decreasing. The entropy is always increasing. Therefore, closed systems cannot perpetually sustain themselves."
In other words, a closed system inevitably always is expending its store of energy and is constantly winding down. An isolated system has no additional source of energy with which to replenish itself. And no system is more "isolated" than a dog breed club's closed studbook. Its "energy" component is its pool of genes. Every breeding decision results in eliminating more and more genes from the very limited pool which a closed studbook contains at its start. Therefore, in no way can the closed studbook be capable of perpetually sustaining itself. From the beginning of the concept of "purebred" breeding, the closed studbook has been destined to degrade into accelerated, irreversible exhaustion.
The breed standard does not mention "pedigree" or the "studbook"
The stated goal of purebred breeding has been to produce dogs which meet a defined "breed standard", which mainly pertains to appearance, structure, and temperament. Breed standards typically do not even mention a requirement that the dogs be descended only from dogs listed in the breed's studbook.
The closed studbook has never really been a necessary corollary to achieve that goal. For example, it is possible to mate together a variety of "mongrels" - note how class snobbery so easily seeps in to the purebred vocabulary - and produce, within as few as three or four generations, a dog which actually meets the breed standard of the cavalier King Charles spaniel. Indeed, if the CKCS breed standard included a "health clause" - that is, requiring that the dog not have certain genetic disorders, such as Chiari-like malformation or mitral valve disease - it would be easier to produce a dog matching the CKCS breed standard from mongrels than it would be by mating purebred cavaliers.
Because the national kennel clubs decreed that their breeds' studbooks be closed, the second law of thermodynamics kicks in and guarantees a foreseeable end point to those breeds' existence. As evidence, the American Kennel Club, founded in 1884, has been predicted to run itself into the ground within the next ten years. This is based upon the rate of declining annual puppy registrations, from a high of over 1,500,000 in 1992 to around 400,000 in 2014*, a decline of over 75% in only the last twenty-two of its 131 years. And just why is that? Pure irrational snobbery, perhaps.
* The AKC was so embarrassed by the declining registrations that it stopped publicizing their numbers in 2008.
So, why not toss out the closed studbook, or at least open it up to outsiders, and let the offspring of any parents vie for matching the breed standard?
Case Study: The low uric acid (LUA) Dalmatian
A tragic example: Up to 2011, all AKC-registered Dalmatians reportedly carried a mutated version of the SLC2A9 gene, which causes exceedingly high levels of uric acid - about ten times that of a normal dog. In research studies, high majorities of males were found to have uric sediment in their bladders, and an estimated 13% to 34% produce potentially painful urate stones which can cause blockages and which may require repeated surgeries to remove.
In an effort to come to the rescue of that breed, in 1973 a very knowledgeable and courageous breeder, Dr. Robert Schaible, cross-bred a Dalmatian bitch with a German shorthaired pointer (not affected with the mutated SLC2A9 gene), producing a litter half of which also did not have the dreadful mutation. These dogs since have been labeled "low uric acid" or LUA Dalmatians. Within three generations after back-crossing those healthy offspring, only the most biased Dalmatian fanciers could detect which dogs were from that cross breeding when compared to champion purebred Dals.
 Nevertheless, the ever so particular
members of the AKC's parent club, the Dalmatian Club of America (DCA), voted twice
- in 1984 and 2008 (by then, the tenth generation of LUA Dals had been
produced) - to reject these healthy dogs' bids to obtain AKC registrations.
In the meantime, all AKC Dalmatian breeders necessarily produced only
litters of dogs with the version of the gene which was certain to cause
exceedingly high levels of uric acid. They all did this intentionally!
Nevertheless, the ever so particular
members of the AKC's parent club, the Dalmatian Club of America (DCA), voted twice
- in 1984 and 2008 (by then, the tenth generation of LUA Dals had been
produced) - to reject these healthy dogs' bids to obtain AKC registrations.
In the meantime, all AKC Dalmatian breeders necessarily produced only
litters of dogs with the version of the gene which was certain to cause
exceedingly high levels of uric acid. They all did this intentionally!
Finally, by the twelfth generation of LUA Dals, which were 99.97% purebreds (see Fiona, at right), even the AKC board of directors had reached the limit of its patience. In November 2010, the AKC board warned the Dalmatian parent club that if its membership did not vote to approve admission of the LUA Dals into the AKC within the following six months, then AKC would take the matter into its own hands and rule on admitting the LUA dogs into the breed's studbook. The parent club read the signals and finally voted to admit the LUA Dals in 2011, after 38 years of irresponsible foot-dragging, during which the club's breeders gleefully continued to produce Dals suffering this potentially agonizingly painful genetic urinary disease.
 So, almost invariably the purebred dog
clubs' studbook fetish trumps
the genetic health of generation after generation of the dogs their breeders produce.
Thus, these degenerate offspring continue to be bred, and their reputations
for sever genetic health defects grow and grow. The recent BBC documentary
television program "Pedigree Dogs Exposed" is evidence of that. As a
consequence, the dog owning public is turned off, repulsed even, by the
selfish, snobbish, anti-health policies of the national kennel clubs.
So, almost invariably the purebred dog
clubs' studbook fetish trumps
the genetic health of generation after generation of the dogs their breeders produce.
Thus, these degenerate offspring continue to be bred, and their reputations
for sever genetic health defects grow and grow. The recent BBC documentary
television program "Pedigree Dogs Exposed" is evidence of that. As a
consequence, the dog owning public is turned off, repulsed even, by the
selfish, snobbish, anti-health policies of the national kennel clubs.
The cavalier clubs still irresponsibly ignore the MVD and the CM/SM breeding protocols
Added to that is the fact that purebred breed clubs often refuse to recognize either the severity of the genetic disorders their breeding practices have brought upon their dogs, or the often simple solutions to dealing with those disorders. For example, both of the CKCS national breed clubs in the United States have refused to endorse the Mitral Valve Disease Breeding Protocol, designed by cardiologists and geneticists to eliminate early-onset MVD in the breed. And, both clubs refuse even to acknowledge the existence of the SM Breeding Protocol, designed by neurologists and geneticists to reduce the incidence of CM/SM in the breed.
 So, we have a combination of (a) the inevitability of the second law of
thermodynamics to waste away an isolated system, like the ubiquitous and
totally unnecessary closed studbook, and (b) the breed clubs' persistent
denial of the reality of at least a partial solution to some of the severe
genetic health disorders which their closed studbooks have brought about.
All this is wrapped in the breed clubs' tuxedo-dressed attitude of elitism,
snobbery, and condescension towards anyone who dares to suggest that the
clubs could be doing something terribly wrong and also could be refusing to
do something absolutely necessary. The victims, of course, are these
purebred dogs, as their genetic health deteriorates with each future
generation.
So, we have a combination of (a) the inevitability of the second law of
thermodynamics to waste away an isolated system, like the ubiquitous and
totally unnecessary closed studbook, and (b) the breed clubs' persistent
denial of the reality of at least a partial solution to some of the severe
genetic health disorders which their closed studbooks have brought about.
All this is wrapped in the breed clubs' tuxedo-dressed attitude of elitism,
snobbery, and condescension towards anyone who dares to suggest that the
clubs could be doing something terribly wrong and also could be refusing to
do something absolutely necessary. The victims, of course, are these
purebred dogs, as their genetic health deteriorates with each future
generation.
Perhaps as predicted, by the year 2025 the purebred dog will be put out of its misery, as the closed studbooks of these miserable dog clubs follow the second law of thermodynamics and degrade into total exhaustion.
RETURN TO TOP
March 25, 2015:
The EPIC trial ends on schedule,
but could a whitewash be in the
works?
Study's objective is changed and findings are disclosed prior to peer review
Such advance disclosures normally are unethical and unprofessional
 In 2010, Boehringer Ingelheim, the manufacturer of Vetmedin (a brand name
for pimobendan)
announced the start of the EPIC Trial, a 360-dog study by 36 veterinary
cardiologists around the world, to determine if the drug could be effective
in delaying the onset of clinical signs of congestive heart failure in dogs
with mitral valve disease. In that announcement, Boehringer Ingelheim's
senior brand manager is quoted stating:
In 2010, Boehringer Ingelheim, the manufacturer of Vetmedin (a brand name
for pimobendan)
announced the start of the EPIC Trial, a 360-dog study by 36 veterinary
cardiologists around the world, to determine if the drug could be effective
in delaying the onset of clinical signs of congestive heart failure in dogs
with mitral valve disease. In that announcement, Boehringer Ingelheim's
senior brand manager is quoted stating:
"The EPIC trial will definitely answer the question: Does pimobendan delay the onset of clinical signs?"
In a press release issued by EPIC Trial co-lead researcher Dr. Jens Haggstrom* on March 16, 2015, it was announced that "The EPIC study has been terminated". No surprise there, because from the beginning of the EPIC Trial back in 2010, it was announced that it would end in early 2015. But, really! A press release to announce the end of a drug study which was scheduled to end anyway? Could that announcement have been just an excuse for issuing a press release at all?
What is surprising is this comment included in that press release:
"The interim analysis indicated that there was clear evidence of benefit of the administration of pimobendan in prolonging the time to the primary endpoint of the study, which was a composite of the development of left-sided congestive heart failure, or death presumed to be cardiac in origin. The interim analysis did not raise any concern over the safety of pimobendan administration." (Emphasis added.)
Unfortunately, there is a lot wrong with that dreadfully vague statement.
Can you spell p-e-e-r r-e-v-i-e-w?
First of all, in the world of scientific
research, it is unusual for research data, much less any results, to be
leaked publicly before peer-reviewing and the official publication of the
peer-reviewed article. Further, it is unheard
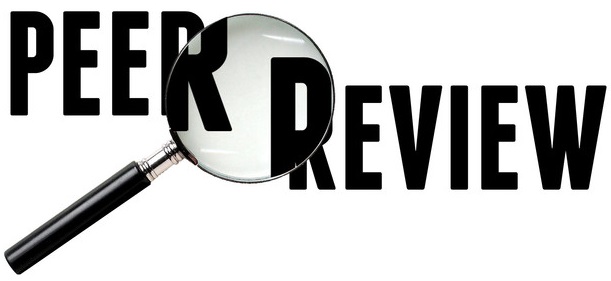 of for there to be an official public
release of any such premature information, over the name of one of the researchers.
Any such prior disclosure normally is considered unethical and
unprofessional in the scientific research arena.**
of for there to be an official public
release of any such premature information, over the name of one of the researchers.
Any such prior disclosure normally is considered unethical and
unprofessional in the scientific research arena.**
So, what is so special about the EPIC Trial that this seemingly unethical, unprofessional, and unheard of press release has been issued? It is far from clear, within the four corners of that press release.
The answer may be tucked into the highlighted portion of that quote above - "or death presumed to be cardiac in origin." You see, from the outset, it never was intended that the EPIC Trial's pre-heart-failure administration of pimobendan end at death.
Here is how the EPIC trial researchers originally stated the objective of their study:
"Investigators will determine if chronic oral administration of pimobendan in dogs with evidence of increased heart size secondary to preclinical MMVD can delay the onset of signs of CHF. Complete EPIC results will be published and distributed, regardless of the outcome.
"Does chronic oral administration of pimobendan in dogs with evidence of increased heart size secondary to preclinical MMVD delay the onset of signs of congestive heart failure?"
In other words, pimobendan would be given to dogs with Stage B2 mitral valve disease (dogs with a loud murmur and some enlargement of the heart but not in heart failure), and once congestive heart failure signs appear, the study ends for that dog. There is nothing there about intending to give the dogs pimobendan until they die, or that doing so would "benefit" the dog.
Now, granted, in the FAQs on the EPIC Trial website, it does state that "The primary endpoint is a composite of the development of left-sided congestive heart failure (CHF) or cardiac death." (All that means is that a particular dog's testing ends either when the dog reaches CHF or if the dog dies instead of reaching CHF.) But surely that did not mean that cardiac death prior to CHF meant that the pimobendan treatment had been a success. It meant the opposite -- that the pimobendan had failed to allow the dog to reach CHF at all. In other words, there would be no "evidence of benefit" if the pimobendan killed a dog which otherwise would have reached CHF.
Since one of the main concerns about administering pimobendan prior to heart failure always has been that it can cause death, and since death before the usual progression to heart failure always has been considered to be a bad thing and not a desirable one, it would be very curious if death prior to heart failure has been added to the EPIC Trial's objective as a normal, desirable end point. ***
A bad smell pervades this EPIC Trial
 This press release is very troubling because it reeks of
an effort to placate the manufacturer of Vetmedin. We feared this from the
beginning, when we urged cavalier owners to not particpate in the EPIC Trial
in our Blog entry, "Beware the pimobendan/Vetmedin 'EPIC clinical trial':
There is no upside."
This press release is very troubling because it reeks of
an effort to placate the manufacturer of Vetmedin. We feared this from the
beginning, when we urged cavalier owners to not particpate in the EPIC Trial
in our Blog entry, "Beware the pimobendan/Vetmedin 'EPIC clinical trial':
There is no upside."
Hopefully, between now and when the actual (presumably peer-reviewed) article on the EPIC Trial is published, responsible professionals will re-take control of this process back from the manufacturer and not suggest that death before reaching congestive heart failure is an acceptable end result of giving their dogs pimobendan.
______
*Lead researcher
Adrian Bosworth issued a nearly identical
press release on March 17, 2015. Co-lead researcher Sonya Gordon
issued an even more egregious
press release on March 24, 2015.
** See,
"What is Ethics in Research & Why
is it Important?", by David B. Resnik, J.D., Ph.D. National Institute of
Health website, 2011: "There are many other activities that the government
does not define as 'misconduct' but which are still regarded by most
researchers as unethical. These are called 'other deviations' from
acceptable research practices and include: ... Bypassing the peer review
process and announcing your results through a press conference without
giving peers adequate information to review your work."
*** In the
"Pimobendan in Congestive Heart Failure (PICO) trial",
a 1996 study of 317 human patients, the researchers found that: "In both
pimobendan groups combined the hazard of death was 1.8 times higher than in
the placebo group."
RETURN TO TOP
March 19, 2015:
Is it 'Back to the Future' for the American Kennel Club?
A degenerate breeding program masquerading as the dogs' champion
 The new Chairman of the Board of the American Kennel Club is the same old
chairman who led the AKC into its decline earlier in this millennium. Ron
Menaker (right) was re-elected chairman by AKC's board of directors this month,
after a three year hiatus while interim chairman Alan Kalter fiddled around
trying to figure out how a million or so "Likes" on Facebook could reverse AKC's
rapid decline.
The new Chairman of the Board of the American Kennel Club is the same old
chairman who led the AKC into its decline earlier in this millennium. Ron
Menaker (right) was re-elected chairman by AKC's board of directors this month,
after a three year hiatus while interim chairman Alan Kalter fiddled around
trying to figure out how a million or so "Likes" on Facebook could reverse AKC's
rapid decline.
Yes, the same Ron Menaker whom we chided in a July 2011 blog entry for not only condemning the factually accurate (as far as cavalier King Charles spaniels are concerned) 2008 BBC television program "Pedigree Dogs Exposed" (PDE), but also actually petitioned the UK Parliament to have the BBC do a documentary attacking PDE's producer, called "Jemima Harrison Exposed"!
To re-hash a bit, Mr. Menaker described PDE as a "piece of sensationalist fiction and tabloid journalism masquerading as a documentary" and an "exercise in media sensationalism". Ironically, he pretty much could have used similar words to describe the AKC these days:
"A degenerate breeding program masquerading as the dogs' champion."
It should come as no surprise that closed studbooks have led to rapid
declines in genetic diversity and the
 production
of sicker and more exaggerated versions of each purebred breed of dogs.
AKC's mantra should be something more like "Cross-breed or die", but Mr.
Menaker appears incapable of seeing that viewpoint.
production
of sicker and more exaggerated versions of each purebred breed of dogs.
AKC's mantra should be something more like "Cross-breed or die", but Mr.
Menaker appears incapable of seeing that viewpoint.
So, the question becomes: Will Chairman Menaker's tired old head-in-the-sand ideas speed up AKC's annual double-digit drop in litter and puppy registrations? We all must wait and see, although perhaps not have to wait as long as the statistically predicted death date of 2025.
RETURN TO TOP
 February 10, 2015:
February 10, 2015:
All that cavalier owners need to know about
the "Reverse Sneeze" or
"Cavalier Snort"
 Occasionally,
excited cavalier King Charles spaniels will suddenly stand still and start
making a very loud snorting sound, over and over, as if they are gagging and
having difficulty breathing. In cavalier circles, this is known as the
"Cavalier Snort" or the "Reverse Sneeze".
A
YouTube video of a cavalier making this sound is here.
Occasionally,
excited cavalier King Charles spaniels will suddenly stand still and start
making a very loud snorting sound, over and over, as if they are gagging and
having difficulty breathing. In cavalier circles, this is known as the
"Cavalier Snort" or the "Reverse Sneeze".
A
YouTube video of a cavalier making this sound is here.
In cavaliers, this gagging sound usually is due to the dog having an elongated soft palate. The palate is the roof of the mouth. It is divided into two parts, the front bony hard palate, and the rear fleshy soft palate. The soft palate separates the nasal passage from the oral cavity. (See the soft palate at the top of the sketch to the right.)
An elongated soft palate is too long for the length of the mouth, so that its tip protrudes into the front of the airway and may get sucked into the laryngeal opening where it may obstruct the normal passage of air into the trachea. This is because the CKCS has a shorter muzzle than the average dog, and therefore all of the dog's breathing apparatus is compressed into a shorter space than the average dog.
When the elongated soft palate protrudes and partially or totally blocks the airway, the dog no longer can breathe through its nose. Since dogs normally breathe through their noses, they continue to try to do so, thereby causing the gagging or snorting sound.
Block the dog's nostrils and make it breathe through its mouth
If the palate is only moderately elongated and does not totally block the airway, most cavaliers are able to pull out of these blockages by themselves. Snorting may be relieved by forcing the cavalier to breathe through its mouth instead of its nose. This may be done by holding the dog's head down and mouth open with one hand while blocking air from entering the nose with the other hand.
In severe instances, the dog may collapse if the airflow is obstructed completely for too long. In such cases, surgical removal of excess tissue from the palate may be necessary. One of those procedures is called "folded flap palatoplasty" (FFP), which both shortens and thins the soft palate. Post surgery prognosis is good for young dogs. They generally may be expected to breathe much easier, with significantly reduced respiratory distress, and display more energy and stamina. Older dogs may have a less favorable prognosis.
In all cases, it is strongly recommended that only board certified veterinary surgeons who also are very experienced at airway surgery, be permitted to perform any type of airway surgery on cavaliers.
(This article has been excerpted from "Brachycephalic Airway Obstruction Syndrome (BAOS) in the Cavalier King Charles Spaniel" on this website.)
RETURN TO TOP
October 20, 2014:
Just Asking: What's up with Vetmedin's 'EPIC Trial'?
It's due to end next year, but some recent indications are ominous
 When
the EPIC Trial was announced in 2010 by the manufacturer of Vetmedin (a
brand name of pimobendan), we did not think it was a wise approach for
studying whether the drug could safely delay the onset of heart failure in dogs
with mitral valve disease (MVD). We went so far as to warn all cavalier
owners to
"Beware the pimobendan/Vetmedin 'EPIC clinical trial': There is no upside"
in an April 2011 blog entry on this page.
When
the EPIC Trial was announced in 2010 by the manufacturer of Vetmedin (a
brand name of pimobendan), we did not think it was a wise approach for
studying whether the drug could safely delay the onset of heart failure in dogs
with mitral valve disease (MVD). We went so far as to warn all cavalier
owners to
"Beware the pimobendan/Vetmedin 'EPIC clinical trial': There is no upside"
in an April 2011 blog entry on this page.
The trial, of up to 360 dogs with MVD murmurs and enlarged hearts (but not yet in heart failure), is scheduled to end in 2015. Each dog was to receive either two pimobendan tablets or placebos daily until the dog reached heart failure. Since the trial started over 4 years ago, presumably many of those dogs by now have reached the heart failure stage of MVD, and their reports should be piling up in the in-boxes of the study's leaders, including Dr. Sonya Gordon of Texas A&M University in the USA and Professor Adrian Boswood in the UK.
We may assume that the 36 cardiologists participating in the EPIC Trial are sworn to secrecy until the final report, which entails drafting, review, approval by at least a majority of them, and peer review before publication in a veterinary journal. However, there are curious indications that some of the results are known and do not look so good for the wannabe peddlers of early-use Vetmedin.
Owners of some of the dogs in the trial are reporting that their dogs
died suddenly, shortly after its start. Some
cardiologists who are among the 36 participants now are talking with renewed emphasis
about the importance of waiting for signs of heart failure before starting
Vetmedin. At least
one other cardiologist recently has openly attacked the trial as being
risky. The EPIC Trial's own website -
epictrial.com --
with its videos and graphics
 and list of names of those 36 cardiologists and
its map showing their locations around the globe and all of its optimistic hype
about Vetmedin before heart failure, has disappeared from the Internet*.
Inquiries to Vetmedin's manufacturer, Boehringer Ingelheim GmbH, go
unanswered.
and list of names of those 36 cardiologists and
its map showing their locations around the globe and all of its optimistic hype
about Vetmedin before heart failure, has disappeared from the Internet*.
Inquiries to Vetmedin's manufacturer, Boehringer Ingelheim GmbH, go
unanswered.
Are these indications that the EPIC Trial has been an epic failure? Just asking ...
* Finally, as of early December 2014, the Epic Trial website is back on line.
RETURN TO TOP
October 13, 2014:
So your cavalier has a heart murmur. What do you do next?
The ACVIM says: Get an x-ray, not an ultrasound!
 Since over half of all cavalier King Charles spaniels may be expected to
develop mitral valve murmurs by age 5 years, it should come as no surprise
when your veterinarian tells you that your cavalier has one. But there is no
reason to panic. The American College of Veterinary Internal Medicine (ACVIM*)
has a sensible list of steps to take once a murmur is first detected in your
CKCS.
Since over half of all cavalier King Charles spaniels may be expected to
develop mitral valve murmurs by age 5 years, it should come as no surprise
when your veterinarian tells you that your cavalier has one. But there is no
reason to panic. The American College of Veterinary Internal Medicine (ACVIM*)
has a sensible list of steps to take once a murmur is first detected in your
CKCS.
For the record, the ACVIM recommends that cavaliers be screened annually by "auscultation" (examination by stethoscope) by board certified cardiologists. Specifically, ACVIM** states:
"Owners of breeding dogs or those at especially high risk, such as Cavalier King Charles Spaniels, may choose to participate in yearly screening events at dog shows or other events sponsored by their breed association or kennel club and conducted by board-certified cardiologists participating in an ACVIM-approved disease registry."
For that reason, CavalierHealth.org has a list of upcoming heart screening clinics in the USA and Canada, which is updated weekly.
Once a murmur is detected by the vet, the first thing to realize is that you do not need to rush your dog to have an ultrasound (echocardiograph) of its heart. In fact, rarely does a cavalier with a mitral valve murmur ever need an ultrasound before the disease reaches heart failure. Instead of an ultrasound, the ACVIM recommends that you get your dog's heart x-rayed to be a "baseline" for measuring the heart size against future x-rays after any heart enlargement takes place. The ACVIM states:
"Thoracic radiography [chest x-ray] is recommended in all patients to assess the hemodynamic significance of the murmur and also to obtain baseline thoracic radiographs at a time when the patient is asymptomatic for CVHD [chronic valvular heart disease]."
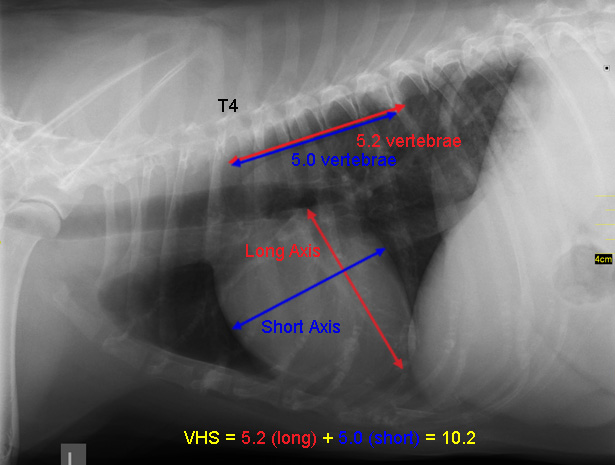 The ACVIM does not recommend that cavaliers with new murmurs be
ultrasounded unless the auscultation and the x-ray do not adequately satisfy
the cardiologist about the true cause of the murmur. Specifically, this is
what the ACVIM states about ultrasounding cavaliers once a mitral valve
murmur is detected:
The ACVIM does not recommend that cavaliers with new murmurs be
ultrasounded unless the auscultation and the x-ray do not adequately satisfy
the cardiologist about the true cause of the murmur. Specifically, this is
what the ACVIM states about ultrasounding cavaliers once a mitral valve
murmur is detected:
"In small breed dogs with typical murmurs, echocardiography is recommended to answer specific questions regarding either cardiac chamber enlargement or the cause of the murmur if those questions are not answered adequately by auscultation and thoracic radiography."
In other words, if the vet heard something unexpected, like a muffled heart sound, or if the dog had something like a suspicion of pulmonary thromboembolism, then an echo after the x-ray would be appropriate.But otherwise, no echo would be needed.
Note that the only "baseline" that the ACVIM recommends for cavaliers with new murmurs is an x-ray and not an ultrasound, as long as the cardiologist is satisfied that the stethoscopic exam and the x-ray confirm the cause of the murmur.
* The ACVIM certifies
veterinary cardiologists. A list of them in the
USA and Canada is available here.
** See the ACVIM's
"Guidelines for the Diagnosis and Treatment of Canine Chronic Valvular Heart
Disease", page 1144.
RETURN TO TOP
October 11, 2014:
Do MVD-affected cavalier King Charles spaniels
really need taurine
supplements?
 There is a popular notion that dogs with mitral valve disease will benefit
from adding taurine (right) to their daily diets. Taurine
(2-aminoethanesulfonic acid) is essential for cardiovascular function as
well as for playing a variety of other fundamental roles in keeping animals
functioning. Fortunately, most all dogs produce sufficient taurine
themselves, as long as they ingest an adequate amount of animal-based
protein. There is no published evidence that dogs with mitral valve disease
are deficient in taruine or would benefit from supplementing it.
There is a popular notion that dogs with mitral valve disease will benefit
from adding taurine (right) to their daily diets. Taurine
(2-aminoethanesulfonic acid) is essential for cardiovascular function as
well as for playing a variety of other fundamental roles in keeping animals
functioning. Fortunately, most all dogs produce sufficient taurine
themselves, as long as they ingest an adequate amount of animal-based
protein. There is no published evidence that dogs with mitral valve disease
are deficient in taruine or would benefit from supplementing it.
There were a couple of reports published in 1997 that found that American Cocker spaniels affected with dilated cardiomyopathy (DCM) became taurine-deficient and in need of taurine supplementation. Apart from the fact that American Cockers and cavaliers have the same last name, there is no established connection between the CKCS and a need for added taurine. Cavaliers are not inherently taurine-deficient, and as a breed, they are not known to develop DCM. Mitral valve disease (MVD) and DCM both affect the dog's heart, but otherwise, they are not related.
Nevertheless, many canine heart supplements include taurine, and even some cardiologists recommend adding taurine to the diets of dogs with mitral valve disease. We are not sure why, because research studies have shown that MVD-affected dogs tend to have higher plasma taurine concentrations than unaffected dogs. In a 1995 study by George A. Kramer, Mark D. Kittleson, Philip R. Fox, Julia Lewis, and Paul D. Pion, for example, they found:
"[P]lasma taurine concentrations were highest in dogs with AVD [acquired valvular disease, e.g, MVD] ... We conclude that plasma taurine concentrations may be increased in dogs with AVD."
 Even
DCM-affected dogs other than American Cockers usually have no taurine
deficiency. Other breeds in which some DCM-affected dogs have been found to
also have taurine deficiencies are the Newfoundland and the Portuguese water
dog.
Even
DCM-affected dogs other than American Cockers usually have no taurine
deficiency. Other breeds in which some DCM-affected dogs have been found to
also have taurine deficiencies are the Newfoundland and the Portuguese water
dog.
In board certified veterinary cardiologist Dr. Rebecca E. Gompf's 2005 article on nutritional therapies, she wrote:
"Because dogs readily make taurine from free sulfur amino acids, only lose a small amount in their bile acids, and can maintain normal blood levels of taurine despite their diets, they do not tend to develop taurine-deficient DCM."
In a 2002 presentation, board certified veterinary cardiologist Dr. Bruce Keene (who conducted one of those 1997 studies of the American Cocker) stated:
"Taurine supplementation is indicated whenever plasma or whole blood taurine concentrations are found to be low. ... [S]upplementation is generally only recommended after discovery of deficiency."
Even Dr. Lisa Freeman, the veterinary nutritionist at Tufts/Cummings veterinary school (with her major financial conflicts for taking money from the notorious major kibble manufacturers and then trashing the dog foods of other manufacturers) has stated in her November 2018 blog:
"Giving taurine is unlikely to prevent DCM unless your dog has taurine deficiency. And given the lack of quality control for dietary supplements, you can introduce new risks to your dog if you give a supplement without evidence that she needs it."
So, the bottom line is that, if you are thinking about giving your cavalier a taurine supplement, check its blood first to see if the dog needs it. The odds are great that no MVD-affected cavaliers will be low in taurine, and remember the old saying: "Too much of a good thing is not a good thing!"
RETURN TO TOP
July 12, 2014:
When NOT to start giving your cavalier
pimobendan (Vetmedin)
 Unfortunately, a few veterinary cardiologists, and a huge number of
general practice vets, have been prescribing pimobendan (brand names
Vetmedin and Cardisure) to cavaliers which have mitral valve disease (MVD)
murmurs but definitely are not yet in heart failure. This is very disturbing
because the premature dosing of pimobendan can kill the dog
which does not need it.
Unfortunately, a few veterinary cardiologists, and a huge number of
general practice vets, have been prescribing pimobendan (brand names
Vetmedin and Cardisure) to cavaliers which have mitral valve disease (MVD)
murmurs but definitely are not yet in heart failure. This is very disturbing
because the premature dosing of pimobendan can kill the dog
which does not need it.
Even some dogs already in heart failure cannot tolerate pimobendan, because one of its consequences is that it strengthens the heart muscle and enables it to pump harder. This is called improving the heart's contractility. If a dog in heart failure still has a strong heart muscle, it does not need to be strengthened, and the pimobendan thereby forces the heart to work much harder than it should.
This is what happened to one of our cavaliers. We noticed that his heart was beating so hard after being given pimobendan that we could see the beats causing his chest hair to vibrate. So we cut back the dosage by half, and then by half again, so that he was getting a quarter of the typical dosage. Finally we discontinued it completely. He had an enlarged heart and he was in heart failure, but the heart muscle remained strong and was doing its job.
Premature administration of pimobendan can overwork the heart to the point of shredding some of its chordae tendineae and thereby causing instant death.
Ask your vet, "WHY?"
So, if you have a cavalier with a mitral valve disease murmur but has no symptoms of heart failure, and your veterinarian recommends starting pimobendan, the first thing you should do is ask him "Why?".
And, show him the manufacturer's warning on the box, about not prescribing it prior to heart failure. It states:
"Contraindications: Vetmedin should not be given ... in cases of hypertrophic cardiomyopathy, aortic stenosis, or any other clinical condition where an augmentation of cardiac output is inappropriate for functional or anatomical reasons.
"Warnings: Only for use in dogs with clinical evidence of heart failure."
See for yourself:
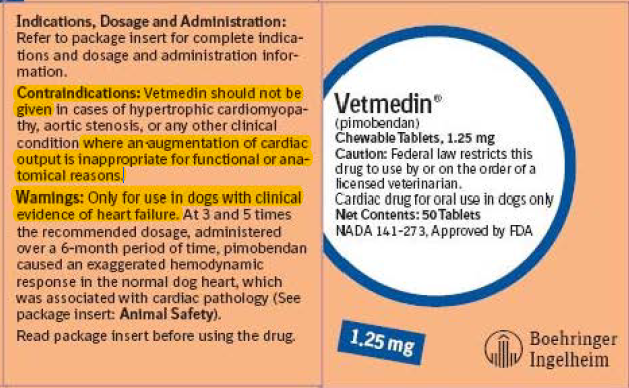
And, point out that Vetmedin's website has this warning:
"The safety of VETMEDIN has not been established in dogs with: Asymptomatic heart disease.
"Use only in dogs with clinical evidence of heart failure."
And, show him the ACVIM consensus statement, which states (on page 1145, top of second column):
"A few panelists considered the use of the following medications for patients in Stage B2 under specific circumstances: pimobendan, ... . The panel felt in general that these treatment strategies needed additional investigation into their efficacy and safety in this patient population before a consensus recommendation could be made."
And, ask him about the current "EPIC study" of 360 pre-heart-failure dogs, being sponsored by Vetmedin's manufacturer and not due to end until 2015, to determine whether or not Vetmedin should be given to pre-heart-failure-dogs. On the EPIC Study website, it specifically states:
"Currently there is no treatment licensed to delay the onset of CHF [congestive heart failure]."
Elsewhere on the EPIC Study website it states:
"There is currently no treatment licensed for the management of preclinical, myxomatous mitral valve disease (MMVD)."
And still on another page of the EPIC Study website it states:
"Treatment of CHF due to MMVD begins when the dog shows clear clinical signs of heart failure, and istailored for the individual dog."
As you see, pimobendan's own manufacturer repeatedly warns against giving the drug to dogs before they are in heart failure.
In other words, ask your veterinarian to satisfy you that his way is better than ALL of the evidence against premature dosing of pimobendan! As Ricky Ricardo would say to Lucy, "You got some splainin' to do!"
RETURN TO TOP
June 18, 2014:
Do-it-yourself diagnosing of congestive heart failure
in your
cavalier King Charles spaniel
"Only respiratory rate predicted the presence of CHF with high accuracy."
E xcept
for prescribing pimobendan, veterinary cardiologists' consensus about
medicating cavalier King Charles spaniels with mitral valve disease
(MVD) is to wait until the dog enters "congestive heart failure" (CHF),
or just "heart failure" (to avoid having to define "congestive"). They
tell us cavalier owners that our dogs with MVD should be brought in and
re-examined regularly - be it every six months or as frequently as every
three months - so that if and when the dog is on the cusp of CHF, the
vet will be ready and able to prescribe a combination of medications -
usually a diuretic, an ACE-inhibitor (in addition to the pimobendan) -
immediately.
xcept
for prescribing pimobendan, veterinary cardiologists' consensus about
medicating cavalier King Charles spaniels with mitral valve disease
(MVD) is to wait until the dog enters "congestive heart failure" (CHF),
or just "heart failure" (to avoid having to define "congestive"). They
tell us cavalier owners that our dogs with MVD should be brought in and
re-examined regularly - be it every six months or as frequently as every
three months - so that if and when the dog is on the cusp of CHF, the
vet will be ready and able to prescribe a combination of medications -
usually a diuretic, an ACE-inhibitor (in addition to the pimobendan) -
immediately.
If it is so important to know exactly when our cavaliers enter CHF, so the drugs may be given promptly thereafter, then exactly how is CHF diagnosed? Can only a veterinarian make that diagnosis? Do only the vets have the necessary equipment? If so, what will happen to our dog if CHF shows up sometime between those periodic visits to the vet?
We know that vets, especially cardiologists, have some very expensive diagnostic equipment for our dogs' heart problems. They include x-ray machines, Doppler echocardiographs (ultrasounds), and electrocardiograph devices (ECG or EKG), all of which may be used to detect CHF. In addition, the vets have expensive blood tests (cardiac biomarkers) to detect CHF. But what good are all of these tools and equipment if our dog enters CHF between visits to the vet?
Simply count the dog's breaths for 15 seconds
 The answer is counting the dog's "respiratory rate"
while asleep, which is something
that cavalier owners can do anytime they are with their dogs. As fancy and
complex as all of the cardiologists' electronic devices may be, and as
sophisticated as their cardiac biomarkers may be, the best single means of
determining when a cavalier enters congestive heart failure is when the
dog's sleeping respiratory rate consistently exceeds 30 or so breaths per minute.
Some cardiologists say 35 or more.
The answer is counting the dog's "respiratory rate"
while asleep, which is something
that cavalier owners can do anytime they are with their dogs. As fancy and
complex as all of the cardiologists' electronic devices may be, and as
sophisticated as their cardiac biomarkers may be, the best single means of
determining when a cavalier enters congestive heart failure is when the
dog's sleeping respiratory rate consistently exceeds 30 or so breaths per minute.
Some cardiologists say 35 or more.
While the dog is sound asleep (but not showing signs of dreaming), count the number of breaths the dog takes in 15 seconds. A rise (inhale) and fall (exhale) of the chest count as one full breath or respiration. Then multiply that number by four to get the number of breaths per minute (bpm). Or, count for 30 seconds and then multiply by two. If that respiratory rate increases by more than 20 percent over 2 to 3 days, or regularly exceeds 30 breaths per minute, many treating veterinarians would advise the dog's owner to report to them.
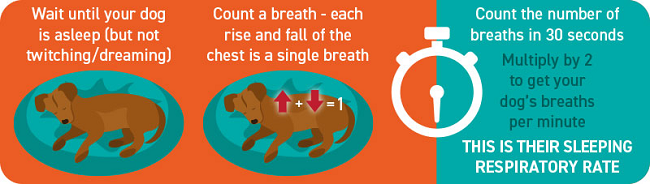
Top cardiologists in the UK and USA have concluded that respiration rate counts are more accurate in predicting the onset of CHF than any other means. In a 2011 study at Ohio State University's veterinary school, Dr. Karsten Schober and a team of researchers compared the respiratory rates of 45 dogs with MVD (including 13 CKCSs) with their cardiac biomarkers and their Doppler echocardiographic indices, and they found that "Only respiratory rate predicted the presence of CHF ... with high accuracy." They concluded that "home monitoring of respiratory rate is simple and very useful in the assessment of CHF in dogs with ... MVD."
In a 2012 study conducted by an international team of cardiologists, they found that "apparently healthy adult dogs generally have mean sleeping respiratory rates [less than] 30 breaths/min and rarely exceed this rate at any time."
As a result of these studies, several cardiologists are recommending that owners become familiar with their MVD-affected cavaliers' normal sleeping breathing rate and effort and keep logs of their sleeping respiratory rates, to establish a baseline rate for each dog, and report when the dogs' rates increase to consistent rates approaching or above 30 to 40 breaths per minute. For example, the University of Pennsylvania's veterinary school advises in a handout available on-line:
"When your dog is at rest, watch their sides rise and fall as they breathe normally. One rise and fall cycle is equal to one breath. Count the number of breaths they take in 15 seconds, then multiply this number by 4 to get total breaths per minute. For example, if you count 8 breaths in 15 seconds, that is equal to 32 (8 x 4) breaths per minute. A normal dog at rest should have a respiratory rate less than 40. If you notice this number increasing consistently, or notice an increase in the effort it takes to breathe, contact your veterinarian."
In her June 2025 article, Prof. Melanie Hezzell stated:
"Monitoring of sleeping respiratory rate (SRR) is recommended in stage B2, as this allows the early detection of CHF. Patients without CHF or with well-controlled CHF are expected to have an SRR below 30 breaths per minute. We recommend that owners contact a veterinarian for advice if the rate is suddenly and persistently over 40 breaths per minute, or if they notice a trend upwards in the breathing rate over some days."
 The vet school at Texas A&M University also has
published a handout
(right) explaining how to keep track of dogs' respiratory rates.
An excellent
YouTube video shows when
The vet school at Texas A&M University also has
published a handout
(right) explaining how to keep track of dogs' respiratory rates.
An excellent
YouTube video shows when
![]() and
how every cavalier owner can count the breaths of their MVD-affected dogs
while they are sleeping or at rest.
and
how every cavalier owner can count the breaths of their MVD-affected dogs
while they are sleeping or at rest.
Infrequent, extremely rapid breathing rates above 100 breaths per minute ( bpm) are commonly called "panting" (usually over 100 bpm) and should not be counted in this test.
Bottom Line: Ask your cavalier's cardiologist (you do have one, don't you?) whether and how you should monitor your dog's respiratory rate for congestive heart failure.
RETURN TO TOP
March 10, 2014:
Dog food companies may be turning a grain-free corner
Some truths about carbohydrate-laden kibbles ooze out of
the petfood industry magazine's March 2014 issue
 Petfood
Industry magazine's March 2014 issue has a picture of a wolf on its cover. It's
cover story is "Should domestic dogs really eat like wolves?" It's subhead asks
"Bio-appropriate petfoods are often meat-first and grain-free, but are they
based on nutrition science?"
Petfood
Industry magazine's March 2014 issue has a picture of a wolf on its cover. It's
cover story is "Should domestic dogs really eat like wolves?" It's subhead asks
"Bio-appropriate petfoods are often meat-first and grain-free, but are they
based on nutrition science?"
Considering that Petfood Industry is the marketing association of the USA's commercial petfood industry, and that the petfood manufacturers' bread-and-butter has been machine-extruded, carbohydrate-laden dry kibble for the past fifty years, one would expect the answer to both of those questions is "No!" - "No, dogs should not eat like wolves" and "No, biologically-appropriate petfoods are not based upon nutrition science".
Well, think again. Petfood companies' "conventional wisdom" is turned on its head in this remarkable issue of the industry's magazine. The wolves article lays waste to the "validity" of feeding dogs carbohydrate-laced kibble, making such heretical politically-incorrect statements as:
"According to 'The Biologically Appropriate Food Concept', conventional dry dog and cat foods appear to be created on the premise that the digestive system of the dog and cat is similar to humans -- with an emphasis on grains and carbohydrates. While some would argue that dogs and cats have adapted since kibble foods were introduced, bio-appropriate petfood makers would counter that their digestive systems remain unchanged.
"'Such evolutionary adaptations require much more time than a mere hundred years or so, and the evolutionary change -- from gross anatomy down to the molecular level -- that would be required for the development of such different digestive capabilities would take much longer than the time that dogs have been living with humans,' the Champion Pet Foods whitepaper points out.
"In the short digestive systems of dogs and cats, plant proteins are far less digestible than meat proteins. High levels of trypsin inhibitors in grain legumes can cause substantial reductions in protein and amino acid digestibilities (up to 50%) in rats and pigs. Certain protein sources are better than others by providing a richer blend of amino acids. These proteins have a high biological value (BV). BV refers to how well the body can actually use the protein."
Veterinary nutritionists' "Pet Humanization" slur is turned against them
In addition, the March issue's second article, "Grain-free petfood: A top trend in the US pet market" (subhead: "Desire for natural products, pet humanization drive this growing segment") reports that discerning pet owners finally are having an impact on the petfood industry by choosing more grain-free foods for their dogs and cats. Admittedly, the author of this article uses the more demeaning slur of "pet humanization" to describe the pet owners' choices of meat protein over corn and other grains. She writes:
"Pet humanization is still a hot topic in the petfood industry today and is characterized by exactly what it sounds like -- pet owners increasingly taking the well-being of their furry companions every bit as seriously as that of any other member of their family. 'Consumers are clearly comfortable splurging on pets because they see them as valued family members, not just everyday animals,' said [Maria Lange, senior product manager for GfK Retail and Technology]."
The fact is that if anyone is guilty of "pet humanization", it is the kibble manufacturers and their bought-and-paid-for "board certified veterinary nutritionists", who have falsely contended that the digestive systems of dogs have evolved to be similar to humans and less wolf-like.
Grain-free pet food sales increased 32% in 2013
 The bottom line of the second article is that grain-free pet food sales
increased 32% in the United States in 2013. Pet owners spent US$1.4 billion on
grain-free dog food products at US pet stores in 2013, according to GfK.
Perhaps, within a year or two, the Science Diet kibbles and their ilk will
become just a nasty experience of the past.
The bottom line of the second article is that grain-free pet food sales
increased 32% in the United States in 2013. Pet owners spent US$1.4 billion on
grain-free dog food products at US pet stores in 2013, according to GfK.
Perhaps, within a year or two, the Science Diet kibbles and their ilk will
become just a nasty experience of the past.
A follow-up question is: What will all of those pro-corn and anti-meat "board certified veterinary nutritionists" do for a living?
RETURN TO TOP
December 12, 2013:
The accordion-muzzled cavalier King Charles spaniel
Why do cavaliers have so many unique disorders of the head?
 The
cavalier King Charles spaniel breed suffers from some fairly unique hereditary
disorders in their beautiful heads, including
Chiari-like
malformation (CM), primary secretory otitis media
(PSOM), progressive hearing loss,
dry eye syndrome,
cerebellar infarcts (strokes), episodic
falling syndrome (EFS), fly catchers syndrome,
periodontal disease, and
temporomandibular joint dysplasia.
CKCSs may not be the only breed with these disorders, but they clearly
have more than their fair share, particularly of CM, PSOM, dry eye, periodontal
disease, strokes, and
EFS.
The
cavalier King Charles spaniel breed suffers from some fairly unique hereditary
disorders in their beautiful heads, including
Chiari-like
malformation (CM), primary secretory otitis media
(PSOM), progressive hearing loss,
dry eye syndrome,
cerebellar infarcts (strokes), episodic
falling syndrome (EFS), fly catchers syndrome,
periodontal disease, and
temporomandibular joint dysplasia.
CKCSs may not be the only breed with these disorders, but they clearly
have more than their fair share, particularly of CM, PSOM, dry eye, periodontal
disease, strokes, and
EFS.
What is there about the cavalier that explains this uniqueness?
There has been much discussion of late about "brachycephalic" breeds of dogs. The term "brachycephalic" means short-nosed and refers to dogs with short muzzles, noses, and mouths. "Brachy" means short and "cephalic" means head. The throat and breathing passages in brachycephalic dogs often are undersized or flattened. The head's soft tissues are not proportionate to the shortened nature of the skull, and the excess tissues tend to increase resistance to the flow of air through the upper airway (nostrils, sinuses, pharynx and larynx). The consequent disorders are labeled "brachycephalic airway obstruction syndrome" (BAOS).
 Many cavalier fanciers will argue, vehemently, that cavaliers are not
brachycephalic. They point out that most CKCS muzzles are significantly
longer than such breeds as the English bulldog, pug, King Charles spaniel
(English toy spaniel), French bulldog, and Pekingese. And, indeed, they have an
obvious point; the muzzle of the average cavalier appears to be proportionally
longer than those other breeds.
Many cavalier fanciers will argue, vehemently, that cavaliers are not
brachycephalic. They point out that most CKCS muzzles are significantly
longer than such breeds as the English bulldog, pug, King Charles spaniel
(English toy spaniel), French bulldog, and Pekingese. And, indeed, they have an
obvious point; the muzzle of the average cavalier appears to be proportionally
longer than those other breeds.
Nevertheless, cavaliers seem to have at least their share of brachycephalic disorders - inhalation issues caused by their compressed breathing apparatus - especially an elongated soft palate - not to mention sets of very jumbled teeth and gums (see photo at right). Also, veterinary researchers have unanimously classified the cavalier King Charles spaniel as brachycephalic in their research articles on the subject.
The CKCS's head has been treated like an accordion!
 Apart
from their relatively longer muzzle, cavaliers' brachycephalism stands apart for
one other reason: The cavalier is the only brachycephalic breed that
was created by purposefully elongating an already snub-nosed snout.
While the English bulldog, pug, King Charles spaniel (KCS), French bulldog, and
Pekingese were fashioned by generation after generation of selective breeding to
shorten the muzzle, the CKCS was bred to lengthen the already
quite snub-nosed King Charles spaniel. Thus, the cavalier's head has been
treated as if it was an accordion - first shortening it to attain the King
Charles spaniel breed standard (see KCS skull at near right), and then,
beginning in the 1920s, selecting KCS breeding stock, and perhaps
out-crossing, to produce longer snouts (see CKCS skull at far right).
Apart
from their relatively longer muzzle, cavaliers' brachycephalism stands apart for
one other reason: The cavalier is the only brachycephalic breed that
was created by purposefully elongating an already snub-nosed snout.
While the English bulldog, pug, King Charles spaniel (KCS), French bulldog, and
Pekingese were fashioned by generation after generation of selective breeding to
shorten the muzzle, the CKCS was bred to lengthen the already
quite snub-nosed King Charles spaniel. Thus, the cavalier's head has been
treated as if it was an accordion - first shortening it to attain the King
Charles spaniel breed standard (see KCS skull at near right), and then,
beginning in the 1920s, selecting KCS breeding stock, and perhaps
out-crossing, to produce longer snouts (see CKCS skull at far right).
(Specimens from the collections of the Albert Heim Foundation, Museum of Natural History, Bern.)
Consider this series of profiles (below), beginning at the left with an 1850 King Charles spaniel, then a 1910 champion King Charles spaniel, then a 1930 second generation champion cavalier King Charles spaniel, then a 1960 champion CKCS, and finally a 2010 champion cavalier. The accordion affect between the 1850, 1910, and 1930 versions is most noticeable.
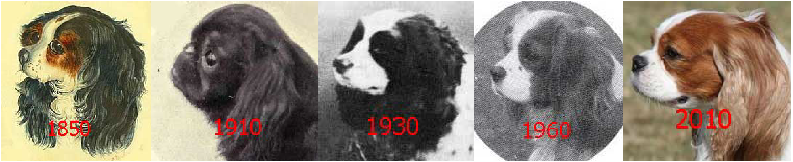
If you consider that breeding to shorten the head will compress the dog's breathing apparatus, what happens when those jumbled contents then are stretched out again? Certainly, there can be no assurance that the end result would be perfectly relocated airway passages and teeth in the exact position they would have been had no bunching had taken place to begin with. Unlike an accordion, the dog's skull is not equipped with a built-in spring. Once jumbled by compression, it is very possible that the decompressed airways remain confusingly jumbled but just in some other manner. We know that to be the case just by looking in the cavalier's mouth. Despite a longer muzzle than the KCS, many of the cavalier's overcrowded teeth are in anything but a functional position.
We also know that the CKCS's hereditary head disorders, particularly PSOM, dry eye, and CM, are the result of the jumbled consequences of brachycephalism, while cerebellar infarcts are believed to be due to CM altering blood flow to the brain. But, in no other brachycephalic breed are these hereditary diseases anywhere close to being so prevalent. As an example, in a March 2006 article, the radiologists authors noted that, while the canine "tympanic cavity is usually quite large and rounded", in the cavalier, "it is smaller and flatter." The accordion effect of breeding cavaliers could explain the uniqueness of these disorders.
RETURN TO TOP
 September 23, 2013:
September 23, 2013:
All that cavalier owners need to know
about primary secretory otitis media (PSOM)
 Primary
secretory otitis media (PSOM) has become more frequently diagnosed in cavalier
King Charles spaniels. It consists of a highly viscous mucus plug which fills
the dog's middle ear and may cause the tympanic membrane to bulge. PSOM has been
reported almost exclusively in cavaliers.
Primary
secretory otitis media (PSOM) has become more frequently diagnosed in cavalier
King Charles spaniels. It consists of a highly viscous mucus plug which fills
the dog's middle ear and may cause the tympanic membrane to bulge. PSOM has been
reported almost exclusively in cavaliers.
Because the pain and other sensations in the head and neck areas, resulting from PSOM, are similar to some symptoms caused by syringomyelia (SM), some examining veterinarians may have mis-diagnosed SM in cavaliers which actually have PSOM and not SM.
The cause of PSOM is unknown. It is suspected to be due to a dysfunction of the middle ear or the Eustachian (auditory) tube: either (a) the increased production of mucus in the middle ear, or (b) decreased drainage of the middle ear through the auditory tube, or (c) both.
The principal symptoms are moderate to severe pain in the head or neck, holding the neck in a guarded position, and tilting the head. Other signs may include scratching at the ears, itchy ears, head tilt, excessive yawning, crying out in pain, ataxia, drooping ear or lip, inability to blink an eye, rapid eyeball movement, facial paralysis or nerve palsy, Vestibular disease, some loss of hearing, seizures, and fatigue. These symptoms, in many cases, are very similar to those of syringomyelia and, to some extent, to those of progressive hereditary deafness. Therefore, the examining veterinarian should take care to consider these other possible causes of the dog's symptomatic behaviors.
PSOM may be detected by veterinary neurology or dermatology specialists from either magnetic resonance imaging (MRI) or a computed tomography (CT) scan. Both require that the dog be under general anesthesia. It also may be observed using an operating microscope with good lighting and at a suitable magnification.
Treatment traditionally has consisted of performing a myringotomy, making a small cut in the eardrum (tympanic membrane), followed by flushing the middle ear to force out the mucus plug. Topical and/or systemic corticosteroids and antibiotics then are administered. The procedure may have to be repeated, in some cases several times, depending upon how the dog responds. An alternative procedure is a ventral bulla osteotomy,which involves making an incision on the under side of the neck behind the jaw bone. The auditory bulla, a hollow bony sheath that encloses parts of the middle ear, then is exposed and is opened.
Some specialist veterinarians have been prescribing N-Acetyl-L-Cysteine (NAC), a mucolytic -- mucus thinning agent or expectorant -- for cavaliers with PSOM, following surgeries.
(This article has been excerpted from "Primary Secretory Otitis Media (PSOM) in the Cavalier King Charles Spaniel" on this website.)
RETURN TO TOP
 August 26, 2013:
August 26, 2013:
All that cavalier owners need to know
about their dogs' blood platelets
 Up
to half of all cavalier King Charles spaniels may have both an abnormally low
number of blood platelets and oversized platelets. Despite the low platelet
counts, the typical cavalier's blood platelets function normally, and the dog
does not appear to experience any health problems due to either the size or
fewer numbers of its platelets. There are, however, limited exceptions to this
typical situation.
Up
to half of all cavalier King Charles spaniels may have both an abnormally low
number of blood platelets and oversized platelets. Despite the low platelet
counts, the typical cavalier's blood platelets function normally, and the dog
does not appear to experience any health problems due to either the size or
fewer numbers of its platelets. There are, however, limited exceptions to this
typical situation.
An excessively low platelet count normally is a sign which tends to alarm general practice veterinarians, and so it is vitally important that cavalier owners alert their vets about this benign condition in the breed when blood tests are ordered.
No treatment is recommended unless the dog shows other symptoms of a blood-related disorder. Cavaliers should not be treated for immune-mediated thrombocytopenia (IMT) as a precaution. Dog really suffering from IMT must be treated quickly, usually with intravenous doses of immunosuppressive drugs -- steroids, azathioprine, cyclosporine A and others -- to save the dog's life. Such treatments are severe and could do major damage to the healthy cavalier with nothing more than a low platelet count.
Most commercial laboratories use an automated counting system for blood cells, which determine cell types on the basis of their size and volume. Because cavaliers' platelets are so large, automated blood cell counters may not recognize platelets as being platelets and undercount them, thereby inaccurately lowering the platelet count. Researchers have found that CKCS platelet counts using three different automated systems underestimated the actual counts determined manually. Antech Diagnostics, the largest veterinary diagnostic laboratory, has specifically stated on its website that:
"Platelets in this breed should be counted manually, because automated blood cell counters cannot distinguish the large platelets from erythrocytes and therefore underestimate the true platelet count."
An accurate platelet count can be obtained by visually counting the cells. Also, because the large platelets are so fragile, any blood samples should be extracted very carefully. Therefore, all blood samples from cavaliers should be taken in a very careful manner and preferably only from the dog's jugular vein, using a large bore needle, and then should be examined only under a microscope by an experienced clinical pathologist before making a diagnosis of low platelet count.
(This article has been excerpted from "Blood Platelets in Cavaliers" on this website.)
RETURN TO TOP
August 10, 2013:
What if the American Kennel Club ceased to exist?
The cavalier's future after the AKC's death spiral
 The
American Kennel Club (AKC) reportedly is withering away. Every year since 1992,
its litter and puppy registration numbers have been dropping by as much as
double digit percentages. Over the course of the last 21 years*, registrations
have declined by over two-thirds, even as the number of dogs in American homes has
increased. Observers have predicted that if AKC's registrations continue to drop
at the same rate, it will be out of business by 2025.
The
American Kennel Club (AKC) reportedly is withering away. Every year since 1992,
its litter and puppy registration numbers have been dropping by as much as
double digit percentages. Over the course of the last 21 years*, registrations
have declined by over two-thirds, even as the number of dogs in American homes has
increased. Observers have predicted that if AKC's registrations continue to drop
at the same rate, it will be out of business by 2025.
* From 1.528,392 in 1992 to 479,404 in 2013.
To continue to survive financially, the AKC has been upping its event fees, such as for conformation shows, obedience, rally, and agility trials, and tracking tests. It even has increased its litter and puppy registration fees, despite the declining registrations. But such counter-intuitive alternative fund-raising initiatives have not stanched its cash crisis. AKC also has cut back on its funding of its programs of kennel inspections, DNA profiling, canine good citizens, search-and-rescue, Canine Health Foundation, legislative issues, etc.
So, what would no AKC mean to the cavalier King Charles spaniel? There are two national CKCS clubs in the United States. One, the American Cavalier King Charles Spaniel Club (ACKCSC), is an official "parent club" for the breed, in the AKC. The other, the Cavalier King Charles Spaniel Club, USA (CKCSC,USA), is independent of the AKC and has been in existence since the 1950s, long before AKC recognition of the cavalier in 1995.
 If
AKC goes kaput, so too would its CKCS parent club. Except for the occasional
"specialty" conformation shows, parent clubs rely totally upon the AKC for
direction, litter and puppy registration, rules, judging, and show organization.
To survive post-AKC, the parent club would have to learn how to do what the
CKCSC,USA has been doing all along for the past 57 years. It would have to re-organize completely,
from the ground up, including registering dogs, creating rules, approving
judges, organizing its own shows around the country, and finding enough
volunteers to do what has been done for them by AKC kennel (all-breed) clubs up
to now.
If
AKC goes kaput, so too would its CKCS parent club. Except for the occasional
"specialty" conformation shows, parent clubs rely totally upon the AKC for
direction, litter and puppy registration, rules, judging, and show organization.
To survive post-AKC, the parent club would have to learn how to do what the
CKCSC,USA has been doing all along for the past 57 years. It would have to re-organize completely,
from the ground up, including registering dogs, creating rules, approving
judges, organizing its own shows around the country, and finding enough
volunteers to do what has been done for them by AKC kennel (all-breed) clubs up
to now.
Ironically, after AKC's demise, the CKCSC,USA may end up being the only show in town for those cavalier breeders who, since 1995, have turned their backs and thumbed their noses at the original cavalier club in the USA.
RETURN TO TOP
July 9, 2013:
All that cavalier owners need to know about
natriuretic peptides tests (ANP and BNP)
 There has been much research into attempting to diagnose mitral valve
disease (MVD), and more
particularly, to diagnose the onset of congestive heart failure (CHF) in dogs by
measuring "cardiac biomarkers", such as blood plasma concentrations of the natriuretic peptides: atrial
natriuretic peptide (ANP) and brain natriuretic peptide (BNP).
There has been much research into attempting to diagnose mitral valve
disease (MVD), and more
particularly, to diagnose the onset of congestive heart failure (CHF) in dogs by
measuring "cardiac biomarkers", such as blood plasma concentrations of the natriuretic peptides: atrial
natriuretic peptide (ANP) and brain natriuretic peptide (BNP).
Natriuretic peptides are hormones manufactured and secreted by areas of the heart. A test of natriuretic peptides measures the quantity of the natriuretic peptides in the dog's blood. Elevated levels of these natriuretic peptides in the blood may be directly related to heart defects, and natriuretic peptides in the blood become elevated only after the heart has to pump harder to compensate for the disorder. In particular, BNP is secreted by the left ventricle in response to heart wall stretching or stress.
Our bottom line on this topic has best been stated by Dr. Jennifer L. Garcia in "The NT-proBNP assay: A portent of heart health." in dvm360:
"For conditions such as mitral valve disease, this test may be of limited value because a diagnosis can be readily made by thorough auscultation and documentation of a heart murmur. In these cases, the assay also has limited utility in determining disease severity; thoracic radiography is preferred."
Translated, she is saying that stethoscopic examinations, combined with periodic x-rays of the heart, are more effective in diagnosing MVD and CHF than any blood tests.
History of natriuretic peptide testing
A 2003 study (conducted by Drs. Kristin A. MacDonald, Mark D. Kittleson, Coralie Munro, and Philip Kass of the University of California at Davis) has shown a positive correlation between BNP and heart disease and CHF in dogs. In that study, BNP increased with the progressively increased severity of mitral valve disease and CHF. For every 10-pg/mL increase in BNP, the 2003 study's dogs' mortality rate increased approximately 44% over the four months of the study. In a 2005 study, Drs. William E. Herndon, Justine A. Lee, Kenneth J. Drobatz, and Matthew J. Ryan concluded that "With further investigation, this new BNP assay may someday provide a widely available noninvasive diagnostic test with rapid turnaround time to help diagnose and/or treat heart disease and congestive heart failure in the dog."
However, in earlier studies (1994 and 1997) conducted by Drs. Jens Haggstrom, Kjerstin Hansson, Clarence Kvart, and others, the researchers have suggested that BNP levels in cavaliers with mitral regurgitation did not rise as dramatically as in humans, and that N-terminal (NT)-proANP (NT-proANP) may better reflect the severity of mitral regurgitation in cavalier King Charles spaniels than NT-proBNP tests.
Four trademarked names for NT-proBNP tests are Canine CardioCare (Veterinary Diagnostics Institute), Canine VetSign CardioSCREEN (Guildhay Ltd.), Cardiopet proBNP (IDEXX Laboratories), and Antech Cardio-BNP (Antech Diagnostics). There have been studies showing the effectiveness of these types of tests for dogs suffering from asymptomatic occult dilated cardiomyopathy (DCM), which is not the same disorder as MVD and is not known to be a genetic problem for cavalier King Charles spaniels.
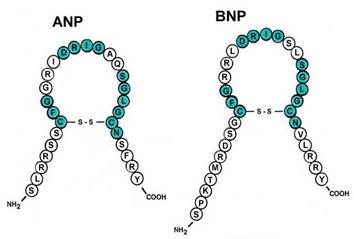 Whichever test (NT-proBNP or NT-proANP) is found to be more accurate for
detecting MVD, it is believed by some researchers that the test may be
useful in assisting examining veterinarians in deciding whether or not
detected heart murmurs are innocent or are pathologic in nature. However, in
a 2007 study of 54 CKCSs by
Drs. Tarnow, Pedersen, Kvart, and others from
Denmark and Sweden, they found that "Natriuretic peptides are elevated in
cavalier King Charles spaniels with congestive heart failure but not in dogs
with clinically inapparent mitral valve disease."
Whichever test (NT-proBNP or NT-proANP) is found to be more accurate for
detecting MVD, it is believed by some researchers that the test may be
useful in assisting examining veterinarians in deciding whether or not
detected heart murmurs are innocent or are pathologic in nature. However, in
a 2007 study of 54 CKCSs by
Drs. Tarnow, Pedersen, Kvart, and others from
Denmark and Sweden, they found that "Natriuretic peptides are elevated in
cavalier King Charles spaniels with congestive heart failure but not in dogs
with clinically inapparent mitral valve disease."
In a May 2008 report by Drs. Mark A. Oyama, Philip R. Fox, John E. Rush, Elizabeth A. Rozanski, and Michael B. Lesser of 119 dogs, they found that "Serum NT-proBNP concentration was significantly higher in dogs with cardiac disease than in control dogs, and a serum NT-proBNP concentration > 445 pmol/L could be used to discriminate dogs with cardiac disease from control dogs with a sensitivity of 83.2% and specificity of 90.0%. In dogs with cardiac disease, serum NT-proBNP concentration was correlated with heart rate, respiratory rate, echocardiographic heart size, and renal function." They concluded that, "For dogs with cardiac disease, serum NT-proBNP concentration could be used to discriminate dogs with and without radiographic evidence of cardiomegaly and dogs with and without congestive heart failure." And that, "Results suggested that serum NT-proBNP concentration may be a useful adjunct clinical test for diagnosing cardiac disease in dogs and assessing the severity of disease in dogs with cardiac disease."
In a May 2009 report from Sweden, the researchers concluded: "Plasma concentrations of the natriuretic peptides measured at re-examination could predict progression in regurgitant jet size."
In a 2012 study of 1,134 dogs, including 37 cavaliers, Stephen J. Ettinger, Giosi Farace, Scott D. Forney, Michelle Frye, and Andrew Beardow concluded that "This biomarker [NT-proBNP] may be a useful tool for staging of cardiac disease and identifying cardiac-related coughing or dyspnea in this species."
In a 2013 study of 36 dogs, none being CKCSs, a team of Japanese researchers concluded: "These results indicated that plasma ANP rose with an increase in the volume overload of the left side of the heart. Plasma ANP discriminated cardiomegaly from non-cardiomegaly caused by asymptomatic MMVD. We conclude, therefore, that plasma ANP concentrations may be a clinically useful tool for early diagnosis of asymptomatic MMVD in dogs."
In an April 2013 report, a team of German veterinary cardiologists studied 352 dogs and found that: "NPs [natriuretic peptides] in canine MMVD are useful to discriminate between asymptomatic dogs and dogs with CHF. Due to a large overlap of NP-concentrations between the groups, NPs do not seem to be useful to differentiate between dogs in stages B1 and B2. Interpretation of NT-proBNP and proANP values should include consideration of sex-specific differences."
In a January 2017 report, researchers focused upon the inherent variability of NTproBNP in all dogs -- both healthy and MVD-affected -- and how those random variations, called biologic variability, affects the accuracy of population-based reference ranges of NTproBNP readings. They measured NTproBNP in healthy dogs and dogs in stages B1, B2, and C of mitral valve disease, to estimate biologic variability and calculate an Index of Individuality (IoI) for each dog. Of the 28 MVD-affected dogs in the study, 14 -- 50% -- were cavalier King Charles spaniels, along with 10 healthy control dogs. They found that MVD-affected dogs had a lower inherent variability of NTproBNP compared to healthy dogs, and that, as a group, MVD-dogs required a change of 58.2% for NTproBNP to be outside the range of inherent biologic variability and indicate a change in disease. They determined that population-based reference ranges for NTproBNP may have limitations. They stated that:
"It is important for veterinarians to have an understanding of how much a biomarker value could change over time due to randomness vs. disease progression in an individual dog. ... Monitoring serial individual changes in NTproBNP values may be clinically relevant in addition to using population-based reference ranges to determine changes in disease status."
This study suggests that a one-time test may not provide an accurate result, and that many repeats of that test are required over an extended period of time.
Why these blood tests are not necessary to diagnose MVD and CHF
Nevertheless, it appears that veterinary cardiologists and other cardio-specialists should be quite capable of detecting mitral valve prolapse (MVP) murmurs and distinguishing between them and flow murmurs or other innocent varieties of heart murmurs. Since BNP in the blood becomes elevated only after the heart has to pump harder to compensate for the disorder, the question then is: When does the heart start working so hard that BNP levels start to go up? In the cavalier King Charles spaniel's version of heart defects -- mitral valve disease due to deteriorating valve flaps -- there are no immediate external symptoms. It is not yet clear from research studies thus far, as to whether the heart becomes labored enough to produce increased levels of BNP before auscultation is able to detect the murmurs from minimal backflow of blood leaking through the mitral valve flaps. Advocates of BNP testing do represent that that studies of BNP and cardiomyopathy show that BNP is elevated before the onset of signs and murmur. But it does not yet appear that BNP testing is an any earlier warning system for MVD than auscultation.
One possible uniquely valuable use for natriuretic peptides tests is if the dog is approaching congestive heart failure (CHF) without any symptoms. In that case, natriuretic peptides tests, combined with "Left Chambers on Aorta ratio" greater than 4,5, the veterinarian may begin administering ACE inhibitors, pimobendan, and other drugs immediately even though the dog is asymptomatic. See Dr. Gerard Le Bobinnec's proposal in this report to the 2010 WSAVA Congress. See, also, the 2012 report of the PREDICT Cohort Study, which found that measurements of left heart size (using the "left atrial to aortic root dimension ratio [LA:Ao]") and plasma NT-proBNP concentration independently estimate risk of first-onset of CHF in dogs with MVD. It correctly predicted first-onset of CHF in 72.5% of cases out of 82 dogs, which included cavaliers.
Dr. Oyama has stated that natriuretic peptide tests may also be useful to properly diagnose a dog known to suffer from congestive heart failure and also is in respiratory distress. He said that, "When dogs come into veterinary hospitals in respiratory distress, it's sometimes difficult to know if they are having a respiratory or heart problem. Such a test could speed effective treatment and also help decide if a dog should be referred to a veterinary cardiologist before undergoing more expensive testing."
(This article has been excerpted from "Mitral Valve Disease and the Cavalier King Charles Spaniel" on this website.)
RETURN TO TOP
July 7, 2013:
The cavalier King Charles spaniel is pre-disposed to ...
The list gets longer
 In
the past two months, we have added two more webpages to CavalierHealth.org -
kidney disease and
pneumocystis pneumonia. Contrary to some breeders' claims, we hate to do
that; we hate to have to increase our list of genetic disorders to which the
cavalier King Charles spaniel is pre-disposed. But when dogs are suffering and
dying of genetic diseases and their owners don't know why, we feel the need to
continue their education about the extraordinary list of serious genetic
problems in our breed.
In
the past two months, we have added two more webpages to CavalierHealth.org -
kidney disease and
pneumocystis pneumonia. Contrary to some breeders' claims, we hate to do
that; we hate to have to increase our list of genetic disorders to which the
cavalier King Charles spaniel is pre-disposed. But when dogs are suffering and
dying of genetic diseases and their owners don't know why, we feel the need to
continue their education about the extraordinary list of serious genetic
problems in our breed.
Chronic kidney disease and pneumocystis pneumonia are killers. The recent deaths of some CKCSs have prompted us to upload these two new webpages. We urge you all to read about them and become aware of their symptoms. You may save your dogs' lives by recognizing signs which often elude your veterinarians. One of the unfortunate facts about owning cavaliers is that many vets are totally clueless about some of these serious diseases, mainly because they are either unique to our breed or darn close to it.
The cavaliers' "pre-disposed" list? Here it is:
Mitral valve disease (MVD)
Chiari-like malformation (CM)
Syringomyelia (SM)
Low blood platelets (idiopathic asymptomatic
thrombocytopenia)
Periodontal disease
Cerebellar infarcts - strokes
Anal sac disorders
Chronic pancreatitis
Brachycephalic airway obstruction syndrome (BAOS)
Curly coat syndrome
Deafness - progressive hereditary hearing loss
Intervertebral disk disease (IVDD)
Diabetes mellitus
Dry eye syndrome
Eosinophilic stomatitis
Facial nerve paralysis
Hip dysplasia (HD)
Idiopathic epilepsy
Episodic falling syndrome
Exocrine pancreatic insufficiency (EPI)
Fly catchers syndrome
Primary secretory otitis media (PSOM) - glue ear
Chronic kidney disesase
Masticatory muscle myositis (MMM)
Muscular dystrophy
Obesity
Patellar luxation
Pneumocystis pneumonia
Temporomandibular
joint dysplasia
Aortic thrombosis
Aortic thromboembolism
RETURN TO TOP
March 26, 2013:
CKCSC,USA embarks on an offensive "charm offensive"
"Forever Guardians of the Cavalier" is its new spin on a BIG LIE!
 The
Cavalier King Charles Spaniel Club, USA has noticed its ever-declining
membership over the past several years and has determined that the problem is
not its fault, but instead has
been due to the "economy" and poor public relations. At its 2012 Annual General Meeting, president Bruce
Henry noted that membership has dropped from 2,000+ five years ago to the
current 1,500 range. He attributed this decline "to the general economy
since there is no change in the way our club operates."
The
Cavalier King Charles Spaniel Club, USA has noticed its ever-declining
membership over the past several years and has determined that the problem is
not its fault, but instead has
been due to the "economy" and poor public relations. At its 2012 Annual General Meeting, president Bruce
Henry noted that membership has dropped from 2,000+ five years ago to the
current 1,500 range. He attributed this decline "to the general economy
since there is no change in the way our club operates."
If president Henry wanted to be more pointed about the growing insignificance of the CKCSC,USA, he could have added that over the past ten years, membership has dropped by well over half!
Apparently, the CKCSC,USA president is oblivious to the more likely real reason for the membership drop, which is that "there is no change in the way our club operates." The way the CKCSC,USA has been operating since the departure of president Anne Eckersley (below right) in 2002 perhaps is the real reason for the lack of interest in joining -- and renewing memberships in -- the "Old Club". It made a major change for the worse back then, and, as Mr. Henry noted, it has not changed since.
The big change
 The
2002 change? When the post-Eckersley presidents and their boards took charge of the
CKCSC,USA, they rejected the health-consciousness of the Eckersley-led board of
directors (BOD). Recall that in 1998, president Eckersley presided at the
International Symposium on Mitral Valve Disease (MVD), where a panel of
veterinary cardiologists and geneticist unveiled the
MVD Breeding
The
2002 change? When the post-Eckersley presidents and their boards took charge of the
CKCSC,USA, they rejected the health-consciousness of the Eckersley-led board of
directors (BOD). Recall that in 1998, president Eckersley presided at the
International Symposium on Mitral Valve Disease (MVD), where a panel of
veterinary cardiologists and geneticist unveiled the
MVD Breeding
 Protocol. Remember that? At the time, in 1998 (CKCSC,USA's
"Year of the Heart!" -- see its logo at left), it was a major
announcement, offering cavalier breeders the
solution to breeding litter after
litter of cavaliers with early-onset MVD. The Eckersley BOD also unanimously
endorsed the MVD Breeding Protocol and actually
urged its members to follow it! They also created the CKCSC,USA Health Registry,
to keep track of cavaliers which did not develop MVD until after their
fifth birthday. Remember the CKCSC,USA Health Registry?
Protocol. Remember that? At the time, in 1998 (CKCSC,USA's
"Year of the Heart!" -- see its logo at left), it was a major
announcement, offering cavalier breeders the
solution to breeding litter after
litter of cavaliers with early-onset MVD. The Eckersley BOD also unanimously
endorsed the MVD Breeding Protocol and actually
urged its members to follow it! They also created the CKCSC,USA Health Registry,
to keep track of cavaliers which did not develop MVD until after their
fifth birthday. Remember the CKCSC,USA Health Registry?
 But with the retirement of the Eckersley administration, her successors
unanimously
have dumped the MVD Breeding Protocol. In their
narrowed minds, it effectively has been air-brushed away, as if that 1998 MVD
Symposium never happened, just like old-fashioned Soviet Union censorship.
But with the retirement of the Eckersley administration, her successors
unanimously
have dumped the MVD Breeding Protocol. In their
narrowed minds, it effectively has been air-brushed away, as if that 1998 MVD
Symposium never happened, just like old-fashioned Soviet Union censorship.

Since then, the CKCSC,USA's memberships -- largely non-breeder pet owners -- have plummeted by 50+%, and it has become an indistinguishable step-sister of the AKC's parent club, the American Cavalier King Charles Spaniel Club. The ACKCSC has been notorious for ignoring the breed's genetic health problems, and since 2002, the CKCSC,USA has been tagging along right behind. Both clubs deny the existence of the MVD Breeding Protocol and the Syringomyelia Breeding Protocol.
The big lie
 So, back to the present: The current CKCSC,USA BOD has unveiled its
much-heralded solution to its lousy membership numbers. It is a combination of a
new slogan, "Forever Guardians of the Cavalier" (below at right), and a
chant of tedious "Watchwords" (which includes a Big Lie):
So, back to the present: The current CKCSC,USA BOD has unveiled its
much-heralded solution to its lousy membership numbers. It is a combination of a
new slogan, "Forever Guardians of the Cavalier" (below at right), and a
chant of tedious "Watchwords" (which includes a Big Lie):
 "We
are Forever Committed to the goodwill of the Cavalier;
"We
are Forever Committed to the goodwill of the Cavalier;
We are Forever Historians of the Cavalier - we are the history of the breed, and
will always be;
We are Forever Protectors of the Cavalier;
We are Forever Dedicated to the health of the Cavalier;
We are Forever Joyful owners of the Cavalier;
We are Forever in Love with the Cavalier;
and lastly, and most important,
We are Forever Guardians of the Cavalier."
And so it goes. The Old Club's solution to the lack of interest in it is to Spin a Big Lie about cavaliers' health. Maybe this should be its new logo:
RETURN TO TOP
December 18, 2012:
AVMA's House of Nannies aims at homeopathic vets
AVMA is bent upon endorsing veterinary malpractice
 Obviously,
the AVMA (American Veterinary Medical Association) leadership feels threatened
by the complexity and success of homeopathy. So what does it do? It lashes out
in ignorance ... again. (It lashed out in August against raw food diets because
they were hurting the vets' sales of kibble.
See here.) In both instances, AVMA defends its hostility upon the pretext of baseless
concerns about health and hygiene. The AVMA is beginning to look like a mass version of the Nanny of
New York, Mayor Bloomberg (left).
Obviously,
the AVMA (American Veterinary Medical Association) leadership feels threatened
by the complexity and success of homeopathy. So what does it do? It lashes out
in ignorance ... again. (It lashed out in August against raw food diets because
they were hurting the vets' sales of kibble.
See here.) In both instances, AVMA defends its hostility upon the pretext of baseless
concerns about health and hygiene. The AVMA is beginning to look like a mass version of the Nanny of
New York, Mayor Bloomberg (left).
At its January 5, 2013 meeting, the AVMA's House of Delegates (read: House of Nannies) probably will pass overwhelmingly this resolution:
"Homeopathy Has Been Identified as an Ineffective Practice and Its Use Is Discouraged
"RESOLVED, that the American Veterinary Medical Association (AVMA) affirms that --
"1. Safety and efficacy of veterinary therapies should be determined by scientific investigation.
"2. When sound and widely accepted scientific evidence demonstrates a given practice as ineffective or that it poses risks greater than its possible benefits, such ineffective or unsafe philosophies and therapies should be discarded.
"3. In keeping with AVMA policy on Complementary and Alternative Veterinary Medicine, AVMA discourages the use of therapies identified as unsafe or ineffective, and encourages the use of the therapies based upon sound, accepted principles of science and veterinary medicine.
"4. Homeopathy has been conclusively demonstrated to be ineffective."
AVMA's premise is a thoughtless lie
Of course, the entire premise of this resolution is a thoughtless lie, as the much more competent American Holistic Veterinary Medical Association has pointed out in its response. Click here to read it.
The AVMA nannies' arrogant adulation of "scientific investigation" is known as "scientism". In his recent article in The New Atlantis, titled "The Folly of Scientism", biologist Austin L. Hughes nails these AVMA hypocrites when he points out:
"Advocates of scientism today claim the sole mantle of rationality, frequently equating science with reason itself. Yet it seems the very antithesis of reason to insist that science can do what it cannot, or even that it has done what it demonstrably has not. ... Scientism claims that science has already resolved questions that are inherently beyond its ability to answer ... Continued insistence on the universal competence of science will serve only to undermine the credibility of science as a whole. The ultimate outcome will be an increase of radical skepticism that questions the ability of science to address eventhe questions legitimately within its sphere of competence."
AVMA reacts like a hurtin' dog
It is quite ironic that a group of veterinarians whose bag-o-tricks pretty much is limited to antibiotics, steroids, vaccines, indiscriminate neutering, and Science Diet, would condemn homeopathy as "conclusively demonstrated to be ineffective." So, the AVMA leadership is proving once again that its instinctive reaction to successful veterinary care that they do not understand, is to lash out like a hurtin' dog (see at right). When will the AVMA learn that it is not wise to endorse veterinary malpractice? When it forbids vets from using diagnostic and treatment modalities which have been proven to be effective for thousands of years, it is asking to be sued, big time.
Post Script: On January 5, 2013, the AVMA's House of Delegates chose to kick this resolution back for further review. It may raise its ugly head again, at its Spring 2013 meeting. We shall see ...
RETURN TO TOP
September 27, 2012:
Dog food companies lie, and allergic dogs may die
 Let's
say that your dog has a raging skin condition that is driving him crazy with
itching and has resulted in gooey infections all over his body. Your
veterinary dermatologist suspects a severe allergic reaction to beef and pork,
and so he prescribes venison for your dog to eat. You feed your pet a dog food
which states clearly on the can that it contains venison and no beef or pork.
But, your dog's allergy gets worse instead of better. What's up?
Let's
say that your dog has a raging skin condition that is driving him crazy with
itching and has resulted in gooey infections all over his body. Your
veterinary dermatologist suspects a severe allergic reaction to beef and pork,
and so he prescribes venison for your dog to eat. You feed your pet a dog food
which states clearly on the can that it contains venison and no beef or pork.
But, your dog's allergy gets worse instead of better. What's up?
What's up is that dog food companies lie about the ingredients of their products.
In an August 2012 study by ELISA Technologies Inc., manufacturers of ten out of twenty-one tested commercial dog foods falsified the contents of their products by either including ingredients specifically excluded on the label or not including ingredients specifically advertised on the label. For instance:
• A food labeled as containing venison, contained no venison or deer at all, and instead contained beef and pork;
• A food labeled "lamb" contained no lamb and contained pork instead;
• A food labeled "chicken meal" contained pork instead;
• Foods labeled "no gluten" or "grain-free" in fact contained gluten and grain levels four times higher than allowable amounts.
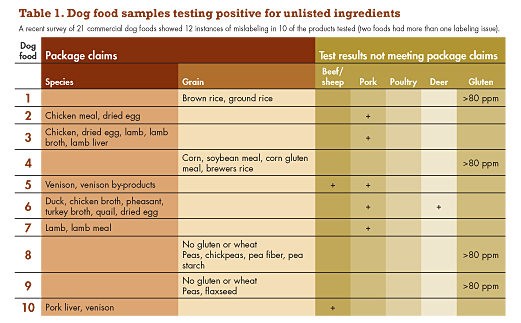
Commercial dog food companies are notorious for switching advertised ingredients, depending upon the varying costs of those ingredients. This August 2012 report clearly substantiates that fact.
When a dog is suspected of having a serious food allergy, veterinary dermatologists typically recommend that the dog be fed an "elimination" diet, by feeding ingredients, usually protein sources, the dog has never had before. For example, if the dog has been fed a typical dry food, usually containing corn, wheat, or other grains, the vet's recommendation is to exclude the corn and grains and feed a particular meat as the protein source. If the allergic dog has been fed beef, the vet might prescribe venison instead.
This study proves that owners of food-allergic dogs cannot rely upon the ingredient lists of dog foods to assure themselves that their dogs are no longer being fed the foods which are causing their allergic reactions. These dog food manufacturers are putting allergic dogs at great risk by falsifying the ingredients described on the packaging, all to save a buck.
RETURN TO TOP
September 26, 2012:
Update on Hill's Science Diet junk food
Hill's finally dumps its "superior nutrition" corn and chicken by-products
 Earlier
this year we blogged "The insidious mind
control over clueless veterinarians by Hill's Pet 'Nutrition'", in
which we pointed out that many veterinary students have been brainwashed by
Hill's about its Science Diet dog food, and that these veterinarians continue
their nutritional cluelessness throughout their professional careers.
Earlier
this year we blogged "The insidious mind
control over clueless veterinarians by Hill's Pet 'Nutrition'", in
which we pointed out that many veterinary students have been brainwashed by
Hill's about its Science Diet dog food, and that these veterinarians continue
their nutritional cluelessness throughout their professional careers.
In that blog entry, we emphasized the horrendous main ingredients in Hill's Science Diet dry food: (a) because its corn and chicken by-products really are totally indefensible as being "superior" to real meat as daily sources of protein for dogs; and (b) because so many veterinarians, including "board certified veterinary nutritionists", have prostituted themselves by actually declaring that corn and by-products are better than real meat.
Well, on September 11, Hill's announced* that it is re-formulating its crappiest dry food, Science Diet, by offering a "quality protein first ingredient" (instead of the current "ground whole grain corn"), and "no chicken by-product". This is the first change of ingredients in Science Diet's 44 year history!
Wow! Without corn and chicken by-products, what will Hill's lapdog veterinary nutritionists and all the other sycophantic veterinarians have to rave about? Will they recant their prior praise for Hills' junk food ingredients of corn and by-products? Will they stop claiming that non-meat chicken by-products are "superior" for dogs than, say, a fresh chicken breast? Will they stop boasting that if corn was good enough for the American Indians, it is good enough for dogs? Has Hill's thrown all of these bootlicking vets under the bus?
 Mind
you, Hill's did not make this change willingly. Hill's U.S. President Kostas
Kontopanos brags in its news release that its "Science Diet is Veterinarians' #1
choice to feed their own pets." (Imagine the scary thought that, for the past 44
years, more veterinarians have chosen Science Diet to feed their own pets than
any other pet food. And we have been trusting their judgment to keep our pets
healthy!) He goes on:
Mind
you, Hill's did not make this change willingly. Hill's U.S. President Kostas
Kontopanos brags in its news release that its "Science Diet is Veterinarians' #1
choice to feed their own pets." (Imagine the scary thought that, for the past 44
years, more veterinarians have chosen Science Diet to feed their own pets than
any other pet food. And we have been trusting their judgment to keep our pets
healthy!) He goes on:
"We took a food that already delivered precisely balanced nutrition, industry leading quality and great taste and will make it even better by adding the natural ingredients that pet parents want."
So, Hill's grudgingly concedes that, despite Science Diet's "superior nutrition, backed by clinical research", we stupid pet owners no longer are falling for the hype like all of those veterinarians have. Hill's president pleads further: "We also want to be pet parents' #1 choice, with the ingredients you prefer, the uncompromising nutrition that more than 50 precisely balanced nutrients deliver and the quality you can trust."
So, this sea-change after 44 years is not being done to improve the nutritional quality of Science Diet's ingredients. Oh no. Hill's insists that its corn and by-products always have been the best source of pet nutrition there can be. Hill's is doing this solely because picky pet owners are more concerned about "natural ingredients".
Now, don't get too excited about this "new-but-not-necessarily-improved" Science Diet. We don't know yet what the "quality protein first ingredient" will be. And, we also realize that "natural ingredients" means absolutely nothing in the pet food industry. All we know for sure is that Hill's claims that the current first two ingredients, corn and chicken by-products, will be gone from the top of the ingredients list. Is it just a coincidence that corn and chicken prices have skyrocketed recently?
Post Script: It is January 2013 already, Hill's. Where is this new Science Diet? Hill's promised in September 2012 that it would introduce its new version of Science Diet, with "natural ingredients", in December 2012. So, where is it? And, what is it? Hill's still has not even told us what the new ingredients are.
RETURN TO TOP
August 3, 2012:
The US cavalier clubs contemptuously
keep whistling past our breed's graveyard
 In
November 2011, the UK's
Advisory Council on
the Welfare Issues of Dog Breeding identified its "first eight problems
which cause serious health and welfare issues for some dogs" as follows:
In
November 2011, the UK's
Advisory Council on
the Welfare Issues of Dog Breeding identified its "first eight problems
which cause serious health and welfare issues for some dogs" as follows:
• Brachycephalic airway obstruction syndrome
• Limb defects (including hip and elbow dysplasia)
• Ocular disease secondary to conformational problems
• Heart disease with a known or suspected inherited basis
• Syringomyelia
• Epilepsy
• Skin conditions with a known or suspected inherited basis
• Issues arising from lack of responsible ownership (including problems such as separation-related behavioural issues and obesity)
Do any of these sound familiar to owners of cavalier King Charles spaniels? Well, seven of them certainly are the most serious problems affecting the CKCS. And, two of them -- inherited heart disease and syringomyelia -- are, by far, more severe in the cavalier than in any other breed of dog. Among these eight serious problems, only inherited skin conditions are not commonplace among the cavalier. Otherwise, the UK Advisory Council might just as well have been writing about only one breed -- ours.
So, what are the US cavalier King Charles spaniel clubs doing about these serious problems? Thus far, absolutely nothing. And there really is no reason to expect that they ever will do anything.
Mitral valve disease (MVD) has been identified as a widespread genetic problem in the
breed for several decades. Over half of all cavaliers are expected to have MVD
by their fifth birthday, and nearly 100% by their tenth year. It is the leading
killer of CKCSs. In most breeds, death is more often due to cancer or accidents,
 but in the cavalier it is MVD. In 1998, a panel of veterinary geneticists and
cardiologists recommended to the US cavalier clubs a breeding protocol designed
to eliminate early-onset MVD in the breed within as few as three
generations. Neither national cavalier club endorses the breeding protocol, and
one of those clubs, the AKC's parent club for cavaliers, refuses to
acknowledge the breeding protocol's existence.
but in the cavalier it is MVD. In 1998, a panel of veterinary geneticists and
cardiologists recommended to the US cavalier clubs a breeding protocol designed
to eliminate early-onset MVD in the breed within as few as three
generations. Neither national cavalier club endorses the breeding protocol, and
one of those clubs, the AKC's parent club for cavaliers, refuses to
acknowledge the breeding protocol's existence.
Similarly, syringomyelia (SM) has been identified as an excruciatingly painful genetic problem in the CKCS for over a decade. It is rampant in the breed; over half of all cavaliers are believed to have SM, and 95% to have Chiari-like malformation, which is part of the cause of SM and its severe pain. Since 2005, veterinary neurologists have designed breeding protocols to rid the breed of SM. However, neither US cavalier club has even acknowledged the existence of any such breeding protocol, much less recommended that it be followed by breeders.
The US cavalier clubs continue to skirt along their merry ways, ignoring any realistic solutions to these severe, breed-wide genetic health problems, and thereby encouraging their breeders to compound the extent and severity of MVD and SM in each and every future generation of cavalier King Charles spaniels.
RETURN TO TOP
June 14, 2012:
The insidious mind control over clueless veterinarians
by Hill's Pet "Nutrition"
 Ever
wonder why so many veterinary clinics have stacks of bags of Science Diet dog
food for sale in their waiting rooms? It probably is because so many vet schools
do not teach companion animal nutrition to their
students. Instead, these many schools delegate to Hill's Pet Nutrition, the
maker of Science Diet, the diet and nutrition curriculum taught to their
veterinary students.
Ever
wonder why so many veterinary clinics have stacks of bags of Science Diet dog
food for sale in their waiting rooms? It probably is because so many vet schools
do not teach companion animal nutrition to their
students. Instead, these many schools delegate to Hill's Pet Nutrition, the
maker of Science Diet, the diet and nutrition curriculum taught to their
veterinary students.
 Dr. Karen Becker, DVM, who authored
Dr. Becker's Real Food for Healthy Dogs and Cats, observed recently:
Dr. Karen Becker, DVM, who authored
Dr. Becker's Real Food for Healthy Dogs and Cats, observed recently:
"Most veterinary students don't learn about species-appropriate pet diets in vet school. The only food discussed is processed, commercial pet formulas."
For nearly all vet students, their schools' nutrition classes have consisted of visits by commercial pet food marketeers to talk about their products. Consider this observation by a veterinarian who graduated from the University of Pennsylvania's veterinary school:
"When I was in veterinary school, we received little education in nutrition (and from walking into the average veterinary clinic today, I assume nothing has changed). Precious little was taught on how to keep the pet carnivore healthy for longevity. The small animal nutrition text was published by a major pet food company and given (not sold) to students."
That major pet food company was Hill's. Consider this telling admission in DVM Newsmagazine:
"Hill's provides financial and educational support to nearly every veterinary college in North America, as well as to veterinary students attending those institutions. This commitment to the profession includes Hill's sponsored teaching programs, residencies and faculty programs in veterinary schools and teaching hospitals all over the world. ...
"Hill's has shown its commitment to the partnership with MSU by providing support to many student groups and student activities; covering costs for students to attend the SCAVMA Symposium; providing students with the textbook Small Animal Clinical Nutrition and other various handouts; ... ." DVM Newsmagazine. Aug. 2004;35(8):38.
That veterinary school textbook, "Small Animal Clinical Nutrition", is published by Mark Morris Institute, which is owned by Hill's. Dr. Mark Morris was the creator of Science Diet kibble.
Hill's " Feeding Programs" -- like pabulum to vet students
 In
most USA vet schools, Hill's offers "Feeding Programs", by which it sells its
pet foods to students and faculty at majorly reduced cost and donates the sales
funds to student groups and scholarships. At each school, one or two students
are appointed as "Hill's Contacts" -- not unlike Lenin's useful
idiots -- to keep lines of communication open between the
unsuspecting students and the pet food conglomerate.
In
most USA vet schools, Hill's offers "Feeding Programs", by which it sells its
pet foods to students and faculty at majorly reduced cost and donates the sales
funds to student groups and scholarships. At each school, one or two students
are appointed as "Hill's Contacts" -- not unlike Lenin's useful
idiots -- to keep lines of communication open between the
unsuspecting students and the pet food conglomerate.
Some vet schools have taken the Hill's bait, hook-line-and-sinker. The University of Florida has a large, permanent display of Hill's Science Diet in the middle of its emergency clinic waiting room. Hill's also is a major benefactor at this vet school, even funding a professorship. See this JAVMA article, "Ethical considerations raised by the provision of freebies to veterinary students", for more details and the ethics involved.
Now, this academic/business relationship would not be so insidious if Hill's Science Diet was a good, nutritive dietary product. But it is not. Here is the list of ingredients in Science Diet adult dry food:
"Ground Whole Grain Corn, Chicken By-Product Meal, Animal Fat
(preserved with mixed tocopherols
 and citric acid), Dried Beet Pulp, Soybean
Oil, Dried Egg Product, Flaxseed, Potassium Chloride, Iodized Salt, Choline
Chloride, vitamins (L-Ascorbyl-2-Polyphosphate (source of vitamin C), Vitamin E
Supplement, Niacin, Thiamine Mononitrate, Vitamin A Supplement, Calcium
Pantothenate, Biotin, Vitamin B12 Supplement, Pyridoxine Hydrochloride,
Riboflavin, Folic Acid, Vitamin D3 Supplement), Vitamin E Supplement, minerals
(Ferrous Sulfate, Zinc Oxide, Copper Sulfate, Manganous Oxide, Calcium Iodate,
Sodium Selenite), preserved with Mixed Tocopherols and Citric Acid,
Beta-Carotene, Rosemary Extract."
and citric acid), Dried Beet Pulp, Soybean
Oil, Dried Egg Product, Flaxseed, Potassium Chloride, Iodized Salt, Choline
Chloride, vitamins (L-Ascorbyl-2-Polyphosphate (source of vitamin C), Vitamin E
Supplement, Niacin, Thiamine Mononitrate, Vitamin A Supplement, Calcium
Pantothenate, Biotin, Vitamin B12 Supplement, Pyridoxine Hydrochloride,
Riboflavin, Folic Acid, Vitamin D3 Supplement), Vitamin E Supplement, minerals
(Ferrous Sulfate, Zinc Oxide, Copper Sulfate, Manganous Oxide, Calcium Iodate,
Sodium Selenite), preserved with Mixed Tocopherols and Citric Acid,
Beta-Carotene, Rosemary Extract."
Where's the meat???
 Ingredients must be listed on the label in decreasing order by weight. For
Hill's Science Diet, the first item is corn, which means that there is
more corn in the mix than anything else. Corn is a cheap filler ingredient with
little nutritional value. It is not a natural source of food for dogs and is
very difficult for them to digest. The second item is chicken
by-product meal. Chicken by-products in dog food do not include meat
and instead contain cheap,
unsavory ingredients ground into the mix, like stomach contents, beaks,
feathers, feet, and entrails. But have no fear, because all of it then is
cooked to death two separate times, changing the structure of proteins for the
worse, and destroying vitamin A, vitamin E, and the B-group vitamins.
Ingredients must be listed on the label in decreasing order by weight. For
Hill's Science Diet, the first item is corn, which means that there is
more corn in the mix than anything else. Corn is a cheap filler ingredient with
little nutritional value. It is not a natural source of food for dogs and is
very difficult for them to digest. The second item is chicken
by-product meal. Chicken by-products in dog food do not include meat
and instead contain cheap,
unsavory ingredients ground into the mix, like stomach contents, beaks,
feathers, feet, and entrails. But have no fear, because all of it then is
cooked to death two separate times, changing the structure of proteins for the
worse, and destroying vitamin A, vitamin E, and the B-group vitamins.
No dog should be required to live on this junk. And yet, seemingly intelligent veterinarians tout Science Diet to their patients' owners as "Vets' #1 Choice for their Own Pets".*
* By the way, Hill's Science Diet kibble cat food does not include any meat, either.
Some veterinarians have been so taken by the Hill's mind-numbing indoctrination efforts, that they actually endorse corn and by-products as nutritional ingredients in pet food. Dr. Bridget Edgren, DVM, of All Pets Animal Hospital in Boulder, Colorado, a Colorado State University vet school graduate (where Hill's Feeding Program lures the students) recently authored an article titled "Finding the right food for your pet". Her ignorance about dog nutrition is obvious when she writes:
"Corn ... is a nutritionally superior grain compared to the others because it provides a balance of nutrients not found in other grains. ... Contrary to popular belief, by-products are not hooves, feathers, and beaks, which have no nutritive value. By-products are not harmful and actually have excellent nutritive value."
Yeah, sure.
After all, corn was good enough for the Indians
 Dr. Sherry Lynn Sanderson, DVM, PhD, of the University of
Georgia's veterinary college and a University of Minnesota vet school graduate
(both schools have Hill's Feeding Programs) wrote "Raw Diets: Do They Make
You Want To BARF?", in which she fervently defends corn as a main
ingredient in dog food. She writes:
Dr. Sherry Lynn Sanderson, DVM, PhD, of the University of
Georgia's veterinary college and a University of Minnesota vet school graduate
(both schools have Hill's Feeding Programs) wrote "Raw Diets: Do They Make
You Want To BARF?", in which she fervently defends corn as a main
ingredient in dog food. She writes:
"If one considers that corn was a main staple in the diet of Native Americans for many years, it is difficult to understand how critics can claim that corn is a filler used in pet foods."
Sad. Her point? She offers no clue. Chickens eat more corn than the American Indian ever did, but neither humans nor fowl are dogs. And this lady is a board certified veterinary nutritionist!
And, Dr. Sanderson is not unique. Another board certified veterinary nutritionist, Dr. Lisa M. Freeman, DVM, PhD, of Tufts University's Cummings School of Veterinary Medicine (another sucker-school for Hill's Feeding Program), also sings the praises of corn and by-products as the major sources of protein, instead of real meat. She writes in "Answering Owners' Questions About Pet Foods" (as if she actually is trying to be helpful to those owners), this incredible statement:
"Some owners are concerned about using diets that contain any vegetable-based proteins, such as soybean or corn. These are NOT added as fillers and contain important nutrients. There is no reason why 'grain free' foods are better for either dogs or cats. ... Pet food ingredients have strict definitions so meat by-products, for example, are not allowed to contain the non-nutritious animal parts that people sometimes worry about (by-products refer to the non skeletal muscle meat - in other words, the organs)"
 Not true, and totally irresponsible. Remember, by definition,
"meat by-products" do not include any meat.*
Not true, and totally irresponsible. Remember, by definition,
"meat by-products" do not include any meat.*
* The AAFCO definition of "poultry by-product meal: Consists of the ground, rendered, clean parts of the carcasses of slaughtered poultry, such as necks, feet, undeveloped eggs, and intestines, exclusive of feathers except in such amounts as might occur unavoidably in good processing practices."
Why this love affair of so many veterinarians with corn and by-products as the major ingredients in dog foods? The answer likely is Hill's indoctrination programs at the earliest stages of their veterinary education. Junk in; junk out.
Logically, what these "nutritionists" claim makes no sense. Humans, who are far less carnivorous that dogs, are not advised to eat highly cooked, dry, and processed foods instead of fresh, whole food-based diets. Why, then, are kibble and other highly-processed non-meat foods more appropriate for pets? To the contrary of all this pro-kibble hype from these "nutritionists", research studies that have not been funded by commercial pet fund manufacturers have reached the opposite -- and more obvious -- conclusion that balanced home-prepared meals are much more healthful for our dogs than commercial diets prepared by pet food conglomerates. For example, in a 2003 Belgium study of 522 dogs*, the researchers found that dogs fed a species-appropriate homemade diet lived 32 months longer on average than dogs fed commercially available dog foods.
* Relations Between the Domestic Dogs' Well-Being and Life Expectancy. Lippert, G., & Sapy, B. Prince Laurent Foundation Price, 2003.
 Post Script:
Has the AVMA now
legitimized veterinary nutrition malpractice? On August 3, 2012*, the American Veterinary
Medical Assn. (AVMA) voted overwhelmingly to condemn the feeding of
home-prepared raw food to
dogs and cats. Not surprisingly, the AVMA's meeting was heavily funded by Hill's
and by Purina, another producer of junk dog food. So, these vets apparently have
learned nothing beyond what the commercial pet food manufacturers indoctrinated
them about in vet school, and continue to wallow in their self-imposed
ignorance. The question now is: Has the AVMA legitimized veterinary nutrition malpractice?
Post Script:
Has the AVMA now
legitimized veterinary nutrition malpractice? On August 3, 2012*, the American Veterinary
Medical Assn. (AVMA) voted overwhelmingly to condemn the feeding of
home-prepared raw food to
dogs and cats. Not surprisingly, the AVMA's meeting was heavily funded by Hill's
and by Purina, another producer of junk dog food. So, these vets apparently have
learned nothing beyond what the commercial pet food manufacturers indoctrinated
them about in vet school, and continue to wallow in their self-imposed
ignorance. The question now is: Has the AVMA legitimized veterinary nutrition malpractice?
* According to the AVMA website, in the four months preceding this AVMA vote, over 60 commercial brands of dog and cat food were recalled, nearly all for "possible Salmonella contamination". Despite these massive recalls of kibble and canned pet foods, AVMA chose to condemn only pet owners for feeding healthful raw food diets to their dogs and cats. Pet owners have been feeding raw diets to their dogs and cats for decades, yet to date, not one documented case of raw pet food causing illness in humans has been reported.
RETURN TO TOP
June 3, 2012:
Congratulations to Her Majesty, lover of cavaliers!
 The
Diamond Jubilee of Her Majesty, Queen Elizabeth II! This is a once in several lifetimes' event for the peoples of
the United Kingdom and the Commonwealth realms. For the first time in 115 years,
their monarch has served 60 years, and only for the second time in the history
of the monarchy.
The
Diamond Jubilee of Her Majesty, Queen Elizabeth II! This is a once in several lifetimes' event for the peoples of
the United Kingdom and the Commonwealth realms. For the first time in 115 years,
their monarch has served 60 years, and only for the second time in the history
of the monarchy.
 The ties of the cavalier King Charles spaniel to Britain are
many and obvious. The breed's name owes itself to one of its kings. But for the
prompt and willing
response
of UK breeders of the English toy spaniel to the challenge of an American,
Roswell Eldridge, in 1926 (the same year the Queen was born), there would be no CKCS breed. Through World War II,
those British breeders rescued and salvaged the fledgling breed.
The ties of the cavalier King Charles spaniel to Britain are
many and obvious. The breed's name owes itself to one of its kings. But for the
prompt and willing
response
of UK breeders of the English toy spaniel to the challenge of an American,
Roswell Eldridge, in 1926 (the same year the Queen was born), there would be no CKCS breed. Through World War II,
those British breeders rescued and salvaged the fledgling breed.
And, thanks to Her Majesty for her total dedication to her life-long job of serving as her realm's sovereign. At age 86 years, she seems indefatigable in dutifully offering herself this weekend in ceremony after ceremony, rain or shine, hours on end, all with grace and dignity. She truly is an amazing person, "a living flag"!
And while she may be a backyard breeder of a lengthy royal line of inbred corgis, the photo above attests that she also loves cavalier King Charles spaniels! May God save the Queen and the cavalier King Charles spaniel!
RETURN TO TOP
May 9, 2012:
When ignorance (stupidity?) guides cavalier PSOM research, and the federal government funds it
Dr. Charles Bluestone doesn't even know what "PSOM" stands for
 What
do you get when a medical researcher who thinks chimpanzees are in his own
pedigree and that the cavalier King Charles spaniel "has been bred over 300 years to have a short
snout", decides to solve the mystery of what he calls "persistent secretory otitis media" in
our breed? Answer: You get Charles D. Bluestone, M.D., professor of
otolaryngology at the University of Pittsburgh School of Medicine (UPMC).
What
do you get when a medical researcher who thinks chimpanzees are in his own
pedigree and that the cavalier King Charles spaniel "has been bred over 300 years to have a short
snout", decides to solve the mystery of what he calls "persistent secretory otitis media" in
our breed? Answer: You get Charles D. Bluestone, M.D., professor of
otolaryngology at the University of Pittsburgh School of Medicine (UPMC).
Yes, this man is convinced that his ancestors were chimpanzees, despite the lack of any evidence to prove it.* He apparently has blind faith in such unproven theories, which is not a good thing for a research scientist. And yes, he obviously knows nothing factual about the cavalier King Charles spaniel, beyond being able to identify one in a photograph.
* His alleged "evidence"? He irrelevantly and erroneously asserts: "Chimpanzees share an astounding 98.4% of their genetic code with us." Actually, using Dr. Bluestone's intellectually shallow means of DNA comparisons, the similarity is more like below 70%, under the most optimal alignment conditions. The 30+% difference represents almost 35 million single nucleotide changes and 5 million insertions or deletions. By his same simplistic standard, the lowly house mouse shares more of our genetic code -- 99% -- than does the chimpanzee. The notion of man's alleged descent from chimpanzees has long been rejected by knowledgeable evolutionists and creationists, alike. (See, e.g.: "The common chimp [Pan troglodytes] and human Y chromosomes are 'horrendously different from each other', says David Page of the Whitehead Institute for Biomedical Research in Cambridge, Massachusetts." The fickle Y chromosome, Nature, Jan. 2010;463[14]:149.) Why Dr. Bluestone bothers to bring the topic up in a report about PSOM is beyond comprehension. Click here for some more interesting reading about Dr. Bluestone's credibility.
He doesn't even know the name of the disease he claims to be researching. He repeatedly has called PSOM "persistent secretory otitis media" instead of its real name, "primary secretory otitis media". Scientists really ought to know the name of what they are researching.
But, with the full weight of federal funding behind him and his co-conspirator, UPMC's J. Douglas Swarts, Ph.D., he is determined to prove that 300 years of breeding the cavalier for its "short snout" altered its palate muscles to keep its Eustachian tube from operating correctly, thereby causing "persistent secretory otitis media" in "up to 40%", or "50%", or "greater than 50%" (pick one) of the breed. Never mind that the modern-day cavalier was created less than 85 years ago and has been bred to have a longer snout - not a shorter one - and that the percentage of cavaliers with PSOM has not been determined.*
* If you want to learn more about PSOM, click here.
When does ignorance morph into stupidity?
Dr. Bluestone's lack of knowledge about the cavalier King Charles spaniel goes way beyond sloppy research. He is so wrong about this breed in so many ways that it is impossible to determine whether he is monumentally ignorant or just flat stupid. Where is his intellectual curiosity? Has he not researched the breed's founding in the years following Roswell Eldridge's challenge in 1926? Has he not learned that the cavalier's longer muzzle sprung from the shorter muzzle of the King Charles spaniel? Does he not even care to learn the actual name of the disorder he has decided to research?

(Specimens from the collections of the Albert Heim Foundation, Museum of Natural History, Bern.)
Note in the comparison of the breeds' skulls above: the King Charles spaniel skull is at the left, and the skull of the cavalier King Charles spaniel is at the right.
How does federal funding fit into this mess? Leave it to the National Institutes of Health (NIH)* to have wasted our tax dollars on this "research": Human evolutionary history: Consequences for the pathogenesis of otitis media, published in Otolaryngology -- Head & Neck Surgery in December 2010.
* Federal NIH funding fits Dr. Bluestone's modus operandi: "Bluestone submitted numerous grant applications to the NIH throughout the 1970s and 1980s and ultimately was awarded approximately $17.4 million. At the same time, Bluestone began receiving funding from various pharmaceutical companies to test the effectiveness of their antibiotics in treating otitis media. Collectively, this industry funding totaled approximately $3.4 million. ... Cantekin claims that as early as 1976, he raised with Bluestone his failure to list his industry funding on his NIH grant applications, but Bluestone allegedly brushed him off, saying that he was not going to tell the 'federal feather merchants' because it was 'none of their business' and would 'muddy up the waters'." Click here for source.
What next for Dr. Bluestone?
Dr. Bluestone stated in his 2010 article that "The underlying pathogenesis of the Cavalier's ME disease is currently under investigation in our laboratory." He re-affirmed this disquieting news in his 2011 video, when he redundantly said "It's a current research project which we are undergoing now." Most recently, in February 2012, he stated:
"Another ongoing research project involves a potential animal model, Cavalier King Charles Spaniel, which has a greater than 50% incidence of chronic otitis media effusion.* Research being conducted with his colleagues in this animal involves histopathology of the middle-ear cleft in cadavers, and Eustachian tube function tests in live animals, conducted at the Ohio State University School of Veterinary Medicine in Columbus Ohio. "
* It seems he keeps increasing the percentage of incidence of PSOM in the breed, each time he makes a public comment, and this time, he has re-named the disorder "chronic otitis media effusion." So, apparently his new acronym for PSOM would be "COME"!
We can only pray that some wild hair will distract him from his focus on the cavalier King Charles spaniel. Otherwise, we will have to endure more of his ignorance, hopefully not on our tax dime.
RETURN TO TOP
March 14, 2012:
AKC's CHIC program is a farce for cavaliers
Don't be fooled by cavalier breeders who brag about CHIC
 The
American Kennel Club* (AKC) sponsors the
Canine
Health Information Center, also known as CHIC, with the stated mission "To
provide a source of health information for owners, breeders, and scientists,
that will assist in breeding healthy dogs." Unfortunately, for the cavalier King
Charles spaniel, CHIC not only does not work; it actually encourages bad
breeding practices and allows bad CKCS breeders to hide behind the CHIC "Good
Housekeeping" seal (see right).
The
American Kennel Club* (AKC) sponsors the
Canine
Health Information Center, also known as CHIC, with the stated mission "To
provide a source of health information for owners, breeders, and scientists,
that will assist in breeding healthy dogs." Unfortunately, for the cavalier King
Charles spaniel, CHIC not only does not work; it actually encourages bad
breeding practices and allows bad CKCS breeders to hide behind the CHIC "Good
Housekeeping" seal (see right).
*And its partners, the Canine Health Foundation (CHF) and the Orthopedic Foundation for Animals (OFA).
The two major genetic diseases affecting the cavalier King Charles spaniel are mitral valve disease (MVD) and syringomyelia (SM). Contrary to its "mission", CHIC provides absolutely no useful MVD or SM "health information ... that will assist in breeding healthy" cavaliers.
MVD is the leading killer of cavaliers. Statistics have repeatedly shown that over half of all cavaliers are expected to have MVD by their fifth birthday and nearly 100% by age ten years. SM is a spinal disorder which can cause excruciating pain. Statistics show that up to 25% of cavaliers may have SM by their first birthday and up to 70% by age 6 or older.
One would think that if AKC's CHIC program really wanted to "assist in breeding healthy" cavaliers, CHIC would recommend that breeders follow the breeding protocols* designed to reduce MVD and SM in future generations of cavalier puppies. Well, CHIC does nothing of the sort.
* Read the details of the MVD Breeding Protocol here, and the SM Breeding Protocol here.
Test for MVD? Yes ... but pass that test? Not necessarily!
As for MVD, all CHIC requires is that the breeding stock be examined by a veterinary cardiologist. It does not require that the results of the examination show no mitral valve disease. A cavalier of any age can be examined, flunk the exam, and still qualify for a CHIC certificate and be bred! See for yourself, from the CHIC policies webpage:
Syringomyelia? Never heard of it!
As for SM, CHIC has no requirements at all! As far as CHIC is concerned, syringomyelia is not a problem in the breed, and any cavalier may be bred without testing for it, much less found not to have it.
So, if a cavalier breeder brags to you about her dog having a CHIC certificate, tell her you know exactly what a CHIC certificate means, and most importantly, what it does not mean.
RETURN TO TOP
March 1, 2012:
Pedigree Dogs Exposed: The Sequel, or The End?
Most all cavalier breeders still refuse to get the message
 Pedigree Dogs Exposed was a televised investigatory documentary about the
British purebred dog scene. It was first broadcast in the United Kingdom in 2008
and then on PBS in the United States in 2009. Since then it has been available
on YouTube.
Pedigree Dogs Exposed was a televised investigatory documentary about the
British purebred dog scene. It was first broadcast in the United Kingdom in 2008
and then on PBS in the United States in 2009. Since then it has been available
on YouTube.
The program focused on a handful of dog breeds, but it had an enormous impact on the cavalier King Charles spaniel (CKCS) because it included video clips of cavaliers writhing in agonizing pain from syringomyelia (SM). (See photo below.) So, for many cavalier owners it was particularly eye-opening because, for the first time, many who viewed it were able to recognize similar symptoms of SM in their own pet cavaliers.
The program produced howls of protest from many corners of purebred dogdom, including over here in the US. The chairman of the American Kennel Club, Ron Menaker, referred to it as "sensationalist fiction and tabloid journalism masquerading as a documentary." But, he's an ignoramus. As far as the CKCS is concerned, every second of that program was factually accurate and needed to be publicized.
"From creation to ruination in less than 100 years"
 Earlier
this week, its sequel,
Pedigree Dogs Exposed -- Three Years On, was broadcast
in the UK. It, too, now is available periodically on YouTube. The cavalier remained a prime
topic in this sequel, and the conclusion to be drawn from it is that, with
early-onset mitral valve disease (MVD) -- nearly 100% affected by age 10 years
-- as well as syringomyelia -- over 70% affected -- it is time for pet buyers
to seriously avoid getting cavaliers. As the program's commentator put it,
"From
creation to ruination in less than 100 years." The rationale is that if the breeders
persist in refusing to follow the MVD breeding
protocol and SM breeding protocol, so as to
avoid producing future generations of only terminally ill cavaliers, then this breed should
come to an end.
Earlier
this week, its sequel,
Pedigree Dogs Exposed -- Three Years On, was broadcast
in the UK. It, too, now is available periodically on YouTube. The cavalier remained a prime
topic in this sequel, and the conclusion to be drawn from it is that, with
early-onset mitral valve disease (MVD) -- nearly 100% affected by age 10 years
-- as well as syringomyelia -- over 70% affected -- it is time for pet buyers
to seriously avoid getting cavaliers. As the program's commentator put it,
"From
creation to ruination in less than 100 years." The rationale is that if the breeders
persist in refusing to follow the MVD breeding
protocol and SM breeding protocol, so as to
avoid producing future generations of only terminally ill cavaliers, then this breed should
come to an end.
What has been the response of many cavalier breeders, to this sequel? Pretty much the same as to the 2008 broadcast: hostile condemnation. So, we are likely to see no progress on the breeding front. For the most part, the only people who "get" the truth are the pet buyers.
The likelihood of finding a cavalier puppy in the USA that either won't develop a heart murmur before its fifth birthday or won't have Chiari-like malformation and syringomyelia, is pretty much nill. Many US cavalier breeders have known about the MVD breeding protocol since 1998 and the SM breeding protocol since 2005, and yet most all of them have ignored both protocols.
For the rest of the US breeders, well they just don't even know about these real breeding protocols. In the US, there are two national breed clubs, one in the AKC and one out of it. Both of them refuse to recommend that their members follow either protocol. In fact, both of them recently have concocted their own phony MVD breeding protocols which no panel of cardiologists has ever approved, and neither club has even acknowledged the existence of the SM breeding protocol.
So, with breed clubs like those two, the CKCS appears to be on an unstoppable downward slide. The end result in the US probably will be generation after generation of sickly cavaliers, with high price tags and even higher veterinary and medicine bills. Surely that cannot go on very long. And then we will have none.
RETURN TO TOP
December 24, 2011:
Will the next SM breeding protocol be
BAD FOR THE BREED?
Breeding under age 2.5 years would increase early-onset MVD
 The
cavalier King Charles spaniel has TWO severe genetic
health disorders, NOT JUST ONE! While
syringomyelia (SM) is very
widespread in the breed, so is
mitral valve disease (MVD),
and it is MVD - not SM - that is the cavaliers' leading killer!
The
cavalier King Charles spaniel has TWO severe genetic
health disorders, NOT JUST ONE! While
syringomyelia (SM) is very
widespread in the breed, so is
mitral valve disease (MVD),
and it is MVD - not SM - that is the cavaliers' leading killer!
While the next SM Breeding Protocol, scheduled to be released in 2012 by the British Veterinary Association and the Kennel Club (BVA/KC), still is a work-in-progress, a preliminary draft of it (see below) would permit the breeding of cavaliers as young as 12 months old! If so, this certainly would violate the MVD Breeding Protocol, which sets the MINIMUM AGE for breeding cavaliers at 2.5 years of age.*
* A September 2010 statistical report has shown that anything less than following the MVD Breeding Protocol has not worked.

Have the new BVA/KC's SM protocol drafters forgotten about MVD? Are they giving CKCS breeders a deadly choice? Is the SM protocol really going to recommend that breeders ignore the MVD Breeding Protocol and thereby produce future generations of many more cavaliers which will die early, painful deaths from congestive heart failure?
Some background
It has been five years since the International Syringomyelia Conference issued its "Revised CKCS MRI Screening and Breeding Recommendations" in November 2006. The introduction to those breeding recommendations, also called the SM Breeding Protocol, stated:
"These breeding recommendations are made using current information and in response to CKCS breeder request for guidelines. It has yet to be proven if this guide is appropriate. The aim of these recommendations is to reduce the incidence of symptomatic syringomyelia (SM) in the breed, not to create litters of puppies guaranteed not to have SM as the chance of producing an affected dog cannot be predicted without knowing the inheritance."
The general principle of the 2006 guidelines is that dogs graded "Code A" are more desirable to use than those graded "Code B", and so on, but that dogs with a higher letter code may still be used in some limited circumstances.
Significantly, the protocol was predictively accurate. Statistics reported in October 2010 showed that:
• 75.9% of the offspring of matings of a Code A sire to a Code A dam were SM-clear.
• 41.9% of the offspring were SM-clear if only one parent was Code A.
• 0% of the offspring were SM-clear if neither parent was Code A.
Statistics reported a year later, October 2011, were similarly on target:
• 70% of the offspring of matings of a Code A sire to a Code A dam were SM-clear.
• 23% of the offspring were SM-clear if only one parent was Code A.
• 8% of the offspring were SM-clear if neither parent was Code A.
Still, much more has been learned about SM in the cavalier since the "current information" available to the International Syringomyelia Conference in 2006.
A June 2011 UK study of 555 cavaliers (Parker Report) showed that:
• 25% of 12 month old asymptomatic CKCSs had SM.
• 70% of asymptomatic CKCSs six years and older had SM.
These figures do not include SM-affected cavaliers which displayed symptoms, so, as the researchers concluded, "The true prevalence of syringomyelia in the general CKCS population is expected to be higher." They also concluded that, based upon their statistics, the minimum age of the SM Breeding Protocol ought to be raised from 2.5 years to 3.0 years, although they recognized that "many breeders would consider 36 months unduly old."*
*There is irony for you! The fact is that most cavalier breeders consider 2.0 years unduly old for initial matings.
In an October 2011 UK study (Knowler Report), the researchers go even farther. First, they concur with the Parker Report that "the optimum age for this early MRI screening is 36 months." Then, they recommend that, if only one of the breeding pair is SM-clear, it be "five years or older".
This is a matter of veterinary ethics!
So, with those two recent reports on the table urging raising the minimum breeding age to three or even five years, how can the BVA/KC possibly - even ethically - decrease that age from 2.5 years to one year?
The clear answer is that they should not! If the final, approved version of the new BVA/KC SM Breeding Protocol allows breeding any cavalier under the age of 2.5 years, then it will undercut the MVD Breeding Protocol, and it will be encouraging rampant early-onset MVD in the breed!
At the very least, the final version of the BVA/KC guidelines chart should change Age from "1-3" to "<3".
RETURN TO TOP
October 14, 2011:
What do the two USA CKCS clubs have against
breeding
healthy cavalier King Charles spaniels?
 The
syringomyelia (SM) breeding protocol works! (See the
October 2011 statistical report.) And, anything less than the
mitral valve
(MVD) breeding protocol has not worked! (See the
September 2010 statistical report.)
The
syringomyelia (SM) breeding protocol works! (See the
October 2011 statistical report.) And, anything less than the
mitral valve
(MVD) breeding protocol has not worked! (See the
September 2010 statistical report.)
BUT ... STILL ... neither of the USA cavalier King Charles spaniel clubs will recommend that their members follow either of these breeding guidelines.
 Why
don't these two breed clubs, the American Cavalier King Charles Spaniel
Club (ACKCSC), and the Cavalier King Charles Spaniel Club, USA (CKCSC,USA),
oppose SM and early-onset MVD in future generations of CKCSs?
Why
don't these two breed clubs, the American Cavalier King Charles Spaniel
Club (ACKCSC), and the Cavalier King Charles Spaniel Club, USA (CKCSC,USA),
oppose SM and early-onset MVD in future generations of CKCSs?
Why don't they endorse the MVD and SM breeding guidelines?
Ask their presidents. Call and email them.
The president of the ACKCSC is Patricia Kanan, telephone 805-688-7830, email torlundy@comcast.net
The president of the CKCSC,USA is Anne Eckersley, telephone 203- 616-5443, email ChadwickCavaliers@comcast.net
RETURN TO TOP
September 13, 2011:
A neurologist answers our August 13 questions:
"Okay syringomyelia researchers:
What now? Where do we go from here?"
 Lo and behold! For a moment there, I thought we might have had a definitive
answer to the query: "So, where do we go from here ...? Yo, researchers, do
you have any suggestions?" in our August 13
editorial.
Lo and behold! For a moment there, I thought we might have had a definitive
answer to the query: "So, where do we go from here ...? Yo, researchers, do
you have any suggestions?" in our August 13
editorial.
In the September 10, 2011 issue of the Veterinary Record, UK veterinary neurologist Rita Gonçalves wrote an editorial titled, "Understanding Chiari-like malformation: where are we now?"
"Ah ha", I thought! What wisdom does she have to impart? Well, not much, actually. After a brief but thorough and concise review of CM research in the cavalier King Charles spaniel, up through mid-2011, along with comparisons to the research of human Chiari malformation, Dr. Gonçalves reaches this painfully disappointing but quite obvious conclusion:
"Chiari-like malformation has for a decade now been widely identified in the CKCS population but despite its high prevalence, little is still known about its pathogenesis. Further studies are necessary to increase our understanding of this condition in order to allow the development of new treatment options and improve the welfare of the CKCS affected."
So, the answer essentially is that we need more money to continue the research, so that we can close in on the mysteries of the causes and solutions to CM and SM in our precious breed.
RETURN TO TOP
August 29, 2011:
Plucking the MVD genes:
The first shoe has dropped!
 The
headline of the September 2011 Journal of Heredity article says it all:
"Identification of 2 Loci associated with development of myxomatous mitral valve
disease in cavalier King Charles spaniels." Translation? It means that the
first step towards finding a DNA test for early-onset MVD genes has been taken.
The first shoe has dropped.
The
headline of the September 2011 Journal of Heredity article says it all:
"Identification of 2 Loci associated with development of myxomatous mitral valve
disease in cavalier King Charles spaniels." Translation? It means that the
first step towards finding a DNA test for early-onset MVD genes has been taken.
The first shoe has dropped.
Soon there should be a second shoe heard hitting the floor, when the researchers announce they've identified the actual genes themselves. In their report, they state:
"We will initiate studies of the most promising candidate genes in the 2 candidate regions which hopefully will lead us to the mutations affecting the development of mitral valve disease."
And then the thud of a third shoe (yes, we are talking about a triped here) will be felt when the researchers offer the DNA test to determine which cavaliers do or do not carry the offending genes.
That will be when the shoes hit the fan! For it has been well over a dozen years since the MVD breeding protocol was offered to cavalier breeders in the USA as the means of eliminating early-onset MVD in the breed. Since that announcement in 1998, nearly all of those "reputable", "responsible" cavalier breeders have declined, claiming that they would prefer to wait until the MVD genes are identified. Instead of trying to reduce MVD in their breeding stock, they chose to hide behind that excuse, and they continued to produce generation after generation of cavaliers with worse and worse early-onset MVD.
But now, those breeders' big bluff is about to be called. Soon enough, they will have what they claimed they've been waiting for. They claimed that they would not risk following the MVD breeding protocol because they feared that it would eliminate too much of their breeding stock. If they thought the MVD breeding protocol would have that much of an effect, just imagine what the DNA test will do to their bloodlines! It may wipe out entire kennels of breeding cavaliers!
So, it looks like they're going to have to come up with a new excuse for ignoring the DNA test. Start thinking hard now, you "reputable", "responsible" breeders. You don't have much time left!
RETURN TO TOP
August 18, 2011:
Will the CSF-space gap predict
future syringomyelia in cavaliers?
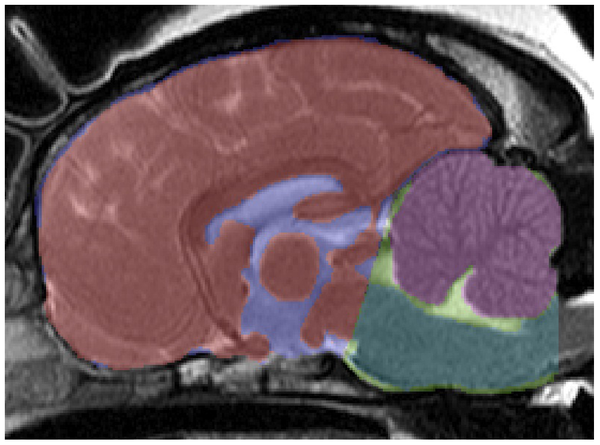 In
a recent research study of cavalier King Charles spaniels with
Chiari-like malformation (CM) and some with both CM and syringomyelia (SM),
the researchers reported:
In
a recent research study of cavalier King Charles spaniels with
Chiari-like malformation (CM) and some with both CM and syringomyelia (SM),
the researchers reported:
"When [cerebrospinal fluid] CSF space between the cerebellum and brainstem was compared in CKCS with and without SM, there was a significant increase in CSF space in CKCS with CM alone compared to those with CM/SM when head position was flexed. In their cine MR imaging study of CSF flow dynamics in CKCS with CM or CM/SM, Cerda-Gonzalez and others (2009a) found that turbulent CSF flow and jets are associated with SM presence and severity and CSF flow velocity at C2/3 is inversely related to the presence of SM. The reduced CSF space in CM/SM dogs reported in this study could explain this jet like CSF flow in dogs with CM/SM compared to those with CM alone."
Translation? We THINK it means that there is more space for cerebrospinal fluid (CSF) between the cerebellum and the brainstem of cavaliers with just CM than there is of cavaliers with both CM and SM.
Now, one of the current issues about CKCSs is that those younger ones with only CM still may develop SM as they age. Another recent study found that most cavaliers do not develop SM until after their third birthday and as late as age 6 years. Most all cavalier breeders believe that it is unreasonable to have to wait until their breeding stock is over 3 years old before being bred for the first time.
It would be a very valuable piece of information for any breeding program to be able to predict if a young cavalier (say, at age 18 or 24 months) will or will not ever develop syringomyelia.
This study may lead to the answer to the question: Can an MRI at an early age, showing the amount of CSF space between the cerebellum and the brainstem, predict whether the cavalier will or will not end up with SM?
RETURN TO TOP
August 13, 2011:
Okay, syringomyelia researchers:
What now? Where do we go from here?
 HERE IS THE SITUATION: In June, a team of veterinary
neurologists issued
a
devastating report. They examined the MRI scans of 555 cavalier King Charles
spaniels, and found that at age 12 months, 25% had syringomyelia (SM), and by
age six years, 70% had SM. And, all 555 of these were cavaliers which reportedly
had no symptoms of SM.
HERE IS THE SITUATION: In June, a team of veterinary
neurologists issued
a
devastating report. They examined the MRI scans of 555 cavalier King Charles
spaniels, and found that at age 12 months, 25% had syringomyelia (SM), and by
age six years, 70% had SM. And, all 555 of these were cavaliers which reportedly
had no symptoms of SM.
THINK OF IT: Not only did 25% of these cavaliers already have SM by their first birthday, but in the five years between age 1 and age 6, 45% of the rest of the cavaliers acquired SM.
Previously, these neurologists thought that most dogs afflicted with SM would start to show symptoms before age 3 years. When the International Syringomyelia Conference issued its revised CKCS MRI screening and breeding recommendations in 2006, the panel of researchers stated:
"The age cut off at 2.5 years has been decided so as to tie in with MVD recommendations and because most dogs with symptomatic SM will show signs before 3 years of age."
That cut off age meant that cavaliers at least 2.5 years old without SM would be classified as Code "A" and could be mated with any other cavaliers over 2.5 years, even if they had asymptomatic SM.
Now, we find, most cavaliers do not even contract SM until after they are 3 years old, much less also become symptomatic.
The authors of the June 2011 report, J. E. Parker, S. P. Knowler, C. Rusbridge, E. Noorman, and N. D. Jeffery, carefully worded the serious impact of these findings upon the current SM breeding protocol:
"The evidence for a lower prevalence in younger animals is more reliable ... and this effect lasts until dogs are at least three years of age. This finding has important implications for the design of a screening test procedure and may conflict with the current recommendations that the optimum age for screening should be 30 months. These data would imply that it is probable that dogs aged up to three years may yet have reduced odds for the diagnosis of syringomyelia. However, there is a need for the dogs to be screened when they are reasonably young so that breeders can decide at an early stage whether their animals are suitable for breeding; many breeders would consider 36 months unduly old."
GET IT? This means that more cavaliers develop SM after age 2.5 years than before that age. So, the current SM breeding protocol is ineffective. But, they also observe that breeders would not consider waiting until their MRI-clear cavaliers are 3 years old ("unduly old"). Thus the dilemma in which we CKCS fanciers find ourselves.
WHAT TO DO? WHAT TO DO? Well, the researchers don't give us much hope. They go on:
"The high lifetime prevalence of syringomyelia raises concerns for the welfare of the CKCS breed and also suggests that eliminating the genetic risk factors for the disease by selective breeding may be difficult, because the heritability has previously been shown to be complex ... and the prevalence of the determinant genes within the population is therefore likely to be high. The true prevalence of syringomyelia in the general CKCS population is expected to be higher than that found in this sample population because symptomatic dogs were specifically excluded."
RAISES CONCERNS!!! To say the least! MAY BE DIFFICULT!!! What an understatement! We now know that SM is far more widespread in the breed than anyone, even the experts, ever thought. We now know that the 2.5 year cut off in the SM breeding protocol is way too early, but that many breeders would not stand for extending that age by even another six months.
(Actually, the dirty little secret is that nearly all US cavalier breeders always have been ignoring the current SM breeding protocol. Neither of the two CKCS national clubs in the US will even acknowledge that the breeding protocol exists, much less recommend that breeders follow it.)
So, where do we go from here, cavalier fanciers? Yo, researchers, do you have any suggestions?
RETURN TO TOP
July 24, 2011:
AKC's chairman Ron Menaker condemns
"Pedigree Dogs Exposed"
Then reinserts his head firmly back underground
 Is
this any way to lead the American Kennel Club through the genetic morass it is
facing? On July 19, the chairman of the board of the American Kennel Club, Ron Menaker, signed a petition to the UK's Parliament to prevent the
British Broadcasting Company from broadcasting a sequel to
"Pedigree Dogs Exposed" (PDE), the 2008 BBC documentary which has turned the
British purebred dog world upside-down.
Is
this any way to lead the American Kennel Club through the genetic morass it is
facing? On July 19, the chairman of the board of the American Kennel Club, Ron Menaker, signed a petition to the UK's Parliament to prevent the
British Broadcasting Company from broadcasting a sequel to
"Pedigree Dogs Exposed" (PDE), the 2008 BBC documentary which has turned the
British purebred dog world upside-down.
Chairman Menaker did not stop at just adding his name to the petition to Parliament. He also wrote:
"Responsible dog owners, the dog loving public and responsible dog breeders should not be subjected to another piece of sensationalist fiction and tabloid journalism masquerading as a documentary. Any investigation of dogs, breeding or health matters should be balanced and fair. If the BBC insists on repeating this exercise in media sensationalism, why not present the truth about the progress that has been made as a result of responsible dog breeding and scientific research projects funded by organizations that truly care about dogs. For the BBC's next installment, how about 'Jemima Harrison Exposed'?"
Thus, the AKC chairman wants UK's Parliament to both ban the BBC from broadcasting its upcoming PDE-2, and to force the BBC to present an expose of PDE's producer, Jemima Harrison. Putting aside all of the anti-Freedoms of Speech and Press and censorship aspects of AKC Chairman Menaker's comments, it is jaw-dropping that the highest ranking officer of the American Kennel Club would wage so public and vicious an attack against PDE and its producer, just as that same producer is putting together the sequel which Mr. Menaker so desperately seems to want to prevent.
Hullo, Mr. Menaker? Can you spell "Good Public Relations"?
 One of the reasons PDE has had such a dramatic impact upon the British
pedigree dog world since 2008 is that the UK Kennel Club and its breed clubs,
including the UK's cavalier King Charles spaniel club, refused to substantively
cooperate during its production. CKCS club members literally turned their backs
on PDE's cameraman. But even those UK clubs had enough savvy to not publicly and
personally lash out at Ms. Harrison, its producer.
One of the reasons PDE has had such a dramatic impact upon the British
pedigree dog world since 2008 is that the UK Kennel Club and its breed clubs,
including the UK's cavalier King Charles spaniel club, refused to substantively
cooperate during its production. CKCS club members literally turned their backs
on PDE's cameraman. But even those UK clubs had enough savvy to not publicly and
personally lash out at Ms. Harrison, its producer.
On the one hand, AKC Chairman Menaker attacks PDE and it's producer for not being "balanced and fair", and yet on the other hand, instead of offering information to help make PDE-2 more balanced and fair, he wants the British government to ban it! And investigate its producer, to boot! His head-in-the-sand approach is not going to work for the AKC, and if Chairman Menaker is not careful, soon Ms. Harrison may cross the pond to produce PDE-3, and re-pay him for his courtesies.
RETURN TO TOP
June 13, 2011:
How the syringomyelia breeding protocol
could lead to the Popular Sire Syndrome
Many "D" bitches mated with the same "A"
stud =
another
genetic crisis for the CKCS
 For corner-cutting breeders of cavalier King Charles spaniels, trying to
follow the syringomyelia (SM) breeding protocol could lead to a uprising of the
dreaded Popular Sire Syndrome*.
For corner-cutting breeders of cavalier King Charles spaniels, trying to
follow the syringomyelia (SM) breeding protocol could lead to a uprising of the
dreaded Popular Sire Syndrome*.
*A Popular Sire has been defined in canine research papers as having produced more than 100 offspring.
The current SM breeding protocol, introduced to the cavalier King Charles spaniel community in 2006 by the International Syringomyelia Conference, only requires that one of a breeding pair of cavaliers not have syringomyelia. The other cavalier of that pair may either have syringomyelia but without any symptoms - according to its magnetic resonance imaging (MRI) scan - or it may not even have been MRI scanned at all.
Specifically, the protocol provides that a dog classified as an "A" must be over 2.5 years of age and that SM is "absent or less than 2mm central canal dilatation in the C2-C4 region only". A "D" cavalier is one which is over 2.5 years and diagnosed by MRI to have "asymptomatic" SM, meaning that the dog has the disease but does not act like it does. That is one way a cavalier may be classified as a "D". The other way is to be over 2.5 years but to not be MRI scanned at all. So, as long as the dog is over 2.5 years and does not behave like it is suffering from SM, it is a "D" dog. This is known as a "default D" dog.
Most cavalier breeders have more female breeding stock than males. Having too many - in some cases even just one - intact males around can cause more problems than the males are worth. So, most cavalier breeders who do not rely much upon line breeding, will hire other breeders' studs for mating, rather than keep the dogs in their own households with all those bitches around.
When a financially-challenged CKCS breeder with, say, a half dozen bitches as her breeding stock, considers the SM breeding protocol, she finds that MRI scanning can be quite costly. One thorough scan for just one bitch can cost thousands of dollars, when the ancillary procedures are taken into account, such as blood tests, anesthesia, radiologist and neurologist fees, transportation, etc. Multiply that cost by the number of bitches in the breeder's kennel, and then maybe double that figure, since more than one MRI scan could be necessary during the breeding years for each bitch. Dealing with just this one protocol for this one genetic disorder could wipe out any hopes of the breeder breaking even on the litters all of her bitches could be hoped to produce.
An apparent solution to this breeder's dilemma is the option under the SM protocol to not scan her breeding stock at all. If they don't have symptoms of SM, then she can call all of them "D"s, hence the term, "default D". And if she can find a sire which has been MRI scanned and classified an "A", she could use that sire on all of her "default D"s and still satisfy the SM protocol.
But what about using that one "A" sire on so many "D" bitches? And what about all the other cavalier breeders who decide to take the same approach and also use that "A" male on all of their "D" bitches?
That would be a classic case of Popular Sire Syndrome (PSS). Yes, the current SM breeding protocol encourages corner-cutting breeders, with "default D" bitches, to use the same limited pool of sires, called "Popular Sires", in this case "popular" because they are among a very limited number of "A" dogs.
The PSS is believed to be one of the main causes for the spread of genetic disorders in any breed. As a result, geneticists have urged all breeders to avoid using the same dog for mating all or most of their own breeding stock, and also to avoid using the same sires that several other breeders have been using. Even the owners of the sires themselves have been urged to limit the usage of their dogs by breeders.
Cavalier breeders should not take the short-cut of calling their unscanned bitches "D" (for default), and then breeding them to the same "A" male, to satisfy the SM breeding protocol. But, if past history is a guide, many of corner-cutting cavalier breeders will do just that, and the CKCS community will face another genetic crisis soon enough, thanks to another round of the Popular Sire Syndrome.
RETURN TO TOP
May 11, 2011:
CKCSC,USA's board admits Its ignorance
...
but not its stupidity!
 After repeated denials, the CKCSC,USA's current board of directors finally
admitted that its 1998 predecessor board really did endorse
the real MVD Breeding Protocol. In the official minutes of the board's October 14, 2010 meeting, it
says:
After repeated denials, the CKCSC,USA's current board of directors finally
admitted that its 1998 predecessor board really did endorse
the real MVD Breeding Protocol. In the official minutes of the board's October 14, 2010 meeting, it
says:
"In response to numerous inquiries and comments regarding the guidelines adopted by the CKCSC-USA, David Frederick clarified that guidelines are not medical protocols. The protocol suggested by a cardiology symposium held in conjunction with the 1997 [really was in 1998] National Specialty specified 2.5 years as the minimum age for first time breeding of dogs and bitches. This protocol was endorsed by an earlier Board." (Emphasis added, of course.)
So, there you have it. The current CKCSC,USA board admits that it was wrong when it claimed that its April 2010 breeding recommendations were "historic" and that "none had existed before"*. Unfortunately, what it did not do at its October 2010 meeting is re-instate the real, one-and-only MVD Breeding Protocol, which this current board un-ceremoniously dumped at its April 2010 meeting. Read "CKCSC,USA Dumps MVD Breeding Protocol" for those details.
The current CKCSC,USA board still endorses only a worthless breeding guideline which no panels of cardiologists or geneticists researchers have ever recommended, and which, they have told us, has not worked and would not work! Stupidity and callous disregard for the hearts of future generations of cavaliers still reign at the Cavalier King Charles Spaniel Club, USA!
*Interestingly, one of the current board members was also on the 1998 board which unanimously endorsed the real MVD protocol. Notwithstanding her inexplicable memory lapse, she now can say that she voted for it before she voted against it!
RETURN TO TOP
April 23, 2011:
Beware the pimobendan/Vetmedin "EPIC clinical trial":
There is no upside
If your cavalier is in it, PULL OUT!
 There comes a time when owners of cavalier King Charles spaniels must say
"NO!" to participating in a pharmaceutical company's study of its proprietary
brand wonder drug. The on-going "EPIC Clinical Trial" of pimobendan is a prime
example. EPIC is being sponsored by its developer, Boehringer Ingelheim GmbH, a
German pharmaceutical company, which markets the drug under the registered brand
name "Vetmedin".
There comes a time when owners of cavalier King Charles spaniels must say
"NO!" to participating in a pharmaceutical company's study of its proprietary
brand wonder drug. The on-going "EPIC Clinical Trial" of pimobendan is a prime
example. EPIC is being sponsored by its developer, Boehringer Ingelheim GmbH, a
German pharmaceutical company, which markets the drug under the registered brand
name "Vetmedin".
Background of pimobendan
Cavalier King Charles spaniels suffering from mitral valve disease (MVD) and in the late stage of congestive heart failure (CHF), often are prescribed pimobendan. This drug has been shown to improve the quality of life for dogs suffering from CHF due to MVD. It can be very effective at increasing the strength of the heart muscle contractions, thereby improving the heart's efficiency to function as a pump, and increasing the blood flow to major organs. It even has been shown, in some studies, to actually reduce the amount of backflow of blood through the mitral valve and reverse the enlargement of the heart chambers.
But, there also can be negative aspects to pimobendan. It can have life-threatening (or worse) side-effects when prescribed for asymptomatic dogs or to dogs which, even though they have enlarged hearts and are in CHF, also still have strong heart muscles and good contractility. For those dogs, pimobendan has over-increased their hearts' pumping ability and contractility to the extent that their mitral valves' major chordae tendineae have been overworked and, in some cases, have actually ruptured, causing immediate death. (Click here for summary of three disturbing research reports about the inappropriate administration of pimobendan to dogs not in CHF, and a dire warning from Vetmedin's manufacturer itself.)
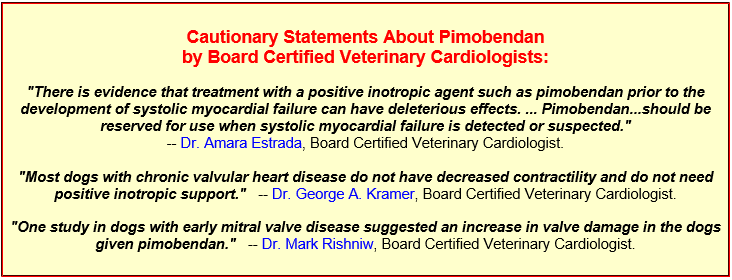
 The U.S. Food and Drug Administration's (FDA)
2007 report approving the use of pimobendan for dogs also contained the
warning that the drug not be prescribed by dogs which are not
in congestive heart failure. On each container of Vetmedin is the warning that "Vetmedin
should not be given in cases ... where an augmentation of cardiac output is
inappropriate for functional or anatomical reasons. Warnings: Only for use in
dogs with clinical evidence of heart failure." (Click here to read more about pimobendan and its downsides.)
The U.S. Food and Drug Administration's (FDA)
2007 report approving the use of pimobendan for dogs also contained the
warning that the drug not be prescribed by dogs which are not
in congestive heart failure. On each container of Vetmedin is the warning that "Vetmedin
should not be given in cases ... where an augmentation of cardiac output is
inappropriate for functional or anatomical reasons. Warnings: Only for use in
dogs with clinical evidence of heart failure." (Click here to read more about pimobendan and its downsides.)
The bad news EPIC trial
Pimobendan's manufacturer's EPIC Clinical Trial has no upside for cavaliers. The trial's criteria are that cavaliers with some heart enlargement due to MVD but which do not have any clinical signs and are not in CHF, are to be given twice-daily doses of either pimobendan or a worthless placebo and nothing else. This daily medication (or placebo) is intended to go on until the dog develops heart failure.
We already know, from the extensive studies relied upon by the FDA in its approval report, that pimobendan should not be prescribed to dogs if they are not in CHF. Even the EPIC Trial's own website contains this pointed reason to not prescribe pimobendan at such an early stage. It states:
"In the recently published ACVIM Consensus Statement, there is no treatment recommendation for dogs in this stage of heart disease."
We also know that treating a progressive disorder like MVD with only a worthless placebo -- and nothing but a worthless placebo -- until heart failure results, can be an extremely risky protocol for any cavalier. It would be irresponsible of the cavalier's owner and its cardiologist.
So, much like Hobson's choice, you can allow your cavalier to risk pre-mature death due to being given pimobendan when it could do more harm than good, or you can allow your cavalier to not be treated with anything at all until it develops heart failure.
Just say NO!
 Occasionally, or perhaps even more often than that, pharmaceutical companies'
motivations to sell their products tend to outweigh the ethical prudence they
should display to not encourage inappropriate marketing. We are not suggesting
that this manufacturer's current EPIC Clinical Trial is such a marketing ploy.
But knowing what we do know about the lethal dangers of prescribing pimobendan
to cavaliers too early in the progression of their MVD, or to cavaliers
even in congestive heart failure but still with strong contractility,
this is a potentially terribly flawed study, and cavalier owners should not allow their dogs
to participate in
it.
Occasionally, or perhaps even more often than that, pharmaceutical companies'
motivations to sell their products tend to outweigh the ethical prudence they
should display to not encourage inappropriate marketing. We are not suggesting
that this manufacturer's current EPIC Clinical Trial is such a marketing ploy.
But knowing what we do know about the lethal dangers of prescribing pimobendan
to cavaliers too early in the progression of their MVD, or to cavaliers
even in congestive heart failure but still with strong contractility,
this is a potentially terribly flawed study, and cavalier owners should not allow their dogs
to participate in
it.
Research Report Summaries:
In "Comparative adverse cardiac effects of pimobendan and benazepril monotherapy in dogs with mild degenerative mitral valve disease: a prospective, controlled, blinded, and randomized study", published in 2007 in the Journal of Veterinary Internal Medicine, the researchers found that "PIMO has adver se cardiac functional and morphologic effects in dogs with asymptomatic MVD."
In "Increased Mitral Valve Regurgitation and Myocardial Hypertrophy in Two Dogs With Long-Term Pimobendan Therapy", published in 2005 in Cardiovascular Toxicology, the researchers concluded "This is the first report to describe an increase in mitral regurgitation under clinical conditions in dogs treated with pimobendan. We also suggest that pimobendan may induce ventricular hypertrophy."
In Cardiac Care for Pets' (CVCA) "Pimobendan- A Silver Bullet?", published in May 2009, the cardiology department stated: "In a small study performed by CVCA, it was determined that after two to three weeks of Pimobendan therapy about 75% of dogs had an increased frequency of ventricular arrhythmias documented on 24 hour ambulatory ECG monitoring."
In the U.S. Food and Drug Administration's (FDA) 2007 report approving the use of pimobendan for dogs, it stated this conclusion in a four week toxicity study of pimobendan administered to 30 previously healthy lab Beagles: "Conclusions: Pimobendan administered IV daily to healthy Beagles caused dose dependent increases in heart rate, mitral valve myxomatous thickening, left ventricular outflow tract endocardial thickening, and ventricular muscle ischemic lesions (multifocal subendocardial necrosis and scarring). The cardiac pathology seen in these dogs is typical of positive inotropic drug toxicity in normal dog hearts, and is related to the physiologic effect of the drug on contractility and exaggerated hemodynamic response."
On Vetmedin's website, it has this warning: "The safety of VETMEDIN has not been established in dogs with asymptomatic heart disease."
RETURN TO TOP
January 30, 2011:
Chiari-like malformation HAS been re-defined!
 Our
January 28, 2011 editorial, "Maybe Cavaliers Don't
Even Have Chiari-Like Malformation (CM)!", pointed out that, in
view of recent research reports, either cavalier King Charles spaniels do not
have CM ("decreased caudal fossa volume") or CM needs to be re-defined to fit
within these current research findings.
Our
January 28, 2011 editorial, "Maybe Cavaliers Don't
Even Have Chiari-Like Malformation (CM)!", pointed out that, in
view of recent research reports, either cavalier King Charles spaniels do not
have CM ("decreased caudal fossa volume") or CM needs to be re-defined to fit
within these current research findings.
Well, apparently CM has been re-defined! On the website of syringomyelia researcher Dr. Clare Rusbridge, CM now is defined as "a condition characterized by a mismatch in size between the brain (too big) and the skull (too small). There is not enough room for the brain and the back part (cerebellum and medulla) is pushed out the foramen magnum." The foramen magnum is a hole in the back of the skull -- in the occipital bone -- leading to the spinal cord. Dr. Rusbridge goes on to explain that the cavalier appears to have a brain more appropriate for a bigger dog.
This new definition of Chiari-like malformation pretty much neutralizes the point of our January 28 editorial, so in the inimitable words of Saturday Night Live's Gilda Radner's character, Emily Litella, "Never mind!"
RETURN TO TOP
January 28, 2011:
Maybe cavaliers don't even have
Chiari-like malformation (CM)!
 It may be time to let Chiari-like malformation (CM) off the hook! For many
moons, CM has been tagged as the "usual suspect" in the blame-game for a cause
of syringomyelia (SM) in the cavalier King Charles spaniel (CKCS). But based
upon recent studies, it looks like cavaliers do not even have CM!
It may be time to let Chiari-like malformation (CM) off the hook! For many
moons, CM has been tagged as the "usual suspect" in the blame-game for a cause
of syringomyelia (SM) in the cavalier King Charles spaniel (CKCS). But based
upon recent studies, it looks like cavaliers do not even have CM!
CM is defined as, "decreased caudal fossa volume with caudal descent of the cerebellum, and often the brainstem, into or though the foramen magnum." The caudal fossa is the cavity within the hind portion of the skull, also known as the occipital bone. The occipital bone contains the foramen magnum, which is the hole at the base of the skull.
The implication has been that the smaller caudal fossa volume within the occipital bone would force the cerebellum (the hindbrain) to squeeze through that hole, the foramen magnum, causing excessive pressure on the cerebrospinal fluid (CSF) and resulting in the production of a syrinx. The conclusion was that it was the smaller size of the hind-skull that was to blame for that squeeze play and the consequent syrinxes.
However, three veterinary research journal articles published in 2009 and 2010 point to evidence that cavaliers' hind-skull volumes are not different from other small breeds, particularly those with short muzzles, and that the percentage of the volume of the caudal fossa to the volume of the total cranial cavity did not differ significantly between CKCSs with and without SM.
Instead, the oversized cerebellum may be the culprit. These studies also found that the volume of hindbrain was significantly greater for young -- 2-years and younger -- cavaliers with SM than older dogs -- 5 years and older -- without SM. They also found that increased hindbrain volume in CKCSs with SM, compared to that of the hind-skull, was directly correlated with the size of the dogs' syrinxes.
If the 2009 and 2010 studies are on the right track, then we may have to either re-define "Chiari-like malformation" or use another term to describe the disorder, since the "malformation" may not be of the skull, but of the brain. A re-definition could be "increased cerebellar parenchyma volume with caudal descent of the cerebellum, and often the brainstem, into or though the foramen magnum." But then, would that really be "Chiari-like", or just some other type of malformation?
So, indeed, the SM cavalier's brain may be too large for its skull!
RETURN TO TOP
December 28, 2010:
CKCSC,USA's board reinstates a third of
the REAL MVD breeding protocol
 In our October 7 Editorial, we
called upon the CKCSC,USA's board of directors to reinstate the REAL
mitral valve disease breeding protocol at their October meeting. Well,
apparently they did a third of that. Recall, if you will, that at their
April 2010 meeting, they dumped the real protocol, which their
predecessors had unanimously approved in May 1998 when the protocol was
introduced. See our September 7 Editorial
("CKCSC,USA Dumps MVD Breeding Protocol") politely pointing out their act of
virtual insanity.
In our October 7 Editorial, we
called upon the CKCSC,USA's board of directors to reinstate the REAL
mitral valve disease breeding protocol at their October meeting. Well,
apparently they did a third of that. Recall, if you will, that at their
April 2010 meeting, they dumped the real protocol, which their
predecessors had unanimously approved in May 1998 when the protocol was
introduced. See our September 7 Editorial
("CKCSC,USA Dumps MVD Breeding Protocol") politely pointing out their act of
virtual insanity.
In April, the current board replaced the REAL protocol with an odious, worthless version, in which they stated: "The CKCSC,USA recommends that prior to breeding any Cavalier, the dog have a clear rating at two years of age from an auscultation by a board certified veterinary cardiologist."
In the face of an onslaught of justifiable criticism, the board met in October and tweaked their bogus breeding recommendation thusly:
"The CKCSC,USA recommends that prior to breeding any Cavalier, the dog should have a heart clearance from an auscultation by a board certified veterinary cardiologist that is consistent with prevailing cardiology protocols; however, the CKCSC,USA recommends a minimum of a cardiology clearance at age 2.5 years by a board certified cardiologist."
Say what??? I suppose we should be grateful for whatever crumbs the board chooses to throw our way, but really!!! This October revision is only a miniscule improvement over their April abomination, and the bottom line is that, according to the researchers, it is still worthless. After all, whatever the CKCSC,USA board "recommends" is toothless at best. No breeders are bound by it, so why doesn't the board go all the way and actually reinstate the REAL MVD protocol that the Club stood by for the past twelve years until this board came along?
Why not add the other two-thirds of the REAL protocol?
• Do not breed any Cavalier under the age of 5 years, unless its parents' hearts were free of MVD murmurs by age 5 years.
• Do not breed any Cavalier who is diagnosed with an MVD murmur under the age of 5 years.
Come On, CKCSC,USA Board: MAN UP!!! Show the world that your Club really does take early-onset MVD seriously, instead of showing your incredible pride and your heinous contempt for future generations of Cavalier King Charles spaniels.
RETURN TO TOP
October 7, 2010:
To CKCSC,USA's board:
Reinstate the REAL MVD breeding protocol!
 Dear CKCSC,USA board of directors: Your next board meeting on
October 14 is your chance to redeem yourselves. Reinstate the
REAL
MVD Breeding Protocol!
Dear CKCSC,USA board of directors: Your next board meeting on
October 14 is your chance to redeem yourselves. Reinstate the
REAL
MVD Breeding Protocol!
The Club's 1998 board wisely endorsed the REAL protocol which the international research panel of heart specialists and geneticist drew up and urged all cavalier King Charles spaniel breeders to follow, at a minimum! They told us at the Club's MVD Symposium in May 1998 that we could eliminate early-onset MVD in just a few generations if enough breeders faithfully followed it. Since then, we know that only a handful of cavalier breeders ever paid any attention to it, so twelve years after 1998, there has been no progress in ridding the breed of young cavaliers with bad hearts, suffering and dying all too soon. But that was no excuse for you to dump the REAL protocol at your April 2010 meeting!
In April, you had your chance to re-new the endorsement and urge all club members to follow the REAL protocol. Instead, you replaced it with a worthless recommendation to breed cavaliers "clear at 24 months", which no cardiologist or geneticist researcher has ever recommended. In fact, they told us in 1998 that breeding "clear-to-clear" has not worked and would not work!
You have ignored the research experts' conclusions that, at a minimum:
(A) All four parents of the breeding pair be MVD-clear as of
their 5th birthday;
(B) The breeding pair be at least 30 months old and MVD-clear at the
time of breeding; and
(C) No cavalier be bred if diagnosed with an MVD murmur before its fifth
birthday.
Just last month, Sweden's Dr. Clarence Kvart reported that the Swedish CKCS club's "clear at 24 months" protocol has not reduced the percentage of cavaliers having MVD, and as a result, the Swedish club is considering making the REAL protocol mandatory!
Whatever your purpose in rejecting the REAL protocol, now is your opportunity to redeem yourselves. You owe it to the future generations of cavaliers. Remember, the next edition of Pedigreed Dogs Exposed is focusing on you!
RETURN TO TOP
September 10, 2010:
How self-absorbed can the CKCSC,USA board be?
 Now, after the editorial
CKCSC,USA dumps MVD breeding protocol first appeared
on September 7, the CKCSC,USA has added to its website an introduction to the
announcement of the board's April 29, 2010 decision to reject its 1998
endorsement of the
MVD breeding protocol. The introduction falsely
states:
Now, after the editorial
CKCSC,USA dumps MVD breeding protocol first appeared
on September 7, the CKCSC,USA has added to its website an introduction to the
announcement of the board's April 29, 2010 decision to reject its 1998
endorsement of the
MVD breeding protocol. The introduction falsely
states:
"The Board took a historic step and established minimal recommendations for conducting health tests ... where none had existed before."
This is a very odd attempt to revise the club's history. The club's 1998 endorsement of the MVD breeding protocol was indeed "historic". The only thing which is historic about the board's April 2010 decision is that it has replaced the MVD breeding protocol with a worthless "clear at 24 months" recommendation, which the research experts told the club back in 1998 would not work.
In the face of the laser now shining brightly and critically upon the cavalier King Charles spaniel, beginning with the broadcast of Pedigree Dogs Exposed, one would expect the CKCSC,USA's board to take a giant step forward and, at the very least, re-new its recommendation of the MVD breeding protocol, if not make it mandatory for registering litters. Instead, the board in April of this year has pretended that it never had recommended the protocol at all, and then replaced it with nonsense. Why does the board now deny that it approved the MVD breeding protocol in 1998?
RETURN TO TOP
September 7, 2010:
CKCSC,USA dumps the MVD breeding protocol
 Taking a giant step backwards from its May 1998 decision endorsing the
MVD breeding protocol, the board of directors of
the Cavalier King Charles Spaniel Club, USA rejected that protocol at its April
2010 meeting. Instead, its board approved a watered down, proven worthless "recommended guideline",
calling for the breeding pair to have MVD-murmur-clear hearts at only 24 months.
Taking a giant step backwards from its May 1998 decision endorsing the
MVD breeding protocol, the board of directors of
the Cavalier King Charles Spaniel Club, USA rejected that protocol at its April
2010 meeting. Instead, its board approved a watered down, proven worthless "recommended guideline",
calling for the breeding pair to have MVD-murmur-clear hearts at only 24 months.
It has been twelve years since the CKCSC,USA sponsored the "International Symposium on Chronic Cardiac Valve Disease (CVD) in the Cavalier King Charles Spaniel" in Atlanta, Georgia in May 1998. The club invited a panel of veterinary cardiologists from the USA and the UK -- Drs. Andrew Beardow, James Buchanan, Virginia Luis Fuentes, and Bruce Keene -- and the renowned canine geneticist, Lennart Swenson from Sweden. Before a packed theater of club members, the panel reported on the severity of the disease and its pervasiveness throughout the breed. They stated these conclusions:
• MVD is the leading cause of death in Cavaliers;
• It is a hereditary, genetic disorder;
• There has been no statistical improvement in Cavaliers' mitral valves in the eleven years since the first studies; and
• The disease can be decreased and the age of onset delayed by following guidelines of only breeding Cavaliers who are over the age of 2.5 years, have hearts free from MVD murmurs, and have parents whose hearts were MVD murmur-free at age 5 years. No Cavaliers should be bred which have murmurs before age 5 years.
The panelists then introduced:
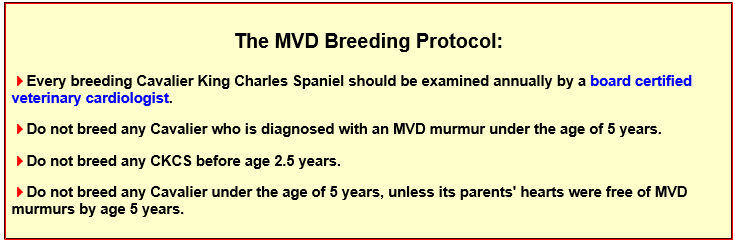
That same weekend in May 1998, the CKCSC,USA's board endorsed the protocol and then sent a verbatim transcript of the symposium to all club members, with this statement:
"In this 'Year of the Heart' in which the CKCSC,USA is instituting a number of programs geared toward the study and control of chronic cardiac valve disease, this symposium was organized to bring together international experts to present data and provide guidelines for breeders.
"We urge our members to follow their recommendations, and hope that we will attain our goal of bringing the prevalence, the age of onset, and the severity of the disease to the levels seen in other breeds of dogs."
The Club also mailed to its members annually, beginning in 1998, a Health Registry booklet, which included this set of MVD breeding guidelines:
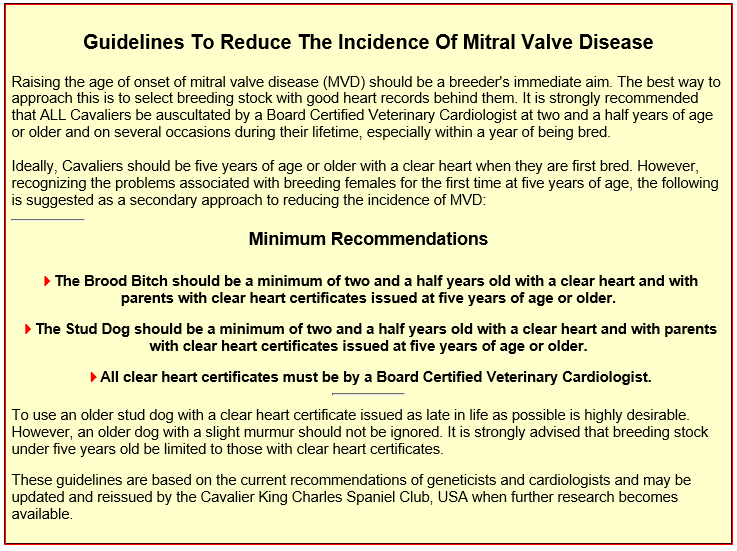
Even with these strong endorsements, only a handful of cavalier breeders have faithfully followed the MVD breeding protocol. As evidence of that lack of participation, in March 2009, eleven years after the protocol was introduced, cardiologist Simon Swift stated: "In the UK and the USA, about ½ of all cavaliers [still] have a murmur by the time they are 5 years old."
Purebred breed clubs -- of which indeed the CKCSC,USA is one -- are obliged to educate breed owners on the nuances of the breed and oversee the breed's health and welfare. The leadership of breed clubs owe a fiduciary duty, not to the club's breeders, but to the breed, to assure that the dogs are protected from irresponsible breeding practices and from the creation of future litters of genetically damaged puppies. Since most all cavalier breeders in the club have failed to faithfully follow the MVD breeding protocol these past twelve years, the responsible thing for its board to do, to protect the breed, would be to re-affirm the importance that its breeders comply with the protocol.
But now we find, twelve years after endorsing the MVD breeding protocol, that instead of doing that responsible thing, the CKCSC,USA board has dumped it and instead has contrived this totally bogus guideline which has been proven to be a failure:
"The CKCSC,USA recommends that prior to breeding any Cavalier, the dog have 1) a clear rating at two years of age from an auscultation by a board certified veterinary cardiologist; ..."
This new worthless guideline ignores the research experts' conclusions that: (A) All four parents of the breeding pair be MVD-clear as of their 5th birthday; (B) The breeding pair be at least 30 months old and MVD-clear at the time of breeding; and (C) No cavalier be bred if diagnosed with an MVD murmur before its fifth birthday.
Sadly, the Club's board has effectively thumbed its collective nose at the heart-health of all future generations of CKCSC,USA cavalier King Charles spaniels.




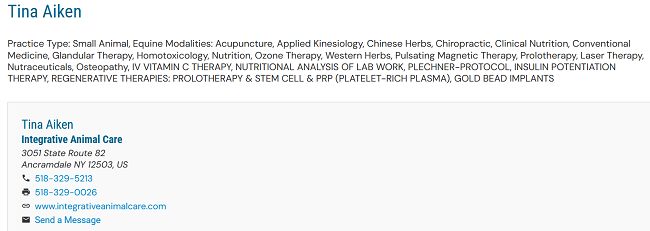
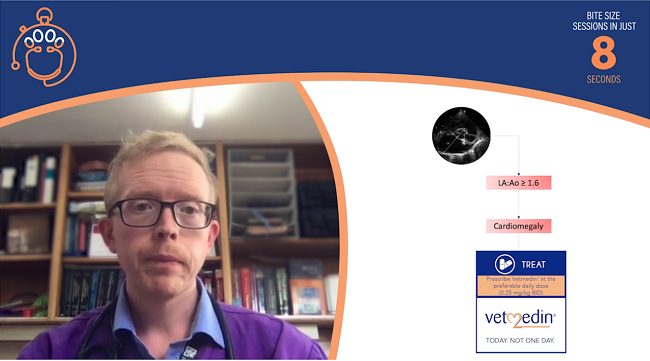

CONNECT WITH US